Erosive pustular dermatosis of the scalp is a rare inflammatory skin disease that mainly affects older patients and is characterized by the presence of sterile pustules and scabs. Recently, several authors have reported the usefulness of photodynamic therapy in the treatment of this condition.1
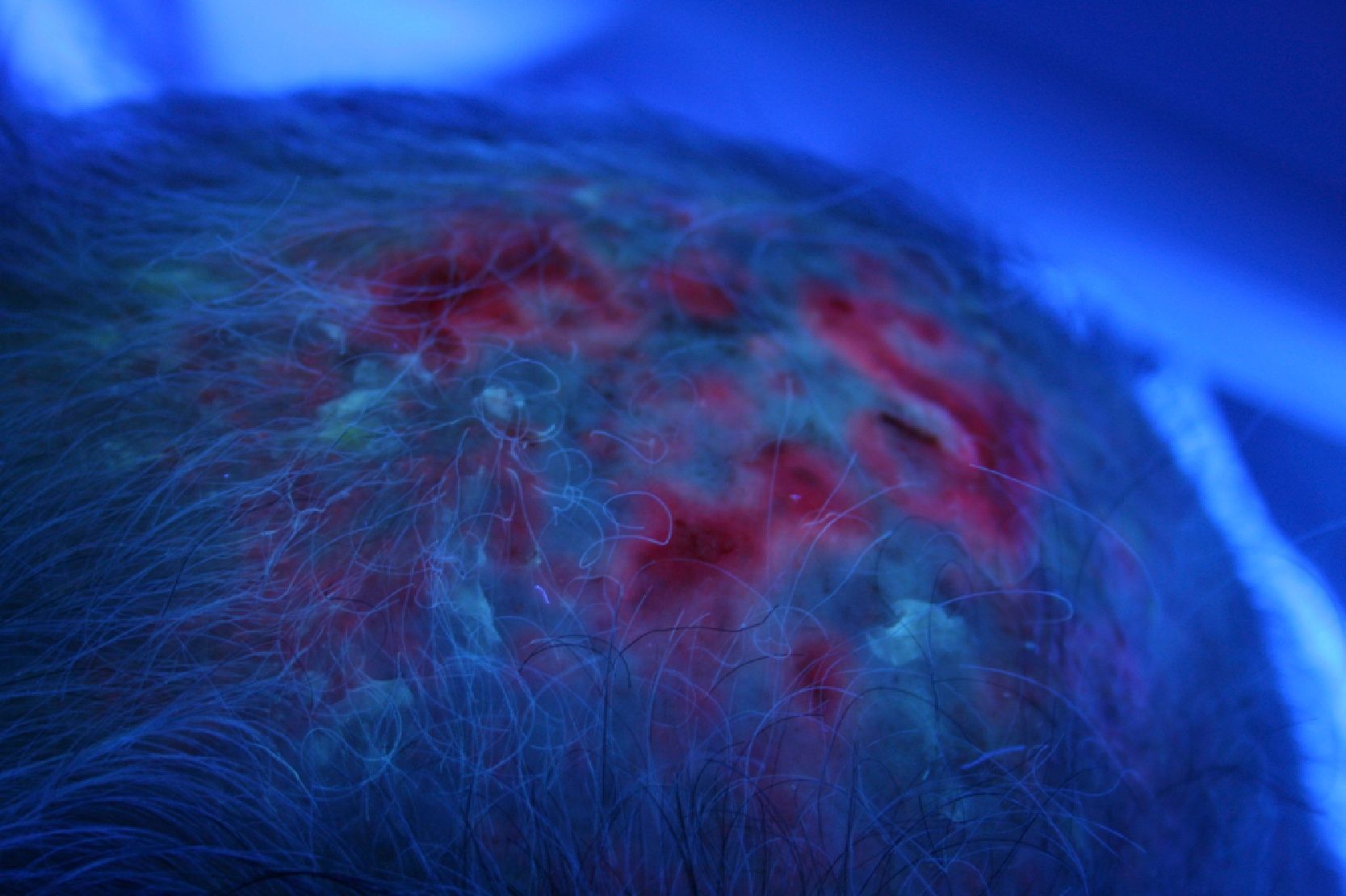
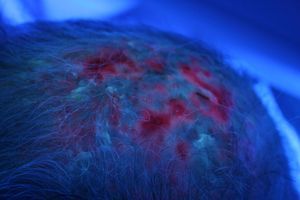
We present the case of a 79-year-old man with skin phototype III and actinic keratosis of the face and scalp, occasionally treated with cryotherapy, after which the patient would complain of painful erosions in the treated area. On one of his check-up visits he had an outbreak of pustules and scabs that mainly affected the posterior part of the parietal region. The pustules had an erythematous base, and painful erosions and scabs were also visible. Biopsy revealed areas of fibrosis, a predominantly perifollicular neutrophil infiltrate, and areas of scarring. The diagnosis was erosive pustular dermatosis of the scalp, which responded favorably to topical treatment with fusidic acid plus betamethasone cream and healed with scarring alopecia. Thereafter, actinic keratoses in this patient were successfully treated with topical imiquimod to prevent outbreaks of pustulosis. During follow-up, however, he presented with hypertrophic actinic keratoses in the occipital region and numerous pustules that coalesced into lakes of pus (Fig. 1). These actinic keratoses did not respond to imiquimod and the erosive pustular dermatosis of the scalp worsened with the use of this agent. It was then decided to try treatment with photodynamic therapy (PDT). At the first session, curettage of the most hypertrophic actinic keratoses was performed and this was followed by an application of Metvix® (160mg/g methyl aminolevulinate hydrochloride cream; manufactured by Penn Pharmaceutical Services Ltd, distributed by Galderma) under occlusion for 3hours. Wood light showed intense uptake in the area (Fig. 2), which was then infiltrated with local anesthetic. Irradiation was by red light (Aktilite CL128, Photocure ASA, Oslo, Norway) at a wavelength of 630 nm, with a fluence of 37J/cm2. A good response was observed after a week but several actinic keratoses and pustules still remained. A second session 3 weeks later cleared the actinic keratoses and the erosive pustular dermatosis of the scalp was rendered inactive (Fig. 3). Six months later, the improvement in the treated area was maintained and the patient is currently awaiting a further session on the occipital region to treat new actinic keratoses.
