Ingrown nails are a common problem, seen mostly in young adults. Also known as onychcrypotisis, this condition typically affects the great toenail. Four stages have been defined according to the severity and duration of the condition, and treatment varies from conservative to surgical techniques depending on the stage. We present our experience with this condition, describing the characteristics of our population and surgical treatment, in particular the super U technique.
Material and methodsThis was a retrospective, descriptive study of patients with ingrown great toenail treated surgically using the super U technique. We also describe postoperative management.
ResultsTen patients with a mean age of 35.7 years underwent operation, 9 for unilateral ingrown great toenail and 1 for bilateral disease. Stage II ingrown nail was the most common. Half of the patients had been treated previously using other surgical techniques. The mean time to healing was 6 weeks. The only postoperative complication was infection in 1 patient. Mild to moderate postoperative pain persisted for a week. The majority of patients were satisfied with the cosmetic result.
ConclusionsWe believe the super U technique is very useful in stage II ingrown nail and in disease that has recurred after previous surgery, and is the treatment of choice in stage III or IV disease in which excessive hypertrophic tissue is found.
La onicocriptosis (OC), problema común, afecta principalmente a adultos jóvenes, siendo a menudo el hallux el más afectado. Dependiendo de la gravedad y cronicidad existen 4 estadios, y de estos se derivan distintos tratamientos, abarcando tanto técnicas conservadoras como quirúrgicas. Presentamos nuestra experiencia en esta afección, destacando las características de nuestra población, y dentro de los tratamientos quirúrgicos la técnica de exéresis en U.
Materiales y métodosEstudio retrospectivo y descriptivo de pacientes que presentaron OC a nivel del hallux, que fueron resueltos quirúrgicamente a través de la exéresis en U y su manejo postoperatorio.
ResultadosDe 10 pacientes operados la edad media fue 35,7 años, en donde 9 tenían compromiso de un hallux y uno de ambos. El estadio ii fue el predominante. La mitad había recibido tratamiento quirúrgico previo con una técnica distinta a la exéresis en U. El tiempo de cicatrización promedio fue 6 de semanas. Respecto a las complicaciones, solo un paciente sufrió una infección postoperatoria; y respecto del dolor posquirúrgico este fue leve-moderado, con duración de una semana. La mayoría estaba satisfecha con el resultado estético.
ConclusionesConsideramos que la exéresis en U es una técnica que ha demostrado ser de gran utilidad cuando la OC se encuentra en estadio ii, y/o cuando el paciente ya ha recibido tratamiento quirúrgico que ha fallado. Además, sería de elección en los estadios iii y iv, donde lo que predomina es un exceso de tejido hipertrófico.
Onychocryptosis is a disease of the nail plate in which an abnormal interaction with the nail fold produces ingrowth, causing pain, inflammation, and even recurrent infection.1 With time, a highly vascular and very tender granulation tissue develops, producing marked morbidity, with difficulty walking and even time off work.2,3
Onychocryptosis is a common health problem, accounting for 20 of every 100000 first consultations and 20% of foot problems.1,4–6 It can present at any age, though it is most common between 15 and 40 years, with a male predominance of 3 to 1.4
Based on clinical experience, the great toe is most commonly affected, usually unilaterally, although the condition can be bilateral.1
Onychocryptosis is classified into 4 stages according to the severity and duration of the disease.3,7 In stage 1, the lateral nail fold is tender and presents erythema and mild edema. The nail fold has not grown over the border of the nail plate. Stage 2 is divided into 2 substages: stage 2A, in which symptoms deteriorate and a serous secretion and infection may develop (the nail fold overlaps the surface of the nail but by less than 3mm); and stage 2B, with symptoms similar to those of stage 2A, but the hypertrophic fold overlaps the nail plate by more than 3mm). In stage 3, symptoms become more intense and chronic granulation tissue and hypertrophy of the nail fold develop. The granuloma or hypertrophic tissue covers a large part of the nail surface. Inadequate treatment can lead to further progression, with severe chronic deformity. Finally, stage 4, the result of progression from stage 3, presents greater deformity of the nail plate and folds; stage 4 is differentiated from stage 3 by hypertrophy of the distal nail fold.
