We describe a patient with primary cutaneous small-to-medium–sized CD4+ T-cell lymphoma, according to the most recent World Health Organization (WHO) classification of cutaneous lymphomas.1
This lymphoma, previously known as primary cutaneous small-to-medium-sized pleomorphic CD4+ T-cell lymphoma,1 has a low incidence and good prognosis. The interest in the case presented in this report derives from a substantial granulomatous component in the clinical-pathological study and the self-healing nature of the lesion. We discuss the possibility of a relationship between these 2 characteristics.
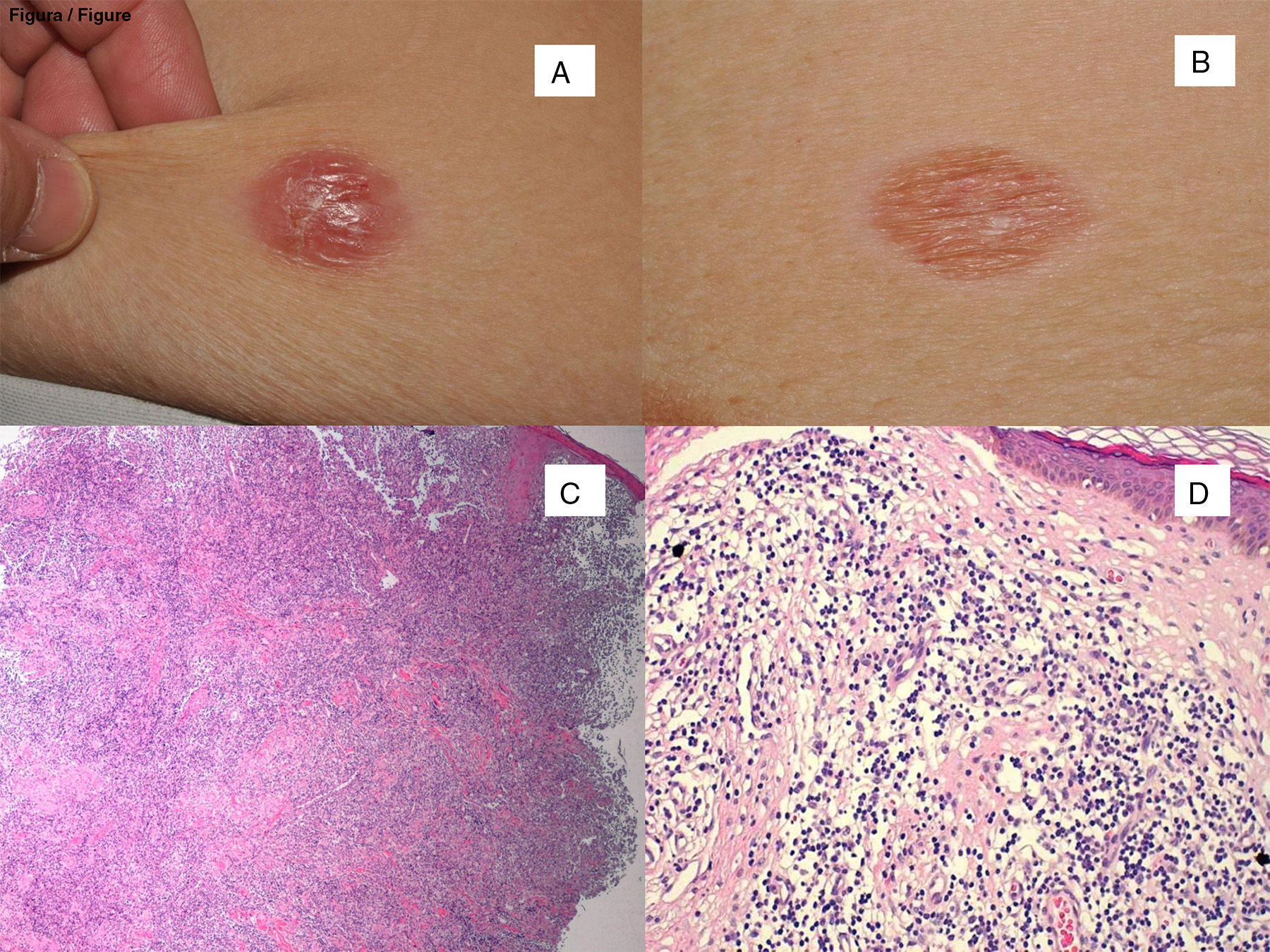
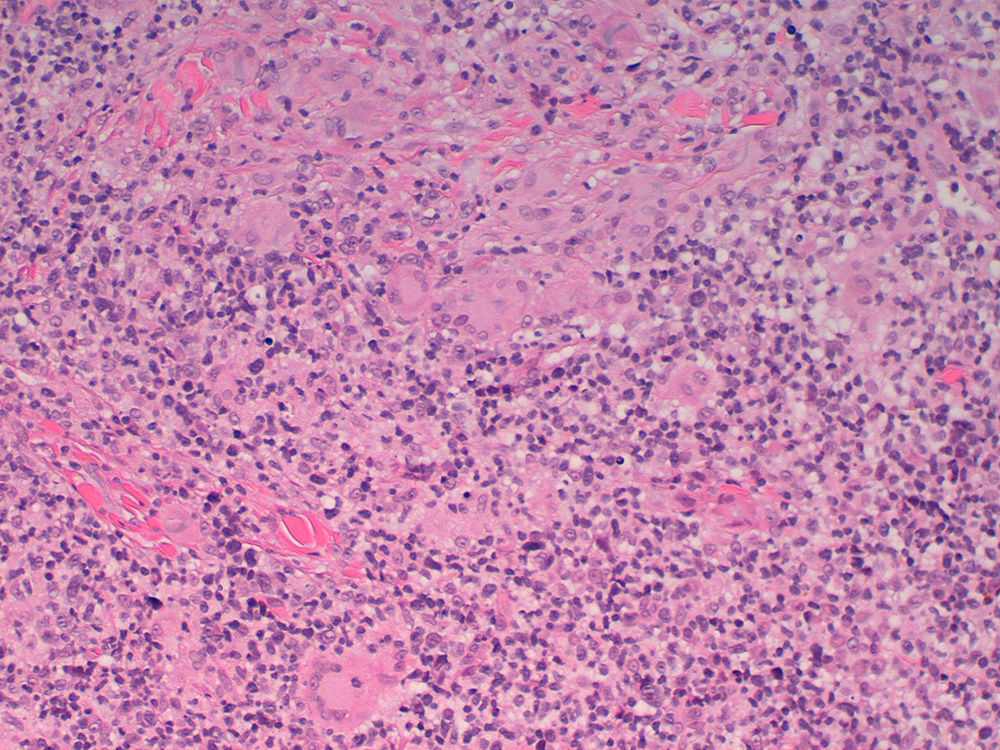
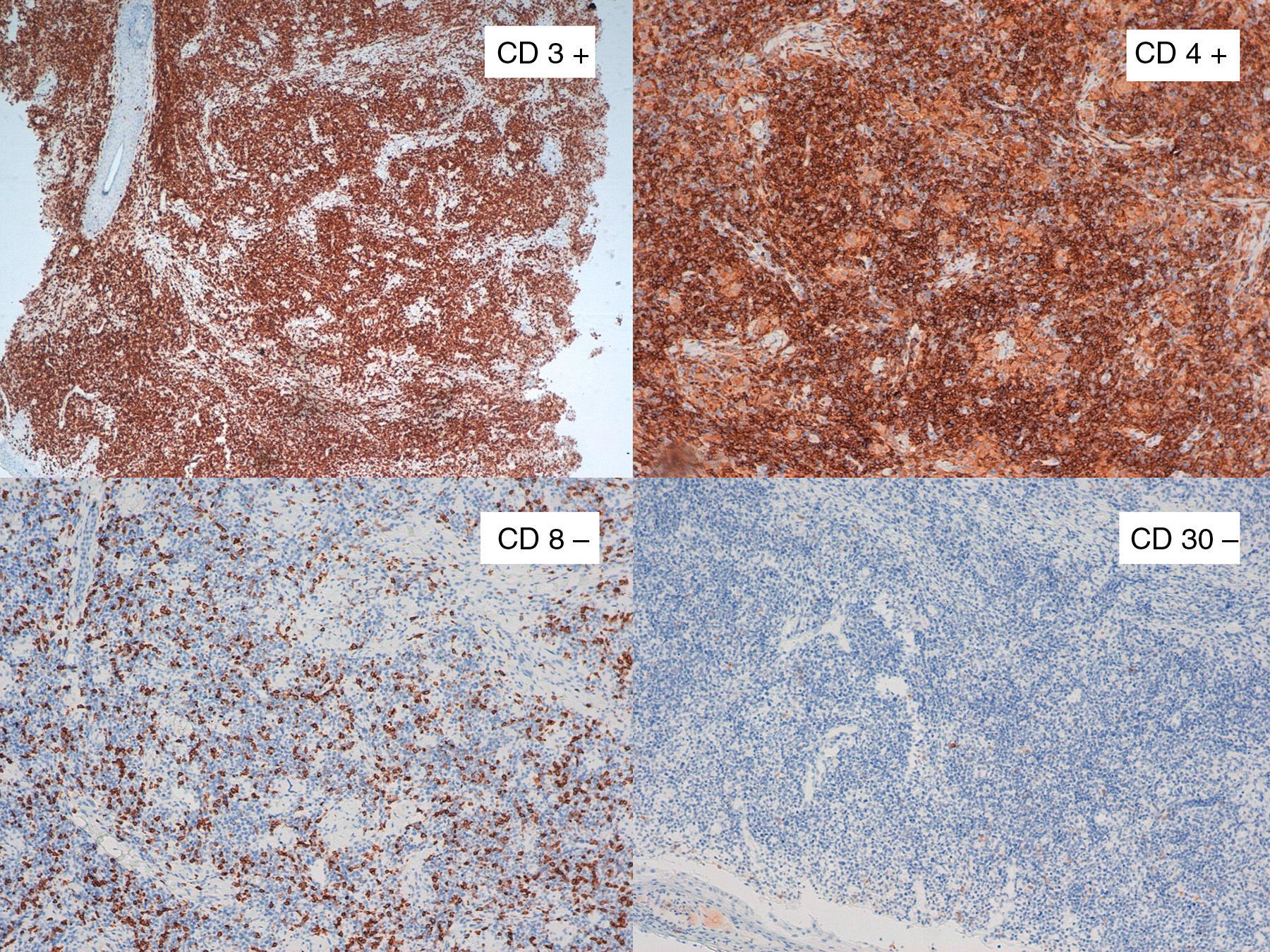
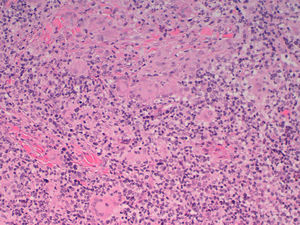
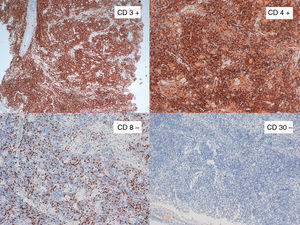
