Since 2000, substantial increases in syphilis have been reported in metropolitan areas of Western countries, with increases noted among men who have sex with men (MSM). Clinical manifestations of syphilis might be influenced by concomitant VIH infection and previous episodes of syphilis. The objectives of this study were to describe the epidemiological and clinical characteristics of the cases of syphilis diagnosed in Barcelona.
MethodsRetrospective study of cases with early syphilis diagnosed in the referral STI Unit of Barcelona from January 2003 to December 2013. Revision of medical records with structured collection of epidemiological and clinical data. Univariate and multivariate statistical analyses comparing the characteristics of MSM cases with and without VIH infection and with and without previous syphilis.
ResultsA total of 1702 cases of syphilis (37% primary, 48% secondary and 14% early latent) were diagnosed, 93% of them in MSM. Among MSM 40% were coinfected with VIH, VIH-positive cases were associated with a previous syphilis (aOR, 5.2 [95% CI, 3.32–8.24]) and with unprotected anal intercourse (aOR, 1.75 [95%CI, 1.17–2.63]). Cases with a history of syphilis presented less often with primary syphilis compared to those without it (27.5% vs 40%) (aOR, 0.58 [95% CI, 0.44-0.77]). One year after treatment, the clinical and serological evolution were similar between VIH-positive and VIH-negative cases.
ConclusionThe epidemic of syphilis in Barcelona disproportionately affects MSM and is closelly linked to VIH infection. The presentation of syphilis is influenced by VIH infection and by previous history of syphilis, without significant differences in their evolution after one year of treatment.
Desde el año 2000 se ha descrito un aumento progresivo de los casos de sífilis en diferentes ciudades europeas, sobre todo en hombres que tienen sexo con hombres (HSH). Las manifestaciones clínicas de la sífilis pueden estar influenciadas por la coinfección del VIH o por el antecedente de sífilis. El objetivo del presente estudio es describir las características epidemiológicas y clínicas de los casos de sífilis precoz diagnosticados en Barcelona.
MétodosEstudio retrospectivo de casos de sífilis precoz diagnosticados en Barcelona (2003-2013). Se revisaron las historias clínicas y los datos epidemiológicos y clínicos fueron recogidos de forma estructurada. Las variables se compararon según el estatus serológico del VIH y el antecedente de sífilis.
ResultadosSe diagnosticaron 1702 casos de sífilis precoz (37% primaria, 48% secundaria y 14% latente precoz), 93% de ellos en HSH. Entre ellos, el 40% presentaba una coinfección por VIH. Los casos de sífilis en pacientes VIH positivos estaban asociados con un episodio previo de sífilis (aOR, 5.2 [95% CI, 3.32-8.24]) y con el haber tenido sexo anal desprotegido (aOR, 1.75 [95%CI, 1.17-2.63]). Los casos con antecedentes de sífilis se presentaron con menor frecuencia como sífilis primaria (27.5% vs 40%) (aOR, 0.58 [95% CI, 0.44-0.77]). Un año después del tratamiento, la evolución clínica y serológica fue similar en los pacientes VIH positivo y negativo.
ConclusionesLa epidemia de sífilis en Barcelona afecta desproporcionalmente a HSH y está estrechamente relacionada con el VIH. La forma de presentación de la sífilis está influenciada por el antecedente de sífilis y por el VIH, sin diferencias significativas en cuanto a la evolución un año después del tratamiento.
Since 2000, substantial increases in syphilis have been reported in metropolitan areas of Western countries, with increases noted among men who have sex with men (MSM). In Europe, there were 22237 cases of early syphilis reported in 2013, with a rate of 5·5 per 100000 inhabitants, 62% of cases were notified from 4 countries including Spain.1 Catalonia (Spain) with 7 million inhabitants had an early syphilis rate of 12·4 per 100000 inhabitants in 2014 representing an increase of 231% since 2005.2 The re-emerging of syphilis in Catalonia was detected in Barcelona in 2002 mainly in MSM with an HIV coinfection rate of 30%.3
The objectives of this study are to describe retrospectively the epidemiological and the clinical characteristics of the cases of early syphilis diagnosed in the STI Unit Vall d’Hebron-Drassanes (STIUVD) in Barcelona within the period 2003-2013, particularly in MSM. The STIUVD provides care to clients who make over 25000 patient visits per year (60% MSM) and reported almost 75% of syphilis cases in Barcelona during the study period.
MethodsParticipants and data collectionWe reviewed all cases of syphilis reported from the STIUVD since January 2003 to December 2013. A total of 2209 histories were revised, 242 were excluded: 52 for not belonging to the period of the study and 190 for abscense of data or unclear final diagnosis of syphilis. 2241 cases (where a case refers to an episode, being able that tha same patients could have more than one episode) had been diagnosed in the STIUVD during the study period, with 1702 of them being classified as early syphilis in 1484 patients. Epidemiological, clinical and microbiological data were retrieved from these clinical records of primary, secondary and early latent syphilis cases in a standardized way. Also, behavioral data related to stable/sporadic partner, number of sexual contacts and condom use in anal sex was gathered. Other variables that were missing in more than 50% of cases (e.g. drug use) due to variations in data collection over the period were not analyzed.