Mild, stage 1 disease can be treated medically, while moderate and severe forms (stages 2, 3, and 4) require surgery.8
Two surgical strategies are used: reduction of the nail plate and reduction of the soft tissues of the great toe. The aim in both cases is to optimize the relationship between the nail and the soft tissue. Treatments that aim to reduce nail size include chemical cautery or partial matricectomy with 88% phenol; this is usually the most widely used technique,9 and it consists of partial surgical ablation of the nail plate using a 80% to 95% solution of phenol in distilled water. The solution, applied under local anesthesia, has 3 main actions: necrosis, disinfection, and anesthesia.9,10
Treatments that reduce the soft tissues, such as the Howard-Dubois and VandenBos procedures, are designed to reduce or eliminate excess tissue.9 The super U technique was first described by Dr. Ival Peres Rosa in 1989.11–13 It is used in cases of severe nail-fold hypertrophy and achieves good healing and a good cosmetic result, with low recurrence rates and no risk of infection.13,14
In this article, we report our experience in patients with onychocryptosis treated surgically using the super U technique.
Material and MethodsPatient SelectionWe performed a retrospective descriptive study of patients with onychocryptosis affecting the nail of the great toe and that was resolved surgically using the super U technique.
Patients who had undergone operation in the Dermatologic Surgery Unit of the Dermatology Department of Hospital de Clínicas in Montevideo, Uruguay, between January 2014 and January 2015 were selected. The following surgical and demographic data were gathered from a review of the medical records and an extensive analysis of the photographic documentation: age, sex, stage, unilateral or bilateral involvement of the great toe, time since diagnosis, adherence to treatment, previous surgical treatments before super U excision, healing time, and complications such as bleeding, infection, and postoperative pain. In accordance with the department protocols, patients signed consent forms for surgery and for the use of photographs in scientific publications. Likewise, data from the routine follow-up were obtained from the medical history. Follow-up consultations were scheduled at 24 to 96hours, weekly thereafter up to a month, at 3 months, and at 1 year; consultations were performed by nurses and dermatologists up to a month and subsequently only by dermatologists. Details were recorded of the appearance of the wound, the healing process, time to granulation, and those complications mentioned above.
