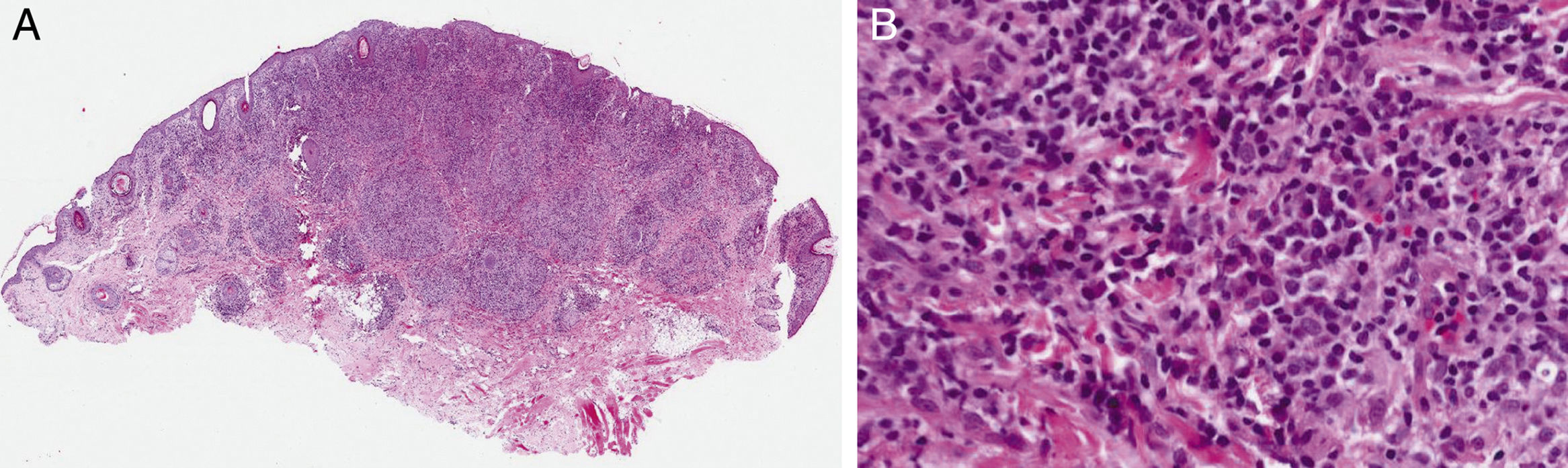
A 54-year-old woman with no relevant past history was referred to us with a facial lesion and scalp nodules of 3 weeks’ duration. She also had holocranial headache. There were no other clinical manifestations. She reported having engaged in risky sexual activity in the preceding months. Physical examination revealed a lesion with a diameter of 1×0.8cm and a “granulomatous” appearance in the chin area (Fig. 1) and 2 subcutaneous nodular lesions, each measuring approximately 1×2cm, in the frontal and occipital region. There was no occipital hair loss. The regional lymph nodes were not enlarged on palpation and no other mucocutaneous lesions were observed. The patient denied previous lesions in other areas. The results of the blood tests were leukocytes, 9600/μL (normal range, 4-10); segmented, 5900/μL (1.3-7.5); erythrocyte sedimentation rate, 57mm (1-20); ultrasensitive C-reactive protein, 3.04mg/dL (0-0.5); aspartate aminotransferase, 50IU/L (6-31); alanine aminotransferase, 48IU/L (7-40); and gamma-glutamyl transferase, 70IU/L (1-30). Skin biopsy of the facial plaque and 1 of the subcutaneous scalp nodules showed a lymphohistiocytic inflammatory infiltrate in the dermis forming noncaseating granulomas and accompanied by abundant plasma cells (Fig. 2A and B).
What is your diagnosis?
DiagnosisNodular secondary syphilis.
Clinical Course and TreatmentCultures and stains were negative for bacteria, mycobacteria, fungi, and parasites. The serological tests for syphilis were positive for nontreponemal antibodies (rapid plasma reagin [RPR] titer, 1/8) and treponemal antibodies (Immunoblot immunoglobulin M antibodies, 4.67). Warthin-Starry staining of lesions was also positive. Serology was negative for hepatitis viruses B and C and human immunodeficiency virus. In view of the refractory headache, we decided to perform a lumbar puncture, but the VDRL test was negative. With a diagnosis of secondary syphilis, we initiated treatment with a single dose of intramuscular penicillin (2.4 million units), which resulted in complete resolution of the facial lesion and subcutaneous scalp nodules. The antibody titers also decreased 1 month after treatment. After a year of follow-up, the RPR results are negative and no new lesions have appeared.
CommentSyphilis is an acute and chronic disease caused by the bacterium Treponema pallidum. It is mostly a sexually transmitted disease and its incidence has increased over the last decade. There are 4 phases of disease with varying levels of activity and infection: primary, secondary, latent, and tertiary. Syphilis is known as the great mimicker as it has a broad spectrum of clinical and histologic presentations.
Secondary syphilis generally develops 3 to 10 weeks after primary infection due to the hematogenous and/or lymphatic spread of spirochetes.2,3 It is characterized by recurrent disease and presents with mucocutaneous lesions and systemic manifestations, which may include focal neurological alterations, such as cephalea due to meningeal irritation.2 Primary syphilis lesions are often not evident and clinical manifestations may only be noticed at a later stage of infection, as occurred in our case.2 Nodular lesions are rare in syphilis.1,3 Histologically, cutaneous lesions can simulate granulomatous diseases, such as sarcoidosis, which is a rare histopathologic manifestation of syphilis.1,4 Apart from inflammatory granulomatous diseases, the differential diagnosis should include leprosy, cutaneous leishmaniasis, mycobacterial infections, foreign body granulomas, and drug-induced granulomatous reactions, among others.
We have presented a new case of nodular secondary syphilis that presented with a granulomatous facial lesion and subcutaneous nodules.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Flores-Terry MÁ, Calle MPCdl, Ramos-Rodríguez C, Martín-Dávila F. Placa facial y nódulos en cuero cabelludo. Actas Dermosifiliogr. 2018;109:441–442.