ProceduresSyphilis infection had been diagnosed by clinical examination, serological evaluation and direct detection when ulcers were present. The serological tests used were the Rapid Plasma Reagin (RPR) test (Biokit, Spain), Treponema pallidum particle haemagglutination test (Biokit, Spain) and Treponemal Enzyme Immunoassay (Siemens Healthcare Diagnostics, Germany). Direct diagnosis was performed by dark-field microscopy or in house PCR for T. pallidum.4 Syphilis cases were staged and classified according to the European guideline on the management of syphilis.5 Early latent syphilis was defined as a positive serological test with a previous negative syphilis serology, or a four-fold increase in the titer of a non-treponemal test (in more than 2 dilutions) within the past 12 months. Reinfection was defined as a new clinical manifestation and an increase of 2 dilutions of non-treponemal test. Serological cure was defined as a four-fold decline (at least two titers) in RPR titers. STI laboratory tests varied during the period of the study, of note the introduction of real time-PCR test for Chlamydia trachomatis (CT) since 2006, Neisseria gonorrhoeae (NG) since 2012, and T. pallidum since 2013. Concomitant infection was defined as HIV, NG and/or CT being diagnosed at the time of syphilis diagnosis (whether the later one was in one or more anatomical sites).
Statistical analysisFirst a descriptive study of all the cases was made, focusing later on MSM (including bisexual men) comparing epidemiological and clinical findings according to HIV status and previous history of syphilis. We conducted univariate and multivariate logistic regression analyses. All analyses were performed in R Version 3·3·1 (The R Foundation for Statistical Computing, Vienna, Austria). Qualitative variables were expressed as percentages; comparisons were made by Chi-square test or Fisher exact test as appropriate. The strength of the association was measured with OR with 95% confidence intervals (95% CI). Quantitave variables were expressed as mean (± SD) or median and interquantile range (IQR). Comparisons were made by T-Test or Mann-Whitney U test, or ANOVA or Kruskal-Wallis test with 95% CI if there were more than two categories. Variables which were significant at univariate level (P<0.01) or were considered clinically relevant, were tested in a final regression model using the Akaike information criterion. Ethical approval was granted by the Hospital Vall d’Hebron Ethics’ Committee.