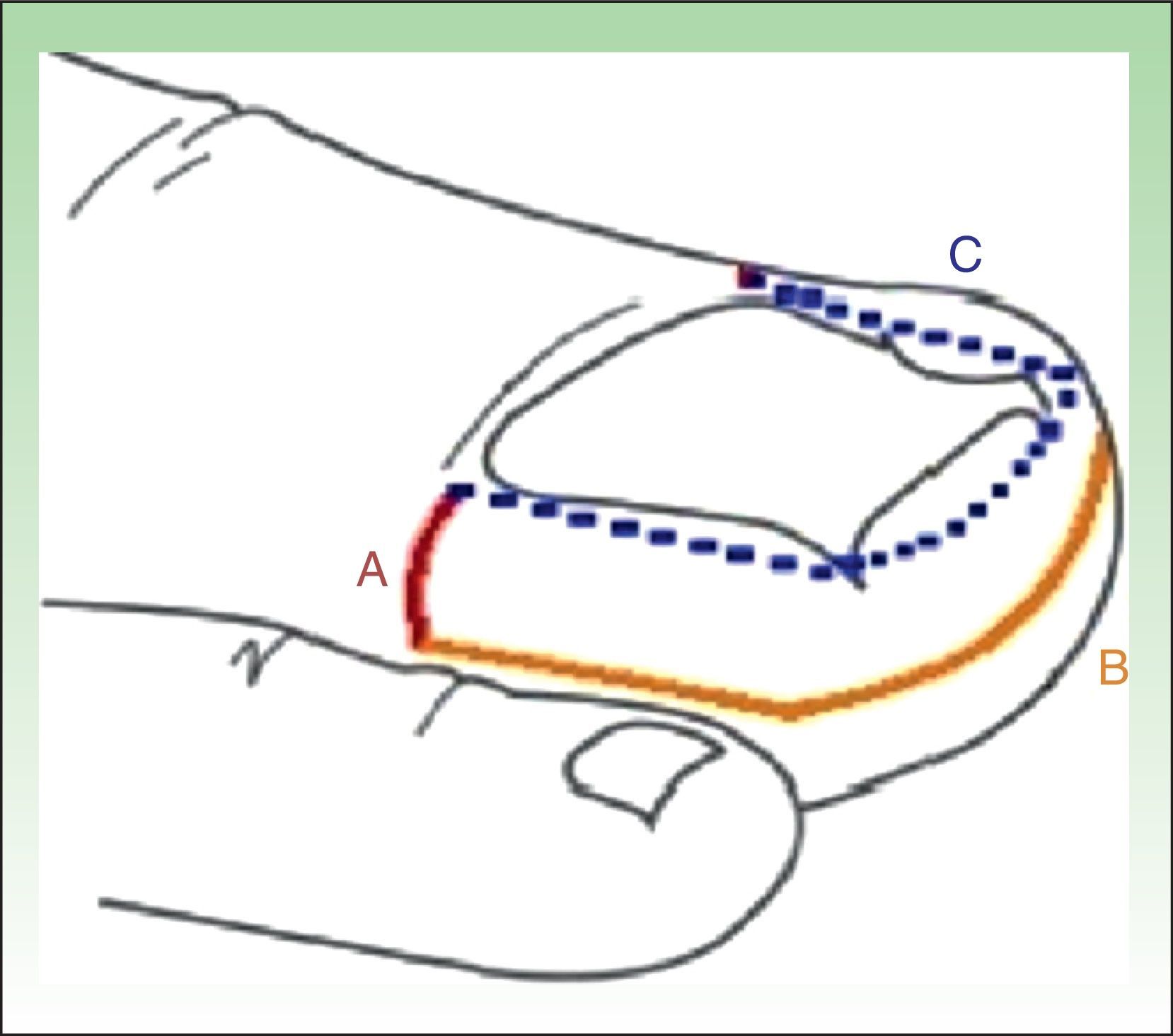
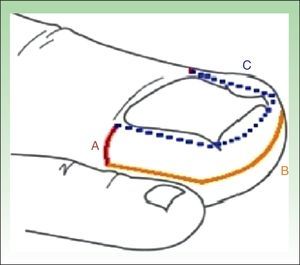
Surgical TechniqueSurgery is performed as an ambulatory procedure. After disinfection of the operating field with alcoholic chlorhexidine solution, nerve block is performed with 2% lidocaine. A tourniquet is then applied to prevent bleeding during exeresis. A dermographic marker is used to outline the U shape of tissue to be excised. The technique consists of a transverse incision on each side of the nail, extending from the extremes of the proximal nail fold to the most distal point of hypertrophic tissue (Fig. 1 LineA). A second incision is then made perpendicular to the first incision, starting from the end of that incision and running parallel to the lateral nail fold, continuing parallel to the distal fold around the tip of the toe to reach the contralateral surface, and ending at the end of the first incision on the opposite side (Fig. 1 LineB).
Line A runs transversely from the end of the proximal nail fold the end of the cuticle to the lateral limit of the hypertrophic tissue. Line B starts perpendicular to the first incision and runs parallel to the lateral and distal nail folds, ending at the same point on the opposite side. Line C (dashed) marks the area to be excised to complete the super U excision.
To complete excision of the hypertrophic tissue between the borders of the nail and the lines shown in Figure1 (lines A and B), the tissue is separated along line C of Figure1 and is cut with scissors, including part of the fatty tissue. It is important to preserve sufficient fatty tissue to cover the phalanx, as this reduces postoperative pain and discomfort.13
When necessary, hemostasis is performed by sutures along the free border of the skin (Fig. 2 A-F), although the use calcium alginate as a hemostatic agent now makes sutures unnecessary. An extra-thin hydrocolloid dressing is used to cover the area, which is then protected with gauze swabs.
