Epidermodysplasia verruciformis (EV) is a rare autosomal recessive genodermatosis characterized by a defect in cell-mediated immunity and increased susceptibility to infections by group B human papillomavirus (HPV).1,2 Its main clinical features are a rash resembling pityriasis versicolor and flat warts distributed in sun-exposed areas. In the last decade, several cases of acquired EV have been reported, particularly in immunocompromised patients.
A 19-year-old White man with congenital human immunodeficiency virus (HIV) infection presented with a skin eruption of 4 years’ duration. Physical examination revealed a macular and papular eruption on the trunk and arms. There were multiple erythematous macules with desquamation on the chest and arms (Fig. 1) and hundreds of disseminated small pink-brownish papules, with the appearance of flat warts, on the back of the trunk and on the shoulders and arms (Fig. 2). The papules were arranged in a linear pattern (Koebner phenomenon). The lesions were asymptomatic, but had increased in number in recent months. At the time of his first evaluation the patient had a CD4 count of 544 cells/mm3 and an undetectable viral load. He was receiving highly active antiretroviral therapy (HAART) with raltegravir, ritonavir, tenofovir, and darunavir.
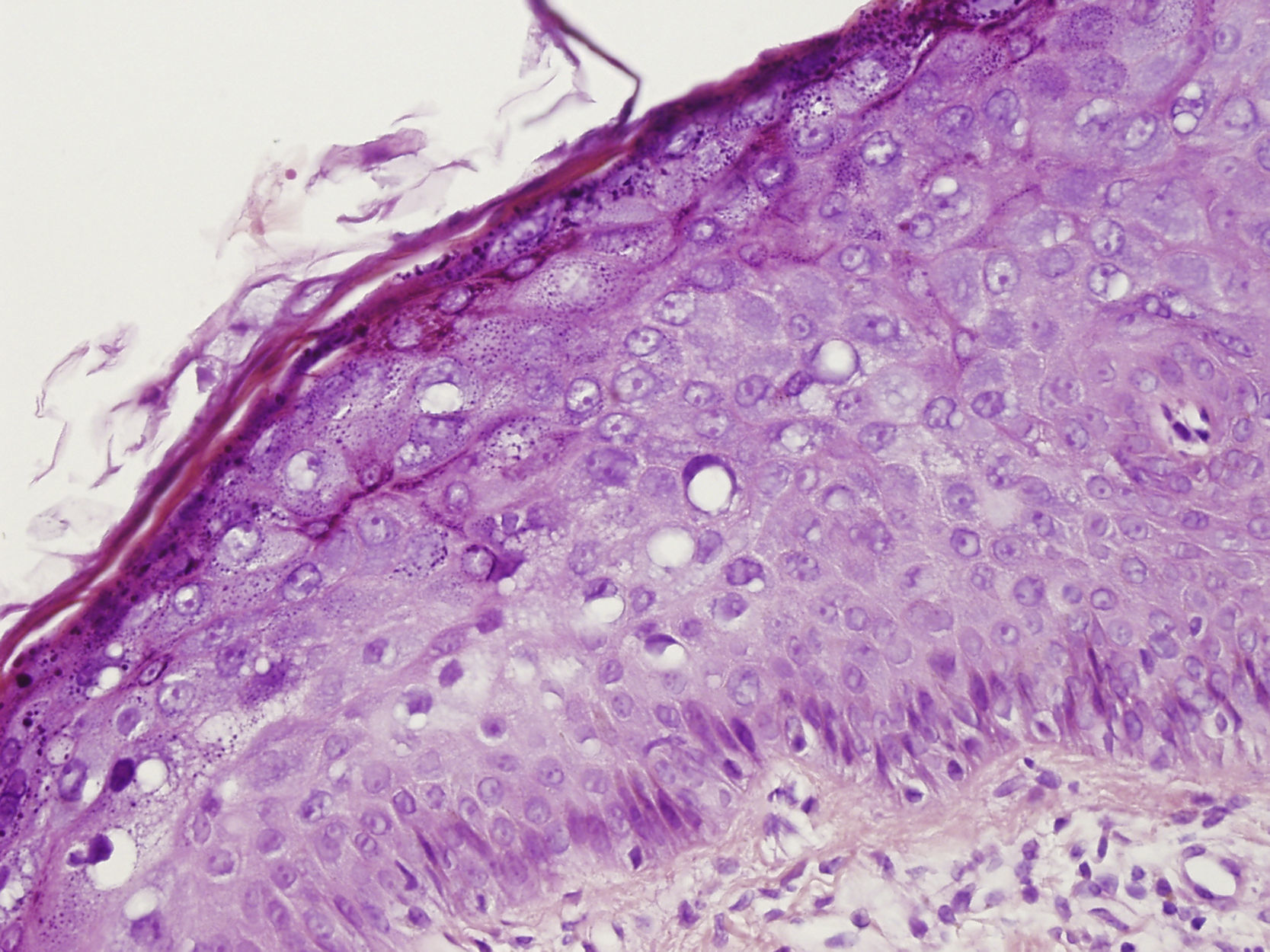
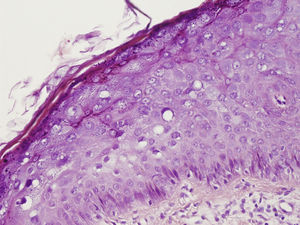
Skin biopsy of a papule on the trunk showed large keratinocytes with voluminous nuclei, basophilic cytoplasm, and perinuclear halos (Fig. 3). HPV type 5 was isolated using the nested polymerase chain reaction technique at the department of oncogenic viruses of the National Institute of Infectious Diseases Dr. Carlos Malbran.
Based on the above clinical and histological features, we made a diagnosis of EV-like eruption.
For treatment we decided to divide the back into 4 quadrants. The first quadrant was treated with topical tretinoin 0.05% cream, applied once daily for 2 months, while the second quadrant was treated with topical imiquimod 5% gel, applied once daily for 3 months. The third and fourth quadrants were treated with electrocauterization and cryosurgery, respectively. The patient was also advised to take sun protection measures.
After 3 months of treatment, we found that none of the therapeutic options had yielded satisfactory results. The patient is still receiving HAART and undergoes periodic skin examination. No signs of malignant transformation have been detected.
