A 4-month-old infant, with no significant personal or family history, was referred due to the presence of a rash on his left hemiface for which they had been admitted 3 times to his local hospital.
ExaminationUpon examination, an erythematous-edematous rash with a few adhered crusts was observed (Fig. 1). On this occasion, the patient exhibited similar lesions, including blisters, on the pretibial area and forearms (Fig. 2). Although these episodes were not associated with prolonged sun exposure, 2 of the occurrences were consistent with car trips. The patient did not use topical sunscreen.
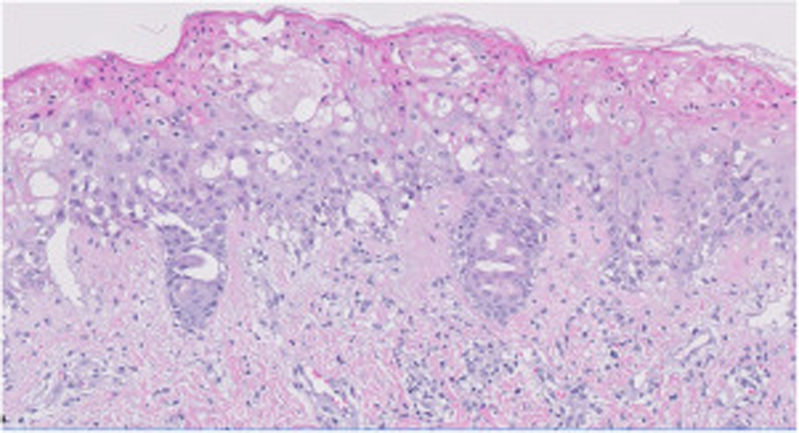
HistopathologyThe histological study of the biopsy was consistent with a picture of phototoxicity, highlighting an epidermis with ballooned keratinocytes and numerous necrotic and apoptotic keratinocytes. The dermal-epidermal junction showed vacuolation changes. The superficial dermis revealed the presence of edema and a sparse perivascular lymphocytic infiltrate (Fig. 3). Immunofluorescence testing was negative.
Other supplementary testsThe analytical study conducted included a complete blood count, biochemistry, PCR, ESR, autoimmunity study, and porphyria tests, which all tested negative. One genetic test was conducted too.
What is your diagnosis?.
DiagnosisThe genetic study diagnosed xeroderma pigmentosum (XP) type D in compound heterozygosity, after detecting the pathogenic c.2046+1G>C variant and the R683W variant as well. The patient had left congenital torticollis, which caused continuous exposure of the same hemiface.
Treatment and course of the diseaseAfter following guidelines related to solar damage prevention, the patient has not experienced any similar episodes. Currently, he remains asymptomatic with vitamin D supplementation and sunscreen.
DiscussionXP is characterized by photosensitivity, pigmentation changes, premature skin aging, photophobia, and neoplasms. The prevalence in Europe is 2.3 cases per million inhabitants.1-3 XP is an autosomal recessive genetic disorder due to mutations in some of the 8 genes involved in nucleotide excision repair (NER) pathways, which protect us from UV-induced damage. Eight types of XP have been described, all showing a marked increase in the risk of developing melanoma and non-melanoma skin cancer.2,3 The mean age of tumor growth is 9 years for non-melanoma skin carcinoma and 20 years for melanoma.1-3 Up to 25% of patients have neurological symptoms, which are more common in types A and D1, including sensorineural hearing loss, microcephaly, or cognitive impairment1, which are crucial for disease prognosis. Additionally, ocular signs appear in up to 80% of patients and can cause corneal opacifications.2
Differential diagnosis should include diseases induced or aggravated by light. Rheumatological diseases, such as systemic lupus erythematosus, metabolic diseases, such as porphyrias, or drug-induced photosensitivity reactions could explain the process. A different group of diseases that could justify the presentation includes hereditary conditions with solar hypersensitivity, such as Cockayne syndrome, Bloom syndrome, Rothmund-Thomson syndrome, and progeria syndromes.1-4 On the other hand, certain disorders unrelated to solar exposure could also have a similar onset to that of the patient in question, such as bacterial infections (Staphylococcus aureus-induced bullous impetigo), or viral infections (herpes zoster). The Meyerson phenomenon with capillary malformation could also start with a similar lesion.5
In this disease, early diagnosis and strict UV radiation protection are essential. Indeed, solar damage prevention is the cornerstone of treatment.5,6 Although there is no curative treatment, various chemopreventives have been developed in the last decade, including systemic retinoids, 5-fluorouracil, endonuclease VT4, and topical imiquimod.6
Early recognition of photosensitivity in pediatric patients is crucial to minimize long-term complications associated with inadequate photoprotection.
FundingNone declared.
Conflicto de interesesLos autores declaran no tener ningún conflicto de intereses.