Postoperative ManagementAt 5 days, a new extra-thin hydrocolloid dressing is applied, and this process is repeated every 5 to 7 days until sufficient granulation tissue has developed to restore the contour of the great toe.
The formation of granulation tissue must be monitored to see that it fills the space up to the level of the nail plate; if overlap occurs, topical silver nitrate is applied to sculpture the soft tissue, and this process is repeated until epithelialization is complete. Antibiotics and analgesics are prescribed as necessary.
Granulation tissue formation, exudate, and pain control using a visual analog scale (VAS) were recorded at each routine weekly follow-up visit.
For this study, when the report of the annual follow-up consultation in the medical history did not describe the cosmetic appearance or the presence or absence of recurrence, the patient was contacted by telephone to clarify these points. Patients were asked to compare the cosmetic appearance before and after surgery and to state whether they found the situation satisfactory or unsatisfactory.
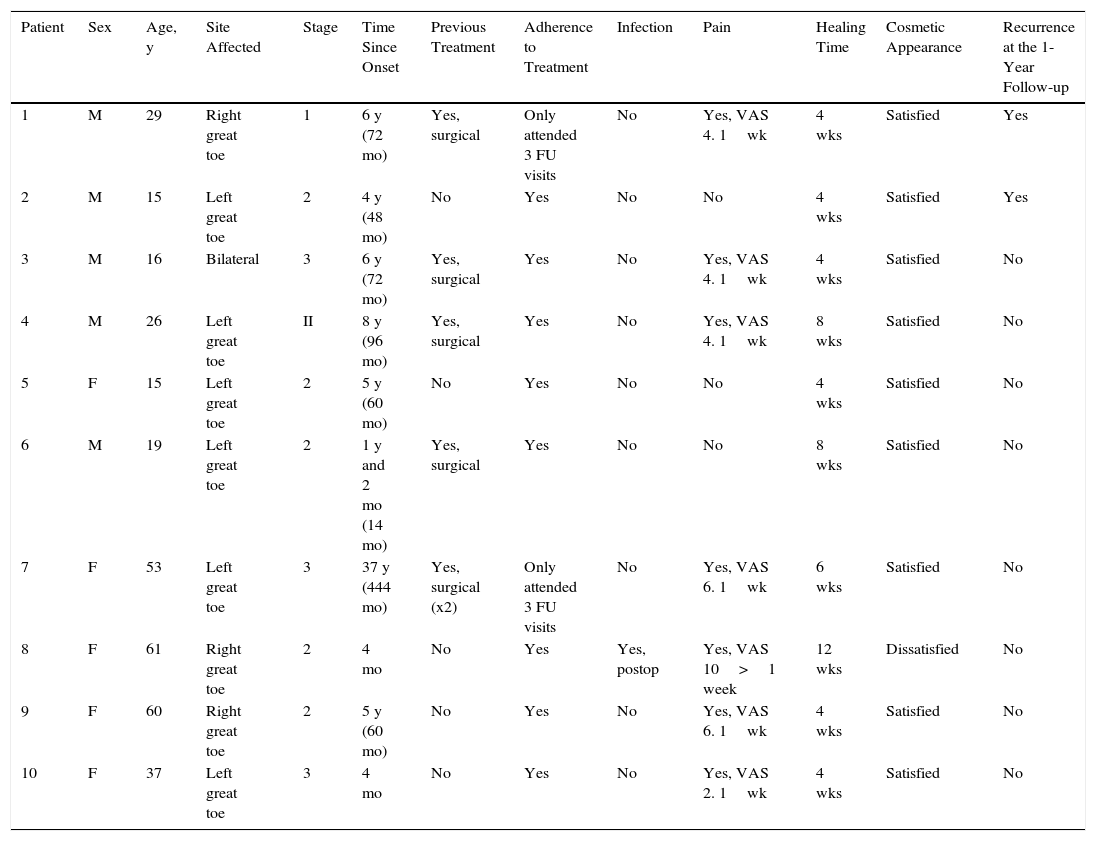
ResultsBetween January 2014 and January 2015, 10 patients (5 men and 5 women) aged between 15 and 61 years (mean age, 35.7 years) underwent surgery for onychocryptosis in the dermatology department using the super U technique (Table 1)
Epidemiological Characteristics of the Patients and Response to Treatment.