The patient was a 32-year-old woman with no clinical history of relevance who attended the clinic in December, 2012, due to a cutaneous lesion on the right breast related to an insect bite 3 months earlier. The lesion consisted of an itchy erythematous nodule measuring 2cm in diameter with a smooth surface (Fig. 1). Biopsy showed a dense and diffuse infiltrate that occupied the entire thickness of the dermis, composed of small and medium sized cells alongside some eosinophils (Fig. 1). Epidermotropism was scarce. Abundant histiocytes and multinucleated giant cells were also observed, forming granulomatous aggregates (Fig. 2), interspersed with lymphoid proliferation. Immunohistochemistry showed CD3+ and CD4+ cells that were however negative for CD8 and CD30 (Fig. 3). Molecular study of the λ chain of the T-cell receptor showed monoclonal rearrangement, and so the patient was diagnosed with primary cutaneous granulomatous small-to-medium sized CD4+ T-cell lymphoma. An extension study was conducted, including study with lymphoid subpopulations, LDH, β2-microglobulin, and positron emission tomography-computed tomography, with normal results. Surgical resection was proposed. On the day of surgery, 2 months later, the nodule had disappeared to leave a residual erythematous macule (Fig. 1). Excision biopsy of the lesion showed a considerable reduction in lymphoid infiltrate, but this remained positive for CD20, CD3, and CD68, with predominance of CD4 over CD8; the infiltrate was negative for CD30. The same monoclonal pattern persisted.
