Skin metastases in thyroid cancer are rare, and when they do occur most are associated with follicular carcinoma. They tend to appear in well-vascularized regions such as the scalp, and without predilection for sex.
A 58-year-old woman with no history of interest presented with a follicular variant of stage iv papillary thyroid carcinoma, with extrathyroidal pulmonary and bone involvement. After total thyroidectomy, she received 4 doses of radioactive iodine and hormonal suppression with levothyroxine. Despite treatment every 6 months with I131, response was limited and metastatic uptake persisted.
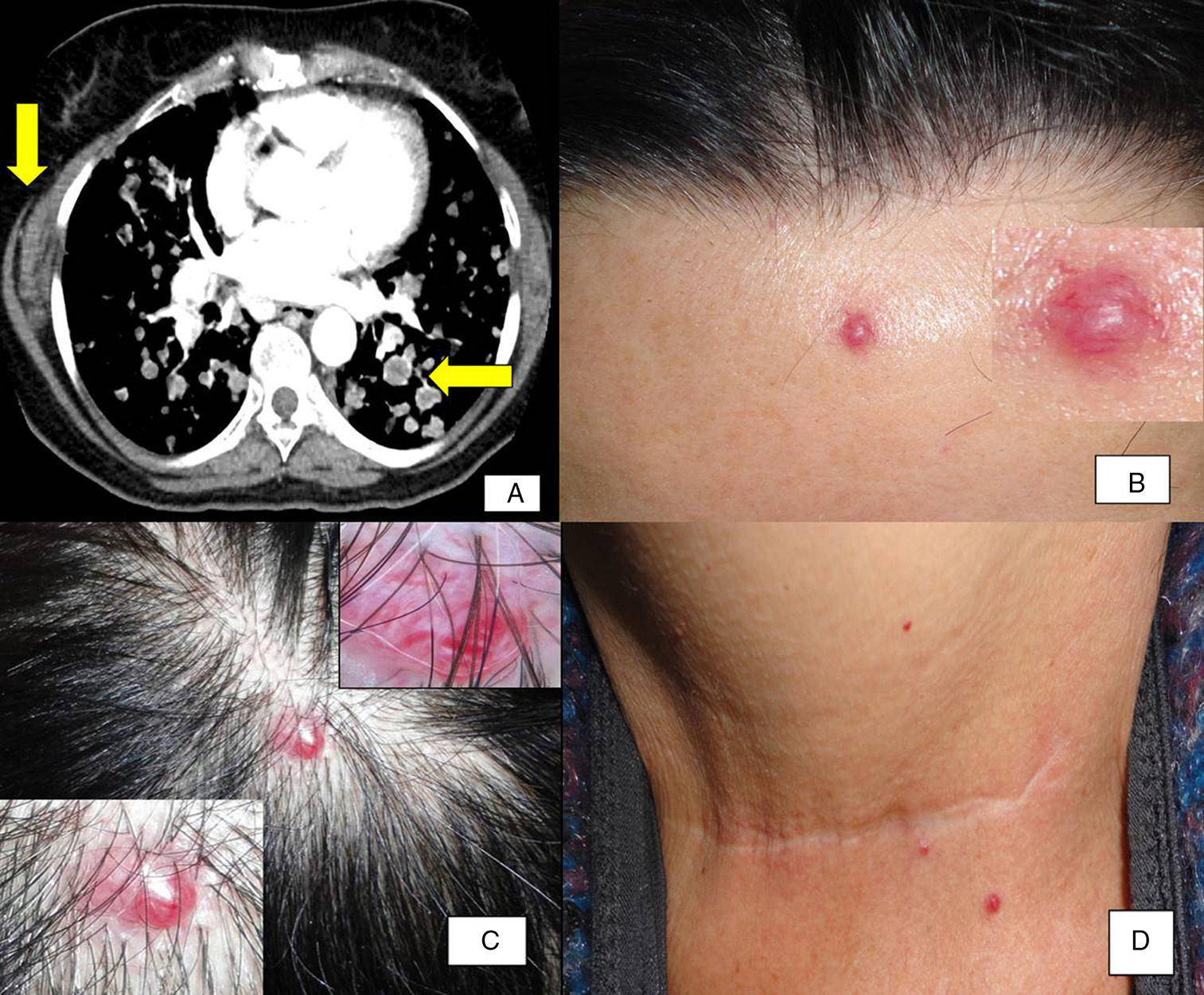
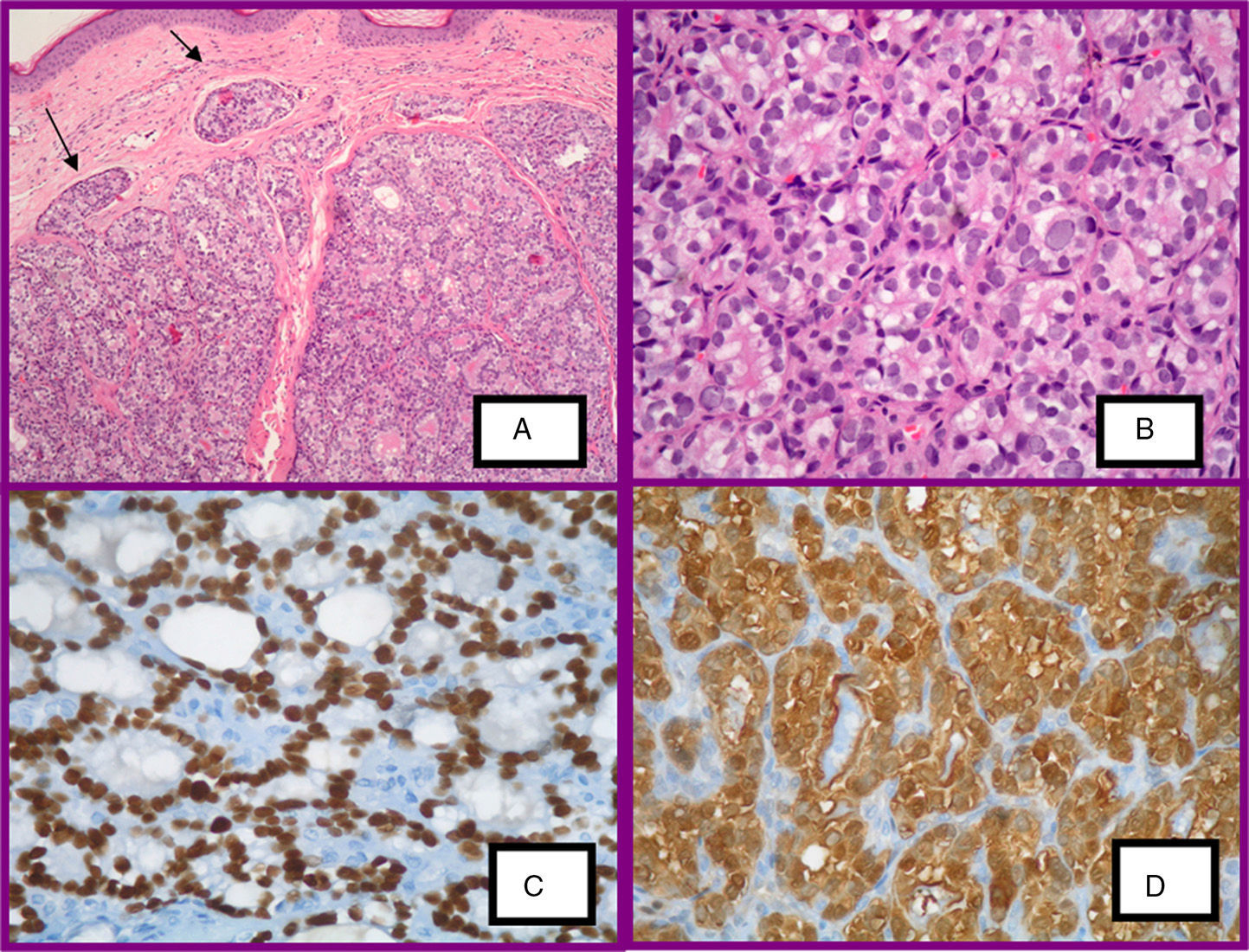
The patient underwent close clinical and imaging follow-up. Two years after surgery, a cervical mass was detected and this was attributed to relapse of papillary thyroid carcinoma. It was decided to excise the lesion and subsequently treat with I131. The patient remained stable, but after 7 months, constitutional symptoms occurred, along with dyspnea and pain in the right side as a result of the presence of multiple bilateral pulmonary nodular metastases, as well as a mediastinal conglomerate lymph nodal mass in both pulmonary hila (Fig. 1a). The physical examination revealed indurated nodular lesions that were mildly itchy with a vascular appearance on the scalp in the frontal region and close to the thyroidectomy scar (Fig. 1b-d). They had appeared 6 months earlier and showed thick vessels with a mottled appearance on dermoscopic examination (Fig. 1c), giving rise to suspicion of metastatic lesions. Biopsy of one of the elements of the scalp revealed a well-delimited intradermal neoplasm, made up of epithelial nodules surrounded by bands of fibrotic tissue and tumoral invasion of superficial skin lymph nodes (Fig. 2a). Neoplastic cells that formed follicular structures had a polygonal form with a clear cytoplasm and pleomorphic nuclei, some of which had a ground-glass appearance (Fig. 2b).
A, Computed tomography of the chest. Pulmonary metastases, mediastinal conglomerate mass of lymph nodes, as well as a mass of soft tissues on the right side. B-D, Red-violaceous lesions in the frontal region, the scalp, and in the proximity of the thyroidectomy scar. Thick, branched vascular structures in dermoscopy of a nodular lesion on the scalp.