| Patient | Sex | Age, y | Site Affected | Stage | Time Since Onset | Previous Treatment | Adherence to Treatment | Infection | Pain | Healing Time | Cosmetic Appearance | Recurrence at the 1-Year Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 29 | Right great toe | 1 | 6 y (72 mo) | Yes, surgical | Only attended 3 FU visits | No | Yes, VAS 4. 1wk | 4 wks | Satisfied | Yes |
| 2 | M | 15 | Left great toe | 2 | 4 y (48 mo) | No | Yes | No | No | 4 wks | Satisfied | Yes |
| 3 | M | 16 | Bilateral | 3 | 6 y (72 mo) | Yes, surgical | Yes | No | Yes, VAS 4. 1wk | 4 wks | Satisfied | No |
| 4 | M | 26 | Left great toe | II | 8 y (96 mo) | Yes, surgical | Yes | No | Yes, VAS 4. 1wk | 8 wks | Satisfied | No |
| 5 | F | 15 | Left great toe | 2 | 5 y (60 mo) | No | Yes | No | No | 4 wks | Satisfied | No |
| 6 | M | 19 | Left great toe | 2 | 1 y and 2 mo (14 mo) | Yes, surgical | Yes | No | No | 8 wks | Satisfied | No |
| 7 | F | 53 | Left great toe | 3 | 37 y (444 mo) | Yes, surgical (x2) | Only attended 3 FU visits | No | Yes, VAS 6. 1wk | 6 wks | Satisfied | No |
| 8 | F | 61 | Right great toe | 2 | 4 mo | No | Yes | Yes, postop | Yes, VAS 10>1 week | 12 wks | Dissatisfied | No |
| 9 | F | 60 | Right great toe | 2 | 5 y (60 mo) | No | Yes | No | Yes, VAS 6. 1wk | 4 wks | Satisfied | No |
| 10 | F | 37 | Left great toe | 3 | 4 mo | No | Yes | No | Yes, VAS 2. 1wk | 4 wks | Satisfied | No |
Abbreviations: F, female; FU, follow-up; M, male.
Only 1 patient had bilateral disease (Fig. 3). The severity of onychocryptosis, based on the staging classification, was stage 1 in 1 patient, stage 2 in 6, and stage 3 in 3. No patients presented stage 4 disease.
Patient 3. Bilateral stage 3 disease. A, Right great toe. B, Left great toe: A dermographic marker is used to outline the tissue to be excised. C, Intraoperative image after U excision of the periungual granulation tissue. D, Four weeks after surgery, silver nitrate is still visible on the nail plate.
The mean time between onset of the disease and treatment using the super U technique was 87 months (range, 4–444 months).
Half of patients had undergone previous surgery of their onychocryptosis using other surgical techniques.
A total of 6 follow-up visits were performed; 2 patients only attended 3 of these visits. Mean time to healing was 6 weeks.
Complications were only observed in 1 patient, who developed postoperative infection requiring treatment with systemic antibiotics. Pain was evaluated at the follow-up visits using a VAS. Seven of the 10 patients reported pain during the week after surgery, with a mean VAS score of 5 in 6 of them. Only 1 patient reported maximum pain for more than a week, related, in this case, to preoperative bone changes and not to the surgical technique.
Nine of the 10 patients were satisfied with the cosmetic appearance evaluated at the follow-up visit at 1 year.
Two patients presented recurrence prior to the 1-year follow-up visit.