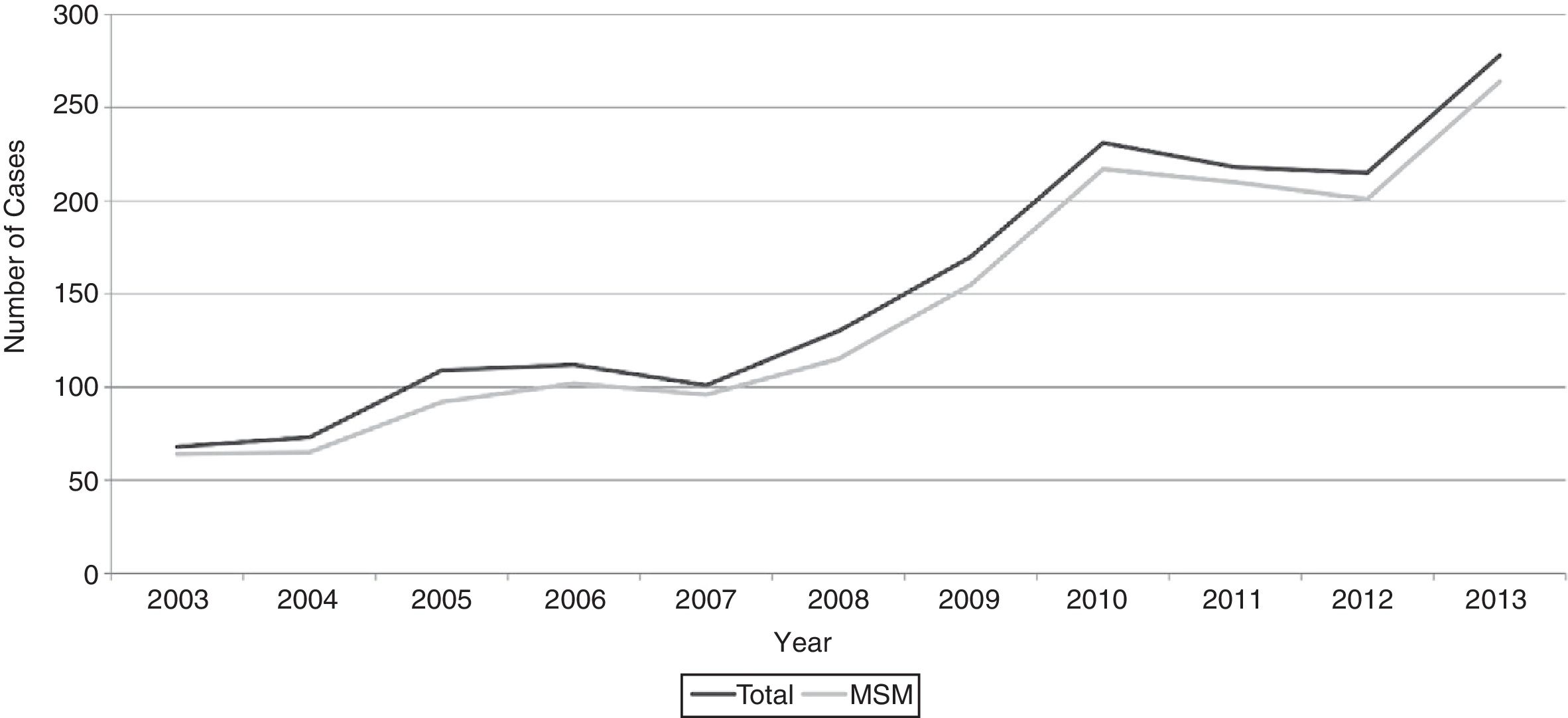
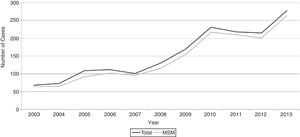
ResultsThe number of cases increased from 68 in 2003 to 277 in 2013 up to a total of 1702 during the period of the study: 97% (165) of the cases were diagnosed in men, 2% (33) in women and 1% (14) in transexuals. Out of the 1702 cases, 1425 (84%) were MSM, 155 (9%) bisexual men, 112 (6.9%) heterosexual men and women and ten (0.6%) unknown (Figure 1). The average age was 35·3±8·9 years, without showing significant changes during the period. Overall, 57% (971) of cases were native and 43% (731) were foreigners these latter once ranging from 32% (22 of 68) in 2003 to 43.5% (120/277) in 2013. 1239 (73%) of the cases had clinical symptoms suggestive of syphilis, 250 (15%) were diagnosed incidentally during an STI screening, 158 (9%) by contact tracing and 54 (3%) during an opportunistic screening in an STI symptomatic cases. From all the cases, 637 (38%) were primary, 829 (48%) were secondary, and 236 (14%) were classified as early latent syphilis. There were changes in practice over the years: at the beginning, most of the cases were registered with symptoms and only 9% (6 of 68) were diagnosed by testing alone; the diagnoses of syphilis by screening increased up to a maximum of 20% (42/215) in 2012. Similarly, diagnoses through contact tracing increased from 4% (3/68) in 2003 to 14% (39/277) in 2013. In parallel to this, the proportion of early latent syphilis diagnoses increased from 7% (5/68) in 2003 to 19% (53/277) in 2013.
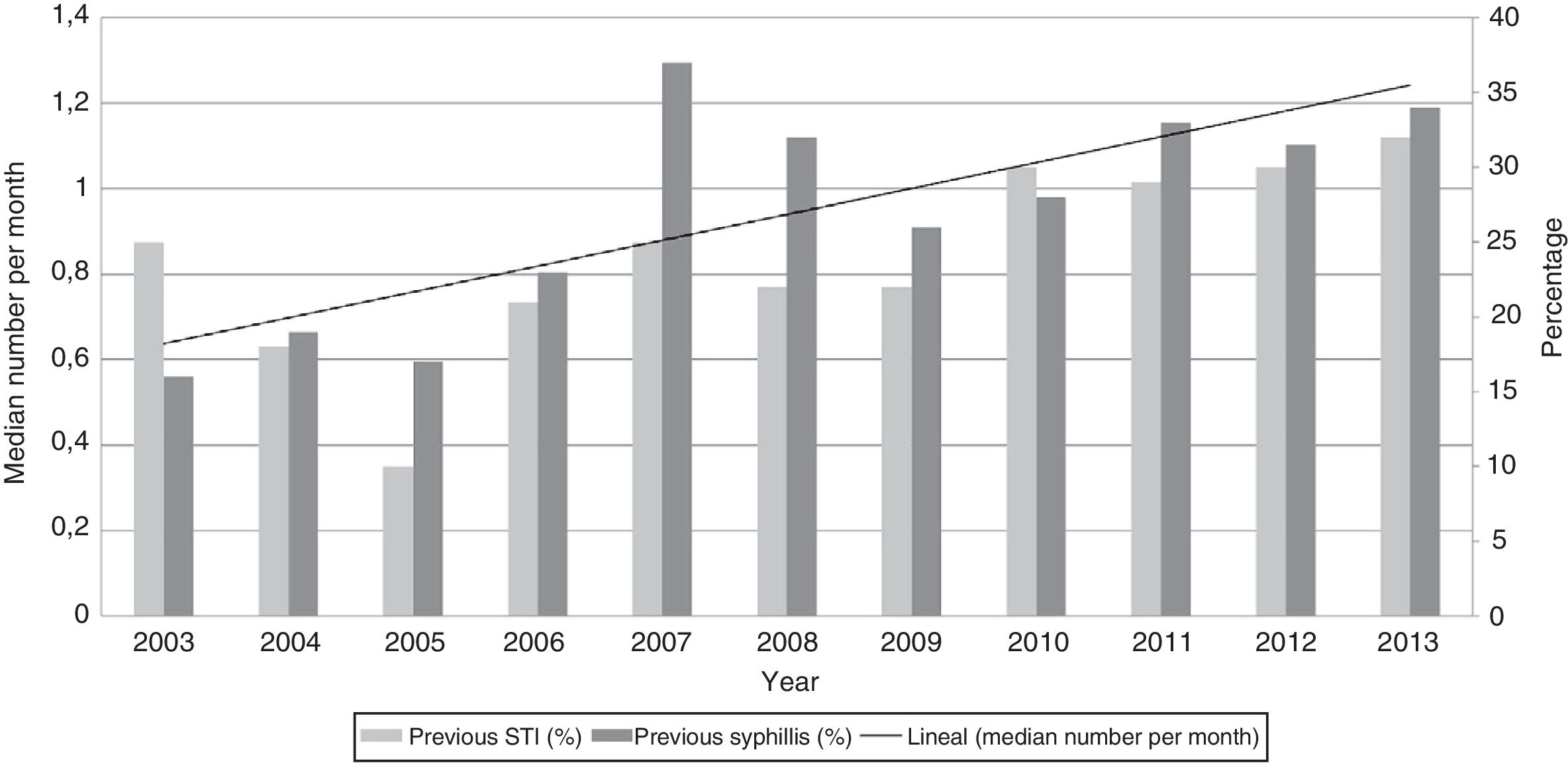
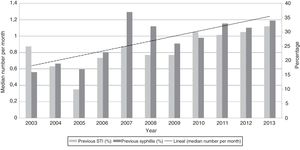
Overall 30% (n=517) of the cases had been diagnosed with HIV infection prior to diagnosis of syphilis, without a significant trend in prevalence over the years. Concerning history of syphilis, 29% (n=487) of the cases had had at least one previous episode of syphilis, showing a progressive increase from 16% (11/68) in 2003 to 34% (93/277) in 