Erosive pustular dermatoses are rare inflammatory skin diseases of unknown origin that typically arise either on the legs or on the scalp. Erosive pustular dermatosis of the scalp mainly affects older patients. It is characterized by confluent sterile pustules, erosions, and scabs on the scalp that heal with scarring alopecia. Factors such as local trauma, cryotherapy, and radiotherapy1 can trigger or worsen this condition. The differential diagnosis includes bacterial folliculitis, inflammatory tinea, blistering diseases such as cicatricial pemphigoid, dissecting cellulitis, and pyoderma gangrenosum.1,2 Treatment is complex and the disease tends to recur. Medium- to high-potency topical corticosteroids have been used successfully, sometimes in conjunction with a topical antibiotic. Topical tacrolimus can also be effective3 and prevents the adverse effects of long-term topical corticosteroid therapy. Other treatments include oral corticosteroids, dapsone, oral retinoids (isotretinoin), and topical calcipotriol. In our patient, treatment of actinic keratoses with cryotherapy probably worsened the erosive pustular dermatosis of the scalp, and cryotherapy was therefore avoided after this second diagnosis was made.
PDT is a well-established treatment for actinic keratoses and other premalignant or malignant conditions.4 It is particularly useful for the treatment of actinic keratoses in patients with multiple lesions or frequent recurrences. There is evidence of the value of PDT in erosive pustular dermatosis of the scalp,1,2 attributed to its immunomodulatory effect on inflammatory cells.5 Meyer et al1 reported the case of a 75-year-old woman with erosive pustular dermatosis of the scalp successfully treated with PDT. Recently, Eleftheriou et al2 published a case similar to ours of a 72-year-old man with actinic keratoses and underlying erosive pustular dermatosis of the scalp. Two sessions of PDT separated by 12 weeks led to resolution of the lesions. However, Guarneri et al6 described the case of a 93-year-old woman who had an outbreak of erosive pustular dermatosis of the scalp after 2 sessions of PDT for actinic keratoses in the same area. Their patient received a higher fluence than ours (75J/cm2 compared to 37J/cm2, respectively), and this may have resulted in the appearance of erosive pustular dermatosis of the scalp.
We report a patient with erosive pustular dermatosis of the scalp and multiple hypertrophic actinic keratoses on the scalp; both conditions responded to treatment with PDT. Two sessions of PDT led to considerable improvement, which was maintained at the 6-month follow-up. Experience of using PDT in inflammatory dermatoses like erosive pustular dermatosis of the scalp is limited, but our case provides more evidence that it can be a good therapeutic option for a disorder that is difficult to manage.
Please cite this article as: Monteagudo AF, et al. Respuesta a terapia fotodinámica en paciente con der-matosis pustulosa del cuero cabelludo y queratosis actínicas hipertróficas. Actas Dermosifiliogr. 2013;104:351–2.