Hailey-Hailey disease or familial benign pemphigus is a rare hereditary skin disease. This chronic and recurrent condition can cause severe discomfort and be difficult to control with conventional treatments. Photodynamic therapy (PDT) could offer an alternative in cases in which other treatment options have failed.
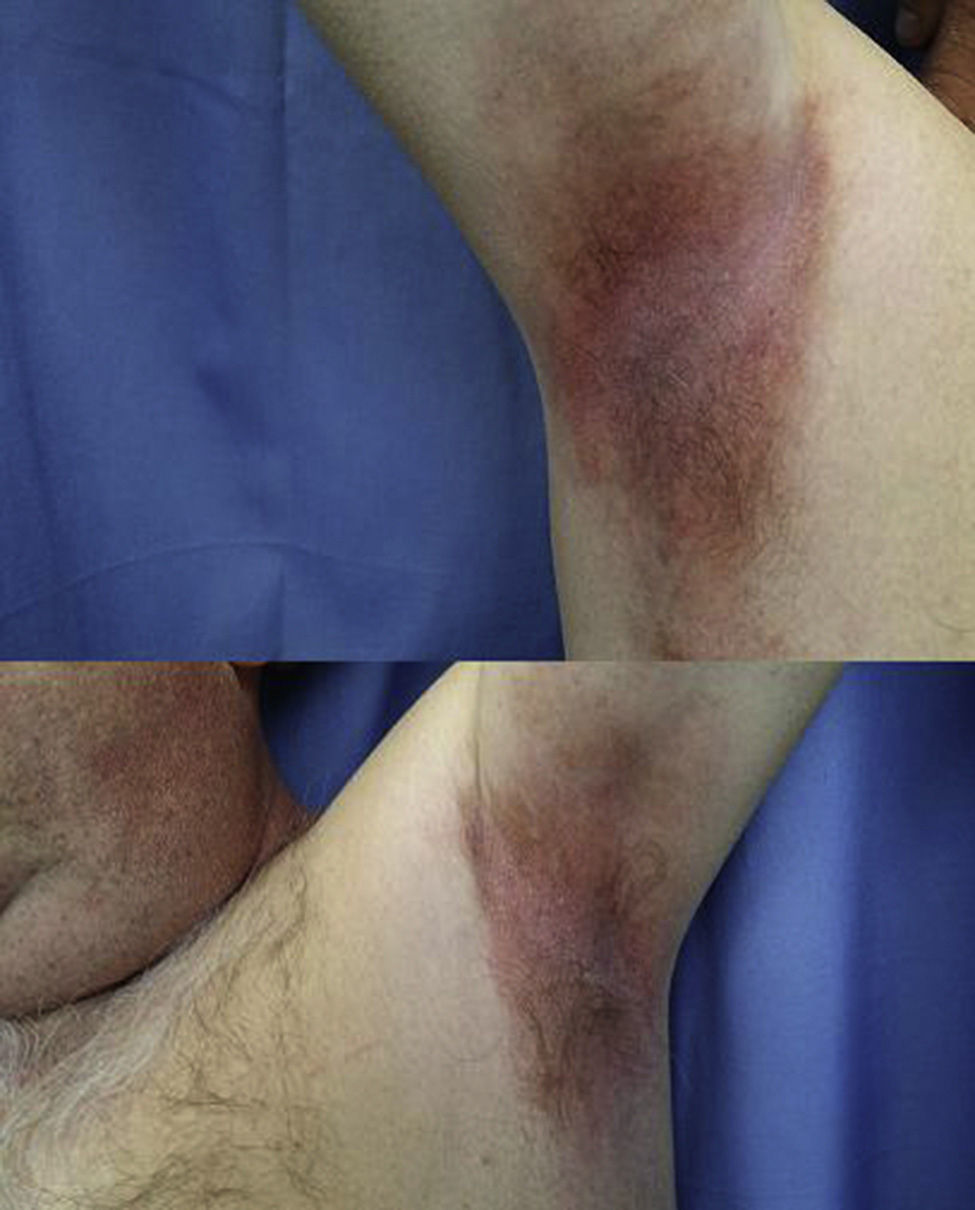
The patient was a 56-year-old male who for 30 years had experienced several outbreaks a year of stinging, itching, and burning lesions located on the neck and armpits. The lesions interfered with his daily activities and had a negative impact on his quality of life. Physical examination revealed bright, well-defined, highly exudative, eroded, and erythematous plaques with some surface crusts located in both armpits and on the lateral aspects of the neck (Fig. 1). Histological study of a biopsied sample from one of the lesions demonstrated an epidermis with erosions and intraepidermal blisters, marked acantholysis, and the typical appearance of a dilapidated brick wall. The patient had been diagnosed with Hailey-Hailey disease and had received multiple treatments with astringents such as copper and zinc sulfate (1:1000), topical and systemic steroids, topical vitamin D derivatives, topical tacrolimus, and acitretin. Response to treatment had always been partial with a disease-free interval between flares lasting only a few weeks. These shortcomings represented an important limitation for the patient. He agreed to undergo a single session of PDT to see what the response would be and to assess the tolerability of the treatment. First, both underarms were cleaned with physiological saline solution and methyl aminolevulinate (MAL) cream was applied under occlusion for 3hours. The underarms were then irradiated with a red light (Aktilite at 37J/cm2) for 7.5 minutes. During the period of exposure, the patient experienced a slight sensation of pain and burning, which was well tolerated. The response on follow-up at 2 weeks was excellent: the erosions had healed, the exudate and erythema had disappeared, and the patient reported an improvement in his quality of life (Fig. 2). Six months later, the patient is still free of lesions and has not undergone any other treatment.