2013. A similar trend over time was also seen for other STI (Figure 2). Having multiple partners was reported by 92% of the cases; with a median of 1 [0·33- 2·00] contact per month, the number of partners increased throughout the period (Figure 2). Results from opportunistic testing for STI at the time of syphilis diagnoses were available from 615 cases (36%). Concomitant infection was present in 205 (33%) of those cases with prevalences of 14·5% (89/615), 8% (49/615), 7·5% (47/615) and 3% (20/615) for HIV, NG, CT and Lymphogranuloma venereum (LGV) respectively. Changes in practice over the time would have influenced those findings since in 2003 only 11% (8/68) of casess were screened for STI (HIV only) in contrast to 2013 when 65% (182/277) of syphilis cases received a complete STI screening. Twenty percent of the 87 MSM patients newly diagnosed with HIV had a previous syphilis history. Below we focus the analysis on MSM, including bisexual men (n=1580).
Comparison between HIV-positive and HIV-negative MSM patientsAvailable HIV information from 1497 syphilis cases in MSM showed that 600 (40%) of them were coinfected with HIV: 513 with a prior diagnosis and 87 newly diagnosed at time of syphilis diagnosis. Comparisons between HIV-positive and HIV-negative patients appear in Table1: HIV-positive cases were significantly older, of foreign origin and with previous histories of STI and of syphilis. Also, they showed higher number of sexual contacts per month and less condom use for anal sex. Regarding syphilis stage, secondary syphilis was the most frequent presentation in both groups. HIV-positive patients presented more often with symptoms without differences in the duration of symptoms (median 8 days). Concomitant CT and LGV were more frequent in HIV-positive cases (23 (11·5%) and 14 (4%) of the 199 cases who had undergone the screening) than in HIV-negative cases (16 (7%) and 6 (1.5%) of 356 cases) respectively. Notably, HIV-positive cases were associated with a previous syphilis (adjusted OR, 5·2 [95% CI, 3·32-8·24]) and other STI histories (adjusted OR, 1·62 [95% CI, 1·09-2·43]) and with unprotected anal intercourse (adjusted OR, 1·75 [95%CI, 1·17-2·63]) in the multivariate analysis.