Clinical images of the lesion. A, At the first visit. B, 2 months later, with self-resolution. Histological appearance of the biopsies corresponding to the clinical images immediately above, with partial reduction of the tumor infiltrate in the second of them. C, Hematoxylin-eosin (H-E), x40. D, H-E, x400.
The patient is still in follow-up in our department and is disease free after 2 years.
Primary cutaneous small-to-medium-sized CD4+ T-cell lymphoma is a rare T-cell lymphoid proliferation that usually presents as a single lesion on the head or trunk and whose histology findings coincide with the case described.2,3 Prognosis is good, with 5-year survival of 80%, with good response to chemotherapy or surgery. In aggressive cases, with multiple lesions, polychemotherapy such as CHOP is used.
The association of cutaneous lymphoma and granuloma is rare although well known. The presence of lymphoma and granuloma in biopsy can lead to erroneous diagnosis and enable the disease to progress undetected for months.4
In the literature review, this phenomenon occurs most frequently in mycosis fungoides and its clinical variant granulomatous slack skin,5 but there have also been isolated reports in Sézary syndrome,6,7 anaplastic CD30+ lymphoma,8 panniculitis-type T lymphoma,8 follicle center lymphoma,8 and in 4 cases of primary cutaneous small-to-medium–sized CD4+ T-cell lymphoma.8 A lymphoma is considered granulomatous when the granulomas occupy at least 25% of the infiltrate.9 This finding occurs in 1.8% of all cutaneous lymphomas.
It is not known whether the granuloma occurs as an immune response of the host to tumor cells or is a result of cytokine release, contributing to better prognosis. Beltraminelli et al.2 went as far as to suggest that small granulomas could be secondary to destruction of skin appendages.
The extent to which this immune reaction could influence the prognosis of lymphoma has also not been established. Granulomatous cutaneous lymphomas normally have a slowly progressive course, although around 50% develop nodal lymphomas with a fatal outcome.
The incongruence between histological findings (pleomorphism, appendage destruction, T-cell monoclonality) and the favorable clinical outcome with a high percentage of remissions seems paradoxic. Histology and immunohistochemistry are, for the time being, not helpful in this case. The monoclonality found in the infiltrate is suggestive of a malign lymphoproliferative process but this finding is not exclusive as reactive inflammatory processes and other processes of unknown significance can also be monoclonal.2 The pattern of PD-1 immuno expression, which we could not determine in our case, may have helped in the diagnosis of primary cutaneous small-to-medium-sized CD4+ T-cell lymphoma.10
Patients with solitary lesions usually have an indolent course. Aggressive treatments should be avoided and these patients should be managed differently to those with multiple cutaneous lesions, in whom prognosis may not be favorable.
In summary, we describe a case of granulomatous primary cutaneous small-to-medium–sized CD4+ T-cell lymphoma with partial self-resolution. The lymphoma has remained in complete remission after surgical excision. Although the presence of granulomas in the histology may hinder diagnosis of the primary tumor,9 and enable its progression, in other cases it may be a true host-versus-tumor reaction and favor self-resolution.
Please cite this article as: García de la Fuente MR, Vilardell-Villellas F, Martí-Laborda RM, Casanova-Seuma JM. Linfoma cutáneo primario T CD4+ de célula pequeña/mediana, granulomatoso. Actas Dermosifiliogr. 2016;107:89–91.