Pigmentovascular phacomatosis is a rare congenital disorder characterized by the coexistence of cutaneous vascular malformations and melanocytic lesions.1,2 Recent reports confirm that it can be the result of somatic mosaicism including activating mutations of GNAQ and GNA11 genes.2 Pigmentovascular phacomatosis can also present abnormalities in multiple organs, such as the eyes and the central nervous system.1,2 Central nervous system disorders described in the medical literature currently available include leptomeningeal angiomatosis, ventriculomegaly, cerebral calcifications and atrophy.2 However, the association between pigmentovascular phacomatosis and the presence of bilateral temporal arachnoid cysts has not been reported to this date. We describe a patient with this association below.
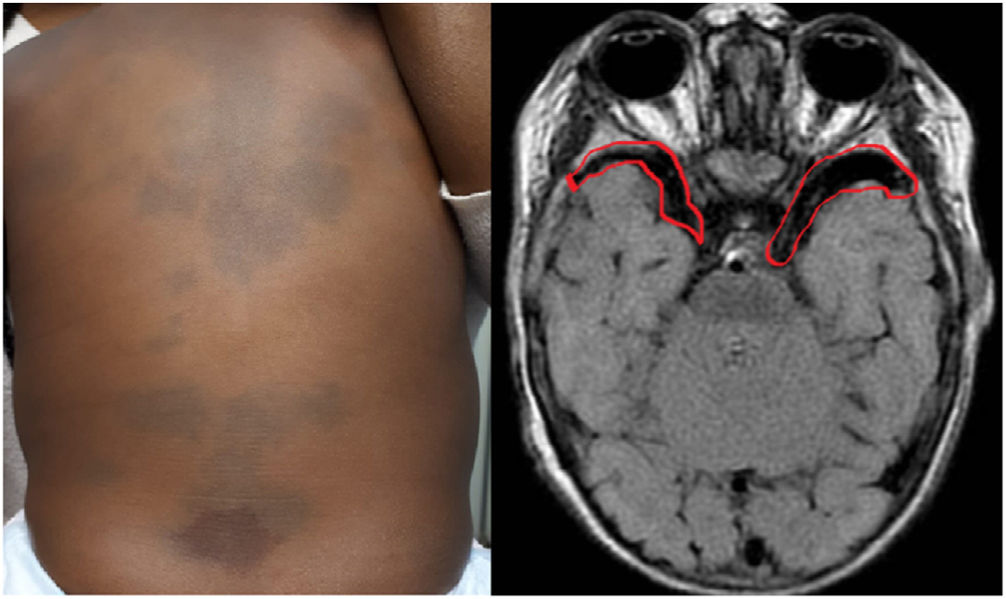
A 10-month-old girl presented to the pediatric dermatology clinic with an erythematous patch on the lumbar area and multiple bluish patches present since birth on the rest of the trunk. The mother's gynecological and obstetric history was normal, and her parents were not consanguineous. Up to that point, the girl had remained healthy, symptom-free, and with a completely normal psychomotor development. The skin examination revealed the presence of a reddish-violet, vascular patch on the lumbar region consistent with a capillary malformation. Additionally, she showed several aberrant Mongolian spots on her buttocks, back, shoulders, and upper limb roots (figure 1A). The diagnosis was phacomatosis pigmentovascularis of cesioflammea type. The ophthalmological and neuropediatric evaluations were normal. However, the nuclear magnetic resonance imaging revealed the presence of bilateral temporal arachnoid cysts (figure 1B).