Epidemiological and clinical findings among MSM with early syphilis in Barcelona by HIV status, 2003–2013.
| HIV positive N=600 (40%) n (%) | HIV negative N=897 (60%) n (%) | p | OR | Ajusted OR | ||
|---|---|---|---|---|---|---|
| Age | <0.001 | |||||
| 16-24 | 20 (3.5) | 93 (10.5) | ||||
| 25-34 | 217 (36) | 391 (43.5) | 2.58 [1.58-4.41] | 2.23 [0.94-6.07] | ||
| 35-44 | 259 (43) | 292 (32.5) | 4.12 [2.52-7] | 2.97 [1.24-8.13] | ||
| 45-79 | 104 (17.5) | 121 (13.5) | 4 [2.35-7] | 2.17 [0.84-6.42] | ||
| Origin | <0.001 | |||||
| Spain | 294 (50.5) | 568 (65) | ||||
| Other Western countries | 106 (18) | 110 (12.5) | 1.86 [1.38-2.5] | 2 [1.16-3.44] | ||
| Latin America | 161 (27.5) | 161 (18.5) | 1.93 [1.49-2.5] | 2.21 [1.36-3.6] | ||
| Other | 22 (4) | 37 (4) | 1.15 [0.66-1.97] | 1.5 [0.57-3.67] | ||
| Previous STIa (Yes) | 336 (56) | 313 (35) | <0.001 | 2.38 [1.93-2.96] | 1.62 [1.09-2.43] | |
| Previous syphilis (Yes) | 305 (51) | 166 (19) | <0.001 | 4.55 [3.61-5.75] | 5.2 [3.32-8.24] | |
| Multiple sexual partners (Yes) (N=1163) | 425 (95) | 673 (94) | 0.686 | |||
| Number of sexual partners per month (median) [IQ] | 1.33 [0.5;3.33] | 1[0.42;2] | <0.001 | 1.08 [1.03-1.12] | 1.11 [1.04-1.19] | |
| Unprotected anal intercourse (Yes) (N=626) | 104 (46) | 136 (34) | 0.005 | 1.64 [1.17-2.28] | 1.75 [1.17-2.63] | |
| Syphilis stage | 0.044 | |||||
| Secondary | 324 (54) | 427 (47.5) | ||||
| Primary | 192 (32) | 337 (37.5) | 0.83[0.6-0.94] | |||
| Early latent | 84 (14) | 133 (15) | 0.83[0.61-1.13] | |||
| Reason for visit | <0.001 | |||||
| Syphilis symptoms | 451 (75) | 628 (70) | ||||
| Other STI symptoms | 33 (5.5) | 15 (1.5) | 3 [1.67-5.87] | |||
| STI screening | 63 (10.5) | 171 (19) | 0.5 [0.37-0.7] | |||
| Contact tracing | 53 (9) | 83 (9.5) | 0.89 [0.61-1.28] |
Data represent number (%) unless otherwise indicated.
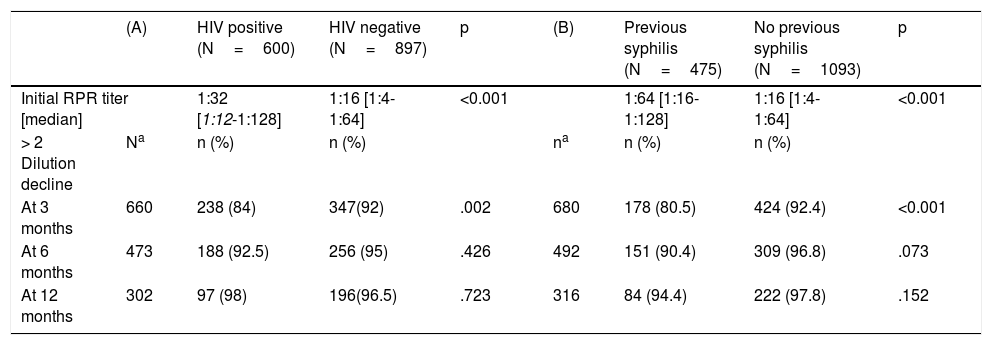
At syphilis diagnosis RPR titers were higher in HIV-positive patients: median of 1/32 [1/12-1/128] compared to 1/16 [1/4-1/64] (P <0.001) in HIV-negative patients. Without differences between them, 40% (612/1497) of all cases were lost to follow up for serological control. Serological cure was achieved earlier in HIV-negative patients at 3 months, but similar in both group at 6 and 12 months (Table 2). HIV-positive cases more frequently received 3 weekly doses of benzatine penicillin (following earlier recommendations of some experts).