Hailey-Hailey disease or familial benign pemphigus is an autosomal dominant genodermatosis caused by a mutation in the ATP2C1 gene. It is characterized by the appearance of vesicles, blisters, and erosions in flexural areas, including the neck and axillas as well as the inframammary and inguinal folds. Typically, patients experience recurrent flares and, occasionally, spontaneous remission. Among the best known precipitating factors are exposure to UV light, sweat, friction, stress, skin infections, and pregnancy.1
Many treatments have been used to control the disease with varying results. Medical treatments include topical and systemic corticosteroids, topical and systemic antibiotics, topical vitamin D analogs, topical 5-fluorouracil, dapsone, psoralen and UV-A light therapy, systemic retinoids, ciclosporin, methotrexate, and oral glycopyrrolate.2,3 A number of invasive treatments have been attempted, including infiltration with botulinum toxin,4 carbon dioxide laser,5,6 erbium: yttrium aluminium garnet laser, and dermabrasion.
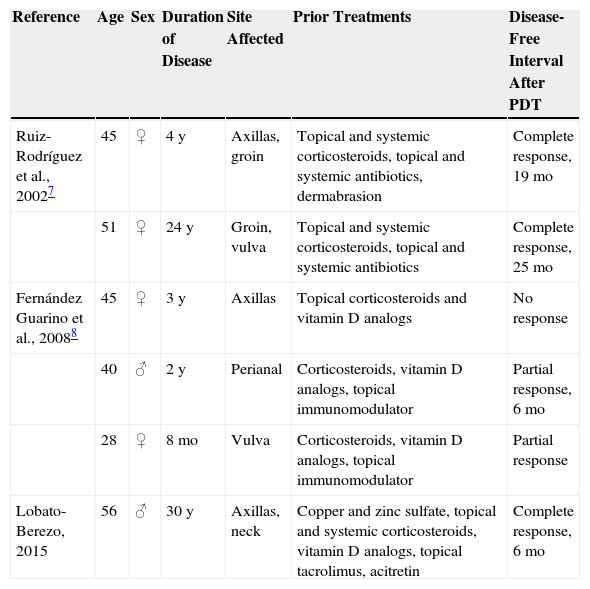
In the literature, we found only 2 articles (referring to 5 patients) on Hailey-Hailey disease treated with PDT (Table 1). The age of the 5 patients ranged from 28 to 51 years and all but one were women. The time elapsed since diagnosis ranged from 8 months to 24 years, and all 5 patients had undergone prior treatment with topical corticosteroids and a topical vitamin D analog or an antibiotic. Two of the patients had a complete response followed by a disease-free interval of 19 and 25 months, respectively; a further 2 patients showed partial improvement of their lesions, and the remaining patient did not improve.7,8 In the cases reported by Ruiz-Rodriguez et al.7 PDT was well tolerated because lidocaine 1% was administered in the treatment site as a local anesthetic. By contrast, the 3 patients reported by Fernández-Guarinoet al.8 experienced pain, erythema and/or edema during and after treatment and none of them wished to undergo another PDT session. Topical anesthetics could interfere with the effectiveness of PDT treatment because they have an alkaline pH that destabilizes the aminolevulinic acid.8 It remains unclear why patients with Hailey-Hailey disease improve with PDT, but the good response is thought to be due to intracellular accumulation of protoporphyrin IX in epidermal keratinocytes, which interferes with structures such as mitochondria, lysosomes, and endoplasmic reticulum.7
Cases of Hailey-Hailey Disease Treated with Photodynamic Therapy.
| Reference | Age | Sex | Duration of Disease | Site Affected | Prior Treatments | Disease-Free Interval After PDT |
|---|---|---|---|---|---|---|
| Ruiz-Rodríguez et al., 20027 | 45 | ♀ | 4 y | Axillas, groin | Topical and systemic corticosteroids, topical and systemic antibiotics, dermabrasion | Complete response, 19 mo |
| 51 | ♀ | 24 y | Groin, vulva | Topical and systemic corticosteroids, topical and systemic antibiotics | Complete response, 25 mo | |
| Fernández Guarino et al., 20088 | 45 | ♀ | 3 y | Axillas | Topical corticosteroids and vitamin D analogs | No response |
| 40 | ♂ | 2 y | Perianal | Corticosteroids, vitamin D analogs, topical immunomodulator | Partial response, 6 mo | |
| 28 | ♀ | 8 mo | Vulva | Corticosteroids, vitamin D analogs, topical immunomodulator | Partial response | |
| Lobato-Berezo, 2015 | 56 | ♂ | 30 y | Axillas, neck | Copper and zinc sulfate, topical and systemic corticosteroids, vitamin D analogs, topical tacrolimus, acitretin | Complete response, 6 mo |
Providing it is tolerated, PDT may represent an alternative treatment option in cases of Hailey-Hailey disease refractory to first-line therapies, since durable remissions can be achieved that can improve the patient's quality of life.
Please cite this article as: Lobato-Berezo A, Imbernón-Moya A, Aguilar-Martínez A. Enfermedad de Hailey-Hailey recalcitrante con buena respuesta a terapia fotodinámica. Actas Dermosifiliogr. 2015;106:852–854.