DiscussionVarious treatments are available for onychocryptosis, from conservative management to complex surgical procedures that require considerable experience.10 Surgery must be considered in cases with pain, recurrent onychocryptosis, surgical recurrence, onychogryposis, chronic recurrent paronychia, or failure of conservative management.7 Management should be conservative in patients with stage 1 disease.3,8 The super U technique can be used in patients with disease in stage 1 or 2 that recurs after treatment, though recognizing that this is an aggressive procedure compared with other existing techniques. The patient with stage 1 disease in our series presented recurrence and severe pain after previous surgery.
According to the literature, partial matricectomy with phenol is more often used in stages 1 and 2A.4 Phenol matricectomy is a rapid, simple, and inexpensive technique. Inflammation and wound healing persist for at least 2 to 3 weeks, with full recovery a month after treatment.10
Recurrence occurs in up to 24%,3,10 probably caused by incomplete matricectomy, with new nail growth in the lateral fold.9 The main disadvantage is that the nail is narrower, typically producing a poor cosmetic result.15
The Howard-Dubois procedure consists of a fish-mouth incision running below and parallel to the lateral and distal nail folds, accompanied by a second incision to create a wedge in the center of the distal wall, with subsequent excision of the crescent of tissue. This technique is considered best for mild to moderate cases, while the super U technique is the best option for severe disease in stage 3 or 4.9 The results are good with both techniques, but the Howard-Dubois operation can lead to necrosis of the wound margins if excessive tissue is removed in cases with moderately hypertrophic lateral folds; this does not occur with the super U technique. In addition, the Howard-Dubois procedure is very painful, requiring good analgesic control.9 Another technique similar to the super U procedure is the one described by Vandenbos. The differences between the 2 procedures are that the proximal part of the incision in the super U technique does not include the proximal nail fold, the distal fold is excised, and hemostasis is achieved using a running lock suture.9,13,14
In our series of 10 patients undergoing the super U procedure, the majority stated they were satisfied with the operation, and recurrence and complication rates were low. We therefore consider that this technique achieved excellent resolution of the disease in almost all our patients.
It is important to draw attention to the patients in who previous treatments had been unsuccessful using techniques distinct from the super U procedure. Of these patients, 4 showed an excellent response to the new procedure, with mild to moderate pain of short duration, an absence of infection, and satisfaction with the cosmetic result. In patients with a long history of the disease or who have undergone previous surgical treatments, the super U procedure therefore appears to be an effective option.
With respect to patients with more advanced disease (stage 3), super U excision is seen as a good option, as the clinical course in all our patients was excellent, with no recurrences or complications.
Another relevant point is postoperative follow-up, especially to control granulation tissue formation and to prevent its hypertrophy by using topical silver nitrate. The super U technique requires very strict nursing control, which is usually complete within 30 to 45 days.
Comparing the results in our patients using the super U technique described by Dr. Peres Rosa, with the results described in the literature for partial matricectomy with phenol,3,5,6,10 we can conclude that both techniques have been shown to be safe, simple, and effective. Both procedures have a low recurrence rate and a relatively similar postoperative recovery, though time to healing is shorter with partial matricectomy with 88% phenol. However, the super U technique preserves the whole nail, adapting the soft tissues of the great toe to the nail, leading to a much better cosmetic result than with matricectomy.
Our study is limited by the small number of patients. No studies designed to compare the super U technique with any other type of surgery have yet been published.
It is very difficult to select a treatment for onychocryptosis that satisfies all patient characteristics and requirements, and more so when resolution of the disease varies with its duration.
Based on our experience and the results of the study presented, we consider that the super U procedure is a very useful technique. It is the best option for severe onychocryptosis that presents hypertrophy of the lateral and distal nail folds, and for stage 2 disease in which previous treatments have failed.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this research.
Confidentiality of dataThe authors declare that they followed their hospital's regulations regarding the publication of patient information.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Correa J. Exéresis en U para la onicocriptosis. Actas Dermosifiliogr. 2017;108:438–444.