Initial RPR test titer and evolution of the number of cases achieving > 2 dilution decline in titers after treatment by (A) HIV status and (B) previous history of syphilis.
| (A) | HIV positive (N=600) | HIV negative (N=897) | p | (B) | Previous syphilis (N=475) | No previous syphilis (N=1093) | p | ||
|---|---|---|---|---|---|---|---|---|---|
| Initial RPR titer [median] | 1:32 [1:12-1:128] | 1:16 [1:4-1:64] | <0.001 | 1:64 [1:16-1:128] | 1:16 [1:4-1:64] | <0.001 | |||
| > 2 Dilution decline | Na | n (%) | n (%) | na | n (%) | n (%) | |||
| At 3 months | 660 | 238 (84) | 347(92) | .002 | 680 | 178 (80.5) | 424 (92.4) | <0.001 | |
| At 6 months | 473 | 188 (92.5) | 256 (95) | .426 | 492 | 151 (90.4) | 309 (96.8) | .073 | |
| At 12 months | 302 | 97 (98) | 196(96.5) | .723 | 316 | 84 (94.4) | 222 (97.8) | .152 | |
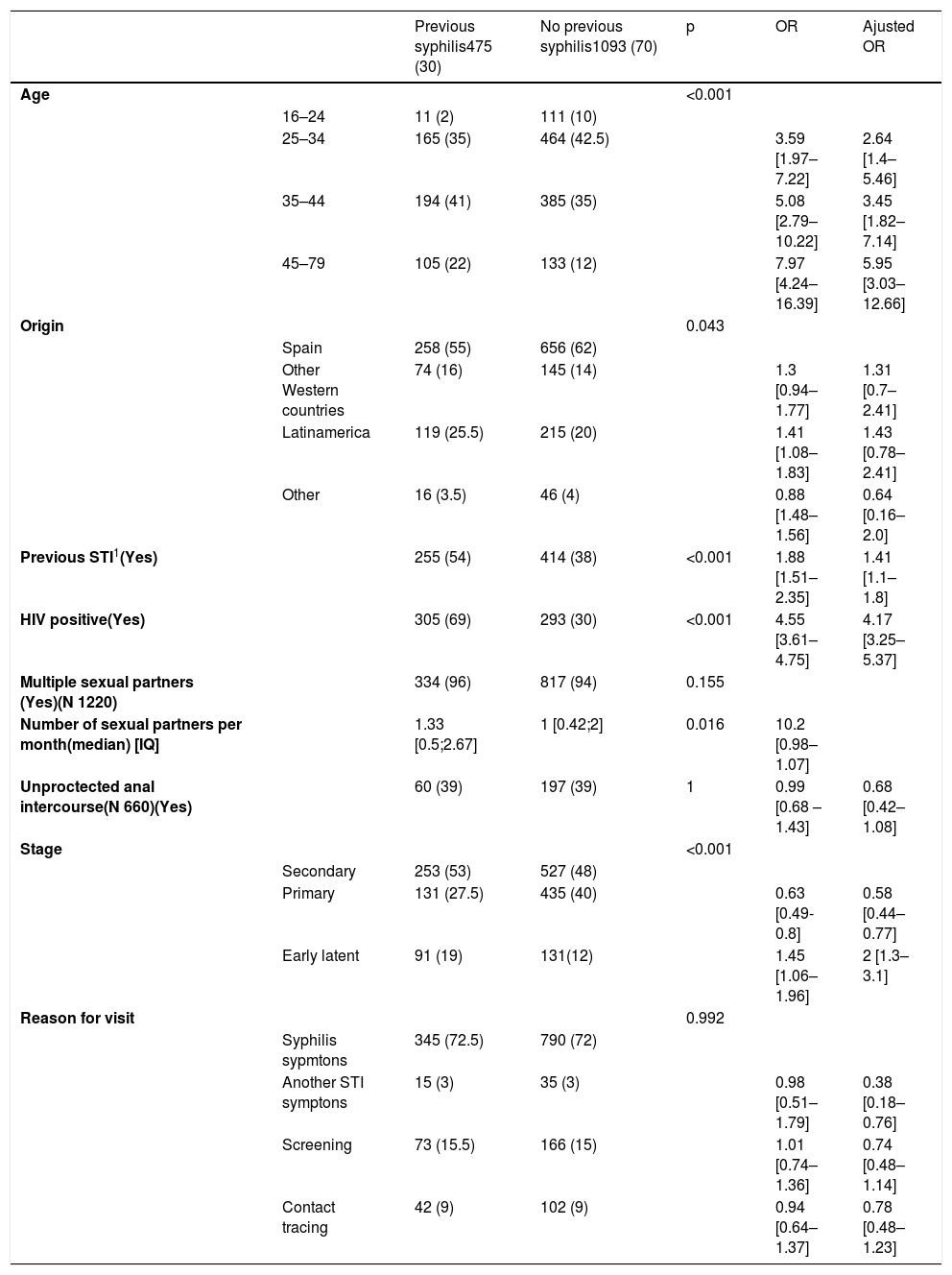
Information about previous history of syphilis from 1568 MSM cases showed that 475 (30%) of them had had at least one lifetime episode before. Some of the comparisons between cases with and without previous history of syphilis appear in Table 3. Those with a previous history of syphilis were significantly older, with previous history of STI, were coinfected with HIV and presented less frequently with primary syphilis (131 (28%) of 475 vs 435 (40%) of 1093) with a shorter duration of symptoms (median 7 vs 10 days, P <0.001). Those with a previous history of syphilis showed a higher number of sexual contacts per month. Available information from 582 cases showed that overall 45% (173) of them had a concomitant infection without differences in both groups (including HIV). Remarkably, cases with a previous history of syphilis, were strongly associated with being coinfected with HIV (adjusted OR, 4·43 [95% CI, 3·47-5·68]) and with other previous STI history (adjusted OR, 1·41 [95%CI, 1·1-1·8]) in the multivariate analysis.