EV-like eruption is an HPV-related disease that is rarely seen in immunocompromised patients.3–6 It is caused by mutations in two genes, EVER1 and EVER2, located on chromosome 17q25. It was first described in kidney transplant recipients4 and then in HIV-positive patients.5
In the HIV-positive population, men and women are equally affected. Lowe et al.7proposed that this entity was more frequent in young, vertically HIV-infected patients than in adults infected later in life. This would be because younger patients would be infected by HPV when their cell-mediated immunity was already affected by HIV. On the contrary, by the time older patients are infected with HIV, they have developed better immune mechanisms against HPV infection.7 The skin lesions appear years after HIV diagnosis following a long period of immunosuppression, and tend to be chronic and refractory to the different therapies available.1,2,6 The mucosal membranes are usually unaffected.1,2
Typical histological findings are acanthosis, a prominent granular layer, vacuolated keratinocytes with perinuclear halos and blue-gray pallor cytoplasm, and rare koilocytotic keratinocytes.8
According to the literature, the progression of cutaneous lesions is not influenced by the immunological status of the patient and response to treatment is poor.2–6
The most frequent HPV strains implicated in skin eruptions are HPV subtypes 5 and 8.1,2,5,6,8,9 Co-infection with other HPV types has also been documented in several publications.1,2,6
When oncogenic HPV subtypes are involved, cutaneous lesions can progress to invasive nonmelanoma skin cancer (mostly Bowen disease and invasive squamous cell carcinomas1) after several years of cellular immunodeficiency and sun exposure.6
While this is not the first report of EV-like eruption in a patient with congenital HIV, we believe that it is of educational value and would like to stress the importance of determining the type of HPV involved in the development of disease in order to estimate the degree of oncogenic potential. We also believe it is important to closely follow all patients with EV-like eruptions, with periodic complete skin examinations, skin biopsy of suspicious lesions, avoidance of radiation therapies, improvement of immunological status, and strong recommendations to avoid sun exposure.
We would like to thank Dr. Alejandra Picconi and Ms. Mariel Correa of the Department of Virology (Oncogenic Viruses Unit) at the National Institute of Infectious Diseases Dr. Carlos Malbran for their diagnostic help.