Neurocutaneous syndromes or phacomatoses are associated with a plethora of congenital disorders including neuroectodermal and, sometimes, mesodermal development abnormalities often affecting the skin, eyes, and the nervous system. Pigmentovascular phacomatoses represent a heterogeneous group of diseases characterized by the coexistence of cutaneous vascular malformations and pigmented nevi.1–3
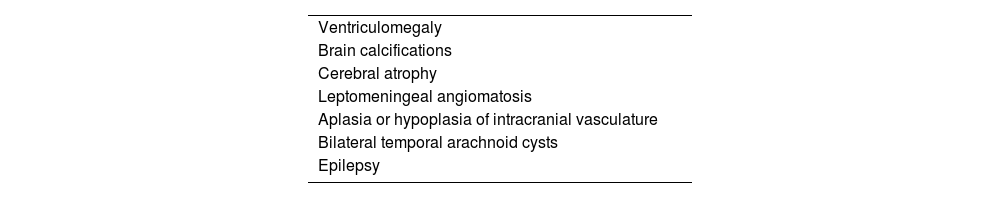
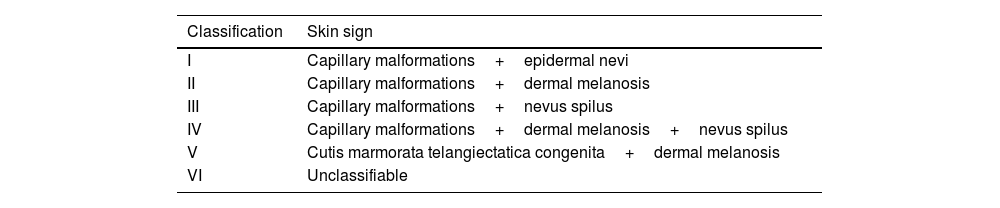
Hasegawa's classification includes 6 types of phacomatoses, which are further subcategorized based on the presence or absence of extracutaneous involvement3 (Table 1). In 2005, Happle proposed a simplified classification into 4 categories: phacomatosis pigmentovascularis of cesioflammea type, phacomatosis spilorosea, unclassifiable forms of phacomatosis, and phacomatosis cesiomarmorata.1–3 Until that time, a total of 250 cases of pigmentovascular phacomatosis had been reported, being 75% of them phacomatosis pigmentovascularis of cesioflammea type.3 Extracutaneous signs in pigmentovascular phacomatosis have been reported in up to 50% of the cases, mainly including central nervous system abnormalities, ocular defects, alopecia, renal agenesis, the Klippel-Trenaunay syndrome, and the Sturge-Weber syndrome. Advances in neuroimaging modalities have improved the ability to demonstrate the association between pigmentovascular phacomatosis and intracranial abnormalities, including arachnoid cysts.1,2 (Table 2).
Hasegawa's classification.
| Classification | Skin sign |
|---|---|
| I | Capillary malformations+epidermal nevi |
| II | Capillary malformations+dermal melanosis |
| III | Capillary malformations+nevus spilus |
| IV | Capillary malformations+dermal melanosis+nevus spilus |
| V | Cutis marmorata telangiectatica congenita+dermal melanosis |
| VI | Unclassifiable |
In the scientific literature, arachnoid cysts represent only 1% of all intracranial space-occupying lesions, and in most cases, a single lesion is reported.4 The presence of bilateral arachnoid cysts is extremely rare. In fact, the presence of bilateral arachnoid cysts suggests the need to rule out metabolic disorders, and/or their association with other phacomatoses.4 In the medical literature has been described in association with neurofibromatosis and tuberous sclerosis in one case but not with pigmentovascular phacomatosis.5,6 On the other hand, activating mutations of genes GNAQ and GNA,11 which are associated with pigmentovascular phacomatosis, are also present in the Sturge-Weber syndrome, where arachnoid cysts have also been reported.6 Based on these observations, we believe that genetic factors are likely responsible for this association.
In conclusion, bilateral temporal arachnoid cysts should be included as part of the wide range of central nervous system abnormalities that should be taken into consideration when diagnosing and studying this type of phacomatosis. Because of the plethora of neurological signs reported, and the fact that these are the most common extracutaneous findings acquiring imaging modalities from patients diagnosed with this condition is certainly advised.