Epidemiological and clinical findings among MSM with early syphilis in Barcelona by previous syphilis history, 2003-2013.
| Previous syphilis475 (30) | No previous syphilis1093 (70) | p | OR | Ajusted OR | ||
|---|---|---|---|---|---|---|
| Age | <0.001 | |||||
| 16–24 | 11 (2) | 111 (10) | ||||
| 25–34 | 165 (35) | 464 (42.5) | 3.59 [1.97–7.22] | 2.64 [1.4–5.46] | ||
| 35–44 | 194 (41) | 385 (35) | 5.08 [2.79–10.22] | 3.45 [1.82–7.14] | ||
| 45–79 | 105 (22) | 133 (12) | 7.97 [4.24–16.39] | 5.95 [3.03–12.66] | ||
| Origin | 0.043 | |||||
| Spain | 258 (55) | 656 (62) | ||||
| Other Western countries | 74 (16) | 145 (14) | 1.3 [0.94–1.77] | 1.31 [0.7–2.41] | ||
| Latinamerica | 119 (25.5) | 215 (20) | 1.41 [1.08–1.83] | 1.43 [0.78–2.41] | ||
| Other | 16 (3.5) | 46 (4) | 0.88 [1.48–1.56] | 0.64 [0.16–2.0] | ||
| Previous STI1(Yes) | 255 (54) | 414 (38) | <0.001 | 1.88 [1.51–2.35] | 1.41 [1.1–1.8] | |
| HIV positive(Yes) | 305 (69) | 293 (30) | <0.001 | 4.55 [3.61–4.75] | 4.17 [3.25–5.37] | |
| Multiple sexual partners (Yes)(N 1220) | 334 (96) | 817 (94) | 0.155 | |||
| Number of sexual partners per month(median) [IQ] | 1.33 [0.5;2.67] | 1 [0.42;2] | 0.016 | 10.2 [0.98–1.07] | ||
| Unproctected anal intercourse(N 660)(Yes) | 60 (39) | 197 (39) | 1 | 0.99 [0.68 –1.43] | 0.68 [0.42–1.08] | |
| Stage | <0.001 | |||||
| Secondary | 253 (53) | 527 (48) | ||||
| Primary | 131 (27.5) | 435 (40) | 0.63 [0.49-0.8] | 0.58 [0.44–0.77] | ||
| Early latent | 91 (19) | 131(12) | 1.45 [1.06–1.96] | 2 [1.3–3.1] | ||
| Reason for visit | 0.992 | |||||
| Syphilis sypmtons | 345 (72.5) | 790 (72) | ||||
| Another STI symptons | 15 (3) | 35 (3) | 0.98 [0.51–1.79] | 0.38 [0.18–0.76] | ||
| Screening | 73 (15.5) | 166 (15) | 1.01 [0.74–1.36] | 0.74 [0.48–1.14] | ||
| Contact tracing | 42 (9) | 102 (9) | 0.94 [0.64–1.37] | 0.78 [0.48–1.23] |
Data represent number (%) unless otherwise indicated.
At syphilis diagnosis RPR titers were higher in cases with history of previous syphilis: median of 1/64 [1/16-1/128] compared with 1/16 [1/4-1/64] (P <0.001) in cases without a previous history. Fewer proportion of cases with previous syphilis (163 (34%) of 475 than those without it (484(44%) of 1093) were lost to follow up serologically (P =0·002). Serological cure rates among cases without history of syphilis were achieved earlier in the first 6 months, but were similar at 12 months after therapy (Table 2).
DiscussionIn this referral STI Unit of Barcelona we have documented a sustained increase in the number of people diagnosed with syphilis between 2003 and 2013 following its re-emerging in Barcelona in 2002.3 The phase specific epidemic curve was an hyperendemic one showing absence of controls.6 In our setting the dominant profile of the epidemic was MSM. Globally in high-income settings, MSM accounts for a disproportionate burden of syphilis infections.7 Different behavioral risk factors have been related to this, such as number of sexual contacts, drug use during sexual intercourse, condomless anal sex, serosorting, anonymous sex and contacting sex partners through internet,8,9 possibly in connection with the phased introduction of highly effective antiretroviral therapy.10 The rise in risky sexual behavior11 in this population group is supported by the parallel rise in several STI over time,12,13 shown also in our study.