A, Histologic lesion of the scalp. Epithelial nodules surrounded by fibrosis and lymphatic invasion of tumor cells (hematoxylin-eosin [H-E], ×40). B, Follicular structures lined by round cells with clear cytoplasm and pleomorphic nuclei (H-E, ×100). C, TTF-1 positive (immunohistochemical staining). D, Galectine-3 positive (immunohistochemical staining).
Immunohistochemical study was positive for TTF-1 (thyroid transcription factor 1) (Fig. 2c) and galectin-3 (Fig. 2d) but negative for thyroglobulin (Tg).
With these findings, cutaneous metastasis of follicular variant of papillary thyroid carcinoma was diagnosed.
The patient received another dose of radioactive iodine, but some months later neurologic symptoms occurred due to bilateral supratentorial and infratentorial brain metastases and osteolytic images were observed in the cranial vault. Given this disease progression, sorafenib was administered in combination with zoledronic acid in the compassionate use setting, but the patient finally died 6 months later.
Cutaneous metastases of thyroid carcinomas are rare (occurring in less than 1% of primary thyroid carcinomas). When they do occur, they present as slow-growing erythematous lesions, purpuric plaques, or soft and mildly itchy erythematous nodules, which may become ulcerated. In 70% of the cases, these lesions are found on the scalp and the rest of the face or neck, due to the extensive vascularization of the dermis at these sites.1–3 The condition affects men and women equally and is most frequently associated with follicular thyroid carcinoma (42%) even though papillary carcinoma is the most frequent primary carcinoma (50%-89%).4 Metastases may present as the first manifestation of an occult papillary carcinoma (worse prognosis) or appear in advanced tumors, as was the case with our patient.5
The presence of vascular structures in dermoscopy of a nodular lesion in a patient with a history of cancer should require differential diagnosis with cutaneous metastases.6 The histological and immunohistochemical characteristics with TTF-1 in the present case, in the clinical context of the patient, suggested diagnosis of metastasis of thyroid carcinoma, although the possibility of a pulmonary origin could not be ruled out given the absence of staining with Tg (characteristically positive). Immunostaining with galectin-3 enabled definitive diagnosis of metastasis of thyroid origin. Galectin plays an important role in cell adhesion and in the interaction between matrix and cells. In addition, it is the primary potential tumor marker for local and distant metastases, particularly in cases of papillary thyroid carcinoma.7
Anatomopathologic diagnosis of metastases of a well-differentiated follicular carcinoma of the thyroid glands is relatively simple given the presence of follicles with colloid material. However, in cases of the follicular variant of papillary thyroid carcinoma, papillary architecture is usually absent and the nuclear characteristics are not always present, and so immunohistochemical techniques are necessary using Tg (sensitivity of close to 100% in follicular cancer, 95% in papillary cancer, and lower in poorly-differentiated carcinomas), TTF-1, RET/PTC, HBME-1, CK19, CD10, and galectin-3.1,7,8 The BRAFV600E mutation has been identified in cutaneous metastases of papillary thyroid carcinoma and its presence is associated with worse prognosis although new chemotherapeutic agents can be used. Mean survival is 19 months after diagnosis of the cutaneous metastases in patients with advanced disease.1
Differential diagnosis should be considered with primary apocrine tumors and other metastatic lesions, with immunohistochemical study with TTF-1, Tg, and galectin-3 being particularly useful.1,5
In conclusion, despite the rarity of cutaneous metastases of thyroid carcinoma, we should be aware of this possibility in the differential diagnosis of cutaneous metastases, given that diagnosis and early treatment may improve prognosis.4
Please cite this article as: Márquez García A, Ferrándiz Pulido L, Ríos-Martín JJ, Camacho Martínez FM. Metástasis cutáneas craneocervicales de un carcinoma papilar de tiroides variedad folicular. Actas Dermosifiliogr. 2016;107:86–88.

![A, Histologic lesion of the scalp. Epithelial nodules surrounded by fibrosis and lymphatic invasion of tumor cells (hematoxylin-eosin [H-E], ×40). B, Follicular structures lined by round cells with clear cytoplasm and pleomorphic nuclei (H-E, ×100). C, TTF-1 positive (immunohistochemical staining). D, Galectine-3 positive (immunohistochemical staining). A, Histologic lesion of the scalp. Epithelial nodules surrounded by fibrosis and lymphatic invasion of tumor cells (hematoxylin-eosin [H-E], ×40). B, Follicular structures lined by round cells with clear cytoplasm and pleomorphic nuclei (H-E, ×100). C, TTF-1 positive (immunohistochemical staining). D, Galectine-3 positive (immunohistochemical staining).](https://static.elsevier.es/multimedia/15782190/0000010700000001/v2_201704190205/S1578219015003261/v2_201704190205/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



