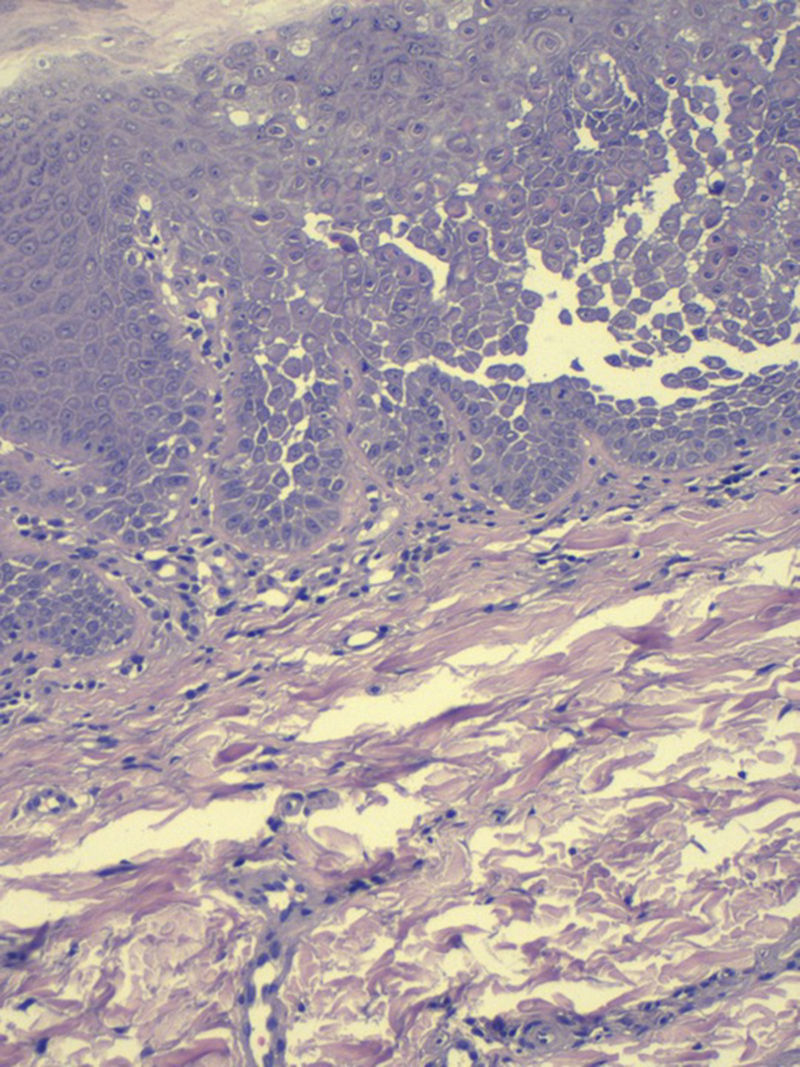
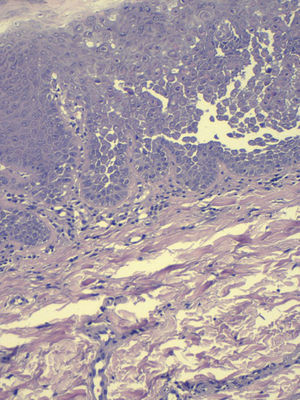
We describe the case of a woman aged 50 years, with a history of systemic hypertension on treatment and benign familial pemphigus (BFP) that had arisen more than 10 years earlier. During those years, she had presented recurrent outbreaks of erosive lesions in the groin, perianal region, and submammary folds (Fig. 1), often with bacterial superinfection. She had received topical therapy with corticosteroids, antibiotics, tacrolimus, and diclofenac, with a partial response. She had also received systemic acitretin at a dose of 25mg/d on several occasions. During a follow-up visit, perianal lesions suggestive of PBF were observed, and asymptomatic shiny whitish papules measuring 2 to 3mm in diameter with a cobblestone appearance on both labia majora (Fig. 2). Biopsy of 1 of these vulvar lesions revealed hyperkeratosis with irregular acanthosis and suprabasal acantholysis with dyskeratosis (Fig. 3); direct immunofluorescence was negative.
Papular acantholytic dyskeratosis (PAD) of the vulva, first described in 1984 by Chorzelski et al.,1 mainly affects young women, typically on the labia majora, although it has also been described on the penis in men, in the anal canal, and in the inguinal folds.2,3 It usually presents as multiple whitish papules that may coalesce to form plaques; solitary papules are rare. Most commonly it is asymptomatic, although intense pruritus can occur. Histopathology reveals acantholysis with varying degrees of dyskeratosis, and direct and indirect immunofluorescence are negative in almost all cases studied.4 Though initially considered an independent entity, its relationship with Darier disease (DD) and with BFP has been under discussion due to the histologic similarity between the diseases.5 The etiology of PAD is unclear. The majority of cases are sporadic, but there have been reports in recent years of cases of DAP due to mutations in genes ATP2A26 and ATP2C1,7–9 which are mutations known in DD and BFP, respectively. Pernet et al.8 reported a familial case of PAD in which the same mutation in ATP2C1 was detected in the mother and daughter, suggesting that PAD is allelic with BFP. Yu et al.9 published the case of a woman with PAD and a family history of BFP; those authors suggested the possibility that a patient with PAD may subsequently develop lesions of BFP and that the 2 diseases belonged to a common spectrum of genetically linked acantholytic dyskeratotic dermatoses. Genetic analysis remains to be performed in our patient, but the coexistence of PAD and BFP in the same patient supports this hypothesis.
We have described a patient with the simultaneous presence of lesions clinically and histologically typical of BFP and PAD; the study of mutations in both lesions remains to be performed. To date, we have found no case reports in the literature describing the coexistence of BFP and PAD in a single patient.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Baliu-Piqué C, Iranzo P. Disqueratosis acantolítica papular de la vulva en una mujer con pénfigo benigno familiar. Actas Dermosifiliogr. 2017;108:78–79.