Focusing on MSM, primary and secondary syphilis comprised respectively 36% (578/1588) and 49.5% (787/1588) of the cases in our study, without differences in HIV status in the multivariate analyses. Unlike ours, other studies had found a higher proportion of early latent syphilis in connection with frequent syphilis screening among HIV positive patients’.14 Syphilis and HIV are closely related since syphilis can increase the risk of HIV transmission by increasing HIV shedding, and acquisition by providing a portal of entry to the HIV virus.15 Thirty four percent (513/1497) of the cases had been diagnosed with HIV prior to diagnosis of syphilis, a proportion similar to that of other studies from Europe and North America.1,16 Concomitantly with syphilis, a further 9% (87/984) of MSM were newly diagnosed with HIV during the study, 20% of them having previous diagnoses of syphilis. It has been shown that syphilis predicts HIV seroconversion, with an incidence between 5 and 20% in the 5 and 10 years after syphilis diagnosis respectively.17 On the other side, almost one third of the cohort had had at least one previous episode of syphilis. However, HIV-positive patients were five more times likely to have had syphilis previously than HIV-negative patients. In this regard similar data have been showed in other studies.8,18 Altogether this points out that syphilis is transmitted largely within tight sexual and social networks of MSM.19
In HIV-positive patients, higher RPR titers (with slower 2-dilution decline at 3 months) were observed compared with HIV-negative patients. However, this serological response to therapy was similar in both groups at 6 and 12 months. Some earlier studies had found a higher frequency of serological failures among HIV-positive MSM, having as a possible cause the immunodeficiency caused by HIV.20,21 Instead, more recent studies like ours show that a meaningful serological response depends more on stage of disease, test titer at time of diagnosis or age rather than on HIV coinfection, history of syphilis or treatment received.22,23
Our study provides some interesting further insight into the clinical manifestations of syphilis and the evolution of serological reagin titers among patients who had a previous syphilis infection. We found that patients with syphilis history were significantly less likely to present primary syphilis (28%) compared to patients without a previous syphilis infection (40%). Brewer et al suggested that this might be due to differences in sexual behavior in that the chancre goes unnoticed in MSM because it could be located at the anus and mouth.24 In our case this reason couldn’t explain the difference because the study was done exclusively in MSM. Also, Courjon et al described less severe skin manifestations during reinfection episodes.25 Thus, we too question whether the chancre might be less symptomatic and be unnoticed in re-infections,26 perhaps related to some host immune factors’.27 Our finding is in agreement with the results of the experimental study in volunteers done by Magnuson et al,28 showing that patients previously treated for syphilis were less likely to develop a chancre when they were reinoculated with T. pallidum. Also we found that previous syphilis infection showed some serological delayed response to therapy which is in line with the study of Romanowski et al demonstrating that individuals with their first infection were more likely to serorevert than those with re-infections.29 Quoting Magnuson et al patients who have once had syphilis are never immunologically the same.28
Our results are subject to limitations. First, data were obtained retrospectively from clinical records subject to some uncertainties and incompleteness in some variables that could not be studied. Second, our results come from a single clinic in Barcelona. Nevertheless, the fact that during the study period there had not been changes in accessibility to our clinic and that it is the referral STI centre in Barcelona all point out that the increasing number of patients diagnosed very probably are a reflection of the increasing incidence of syphilis. Third, diagnostic techniques and screening practices did change over the study period limiting the detection of some concomitant infections. Finally, follow-up of patients after the diagnosis of syphilis was limited to the cases followed up in our clinic.
ConclusionsOver a decade since 2003 the epidemic of syphilis continued without control in Barcelona. Like in other parts of Western Europe and North America it disproportionately affected MSM and was closely linked with HIV infection transmitted largely within core groups. Hence, syphilis has become an important and complex public health problem in Barcelona and other major cities. Beyond primary prevention, due to a return to unsafe sexual practices -especially condomless anal sex- approaches for syphilis control remain as proposed almost one hundred years ago: widespread screening, professional and public education and engagement, timely treatment, and continued reseach to improve these efforts.30 Our study is reassuring that the clinical and serological evolution of syphilis is rather similar regardless of HIV status. The presentation of syphilis is influenced by concomitant HIV infection and by previous history of syphilis, without differences in their serological response after one year of treatment.
Conflicts of interestAll authors: no reported conflicts.
This research received no specific grant from any funding agency, commercial or not-for profit sectors.
The statistical analysis has been carried out in Statistics and Bioinformatics Unit in Vall d’Hebron Institute of Research.
Please cite this article as: Arando M, Caballero E, Curran A, Armengol P, Barberá MJ, Vall-Mayans M. Las características epidemiológicas y clínicas de la epidemia de sífilis en Barcelona. Actas Dermosifiliogr. 2019;110:841–849.