A 43-year-old woman with a history of obesity and gestational diabetes was referred for evaluation of pruritic lesions that had arisen on her legs 7 years earlier and had shown a fluctuating course. She also described persistent palmar pruritus. She was not on any regular pharmacological therapy. On physical examination, 2 erythematous-brownish hyperkeratotic plaques with a spongiform appearance were observed on the anterior surface of her lower legs. The plaques, which measured 2 to 5cm in diameter, had well-defined borders and were surrounded by a violaceous halo (Fig. 1). In addition, she presented numerous, small, depressed hyperkeratotic papules confined to the palmar creases (Fig. 2). Examination of the oral mucosa revealed a whitish reticulated pattern on the cheek and a cobblestone pattern of whitish papules on the dorsum of the tongue. No lesions were observed on the genital mucosa, nails, or scalp. Histology of a hyperkeratotic plaque on the leg confirmed the clinical suspicion of hypertrophic lichen planus (LP), and biopsy of a small palmar lesion also showed typical histological features of the disease. Laboratory tests, including complete blood count, biochemistry, and serology for HBV, HCV, syphilis, and HIV, were normal or negative.
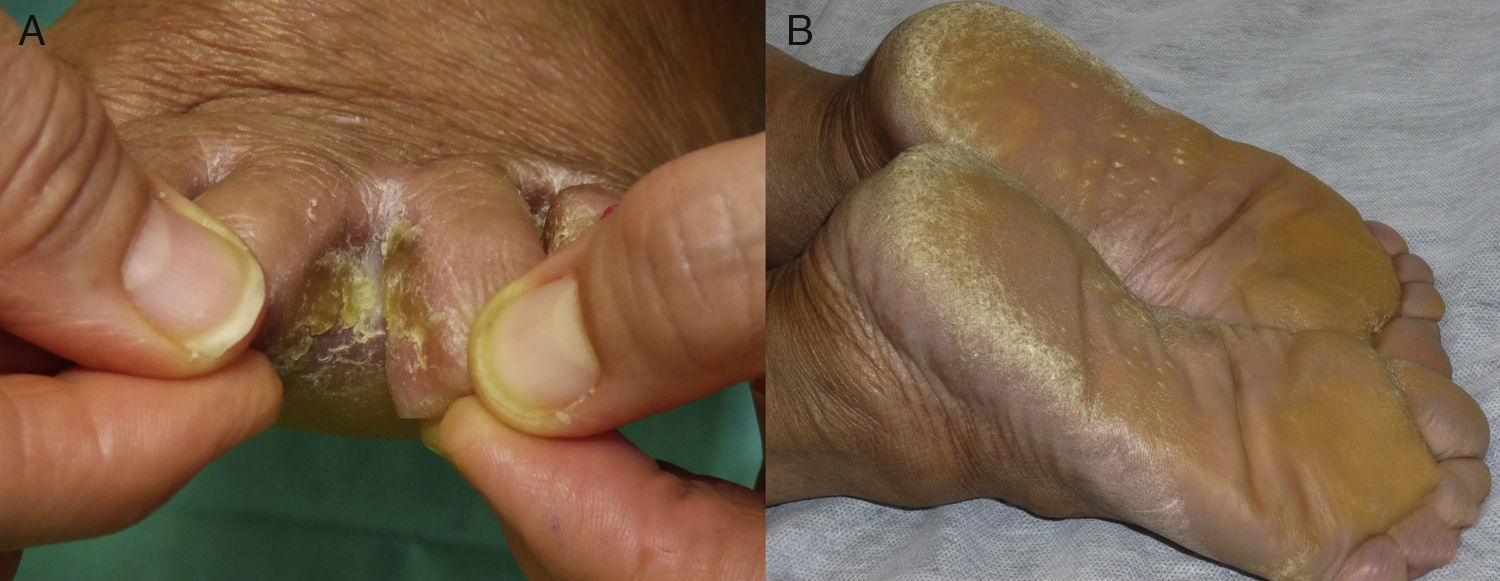
The patient subsequently consulted for the appearance of whitish, macerated and fissured hyperkeratotic plaques in the interdigital folds of the feet (Fig. 3A). Although cultures for fungi were repeatedly negative, oral treatment was started with terbinafine due to the elevated clinical suspicion of dermatophytosis. Given the absence of improvement after a month of treatment, a biopsy was taken, which showed the characteristic findings of LP. Finally, she developed progressive induration of the palms and soles, with severe pain that interfered with her activities of daily living and walking. Examination revealed diffuse palmoplantar keratoderma, most evident in the pressure areas (Fig. 3B), with the presence of confluent pink papules at the border of the keratoderma. Histology again confirmed involvement by LP.
According to the literature, predominantly or exclusively palmoplantar involvement in LP is rare and its clinical presentation differs from classic LP.1 The greater thickness of the corneal layer explains the absence of the characteristic Wickham striae, as the histopathologic correlate—wedge-shaped hypergranulosis—is obscured. In addition, the typical violaceous polygonal papules, only occasionally observed at the borders of the palms and soles, are not present.2 In contrast, a broad spectrum of clinical manifestations have been reported: diffuse keratoderma, punctate keratosis, desquamating erythematous plaques, pseudovesicular and petechial lesions, umbilicated papules, ulcerated lesions and hyperpigmented macules.3–6 The most common finding is a desquamating erythematous or hyperkeratotic pattern. We have found no previous reports of the punctate keratosis pattern confined to the palmar creases, seen in our patient. This case exemplifies how various patterns can present in a single patient. This broad morphological spectrum, with absence of the classic papules of LP, means that clinical diagnosis can be very difficult, particularly if there is only palmoplantar involvement. According to the largest series published, the presence of intensely pruritic, self-limiting, hyperkeratotic or desquamating erythematous plaques with well-defined borders arising on the medial surface of the arch of the foot, with no involvement of the pulp of the toes, is a highly characteristic finding.2 Histology, which reveals the classic features of LP in the palmoplantar tissues, is therefore essential for diagnosis.
Although the majority of the lesions are self-limiting according to Sánchez-Pérez et al.,2 recalcitrant cases have been reported and show a variable response to treatments including corticosteroids, retinoids, psoralen–UV-A baths, methotrexate, ciclosporin, dapsone, and enoxaparin.7,8 Our case provides further evidence of the recalcitrant nature of palmoplantar LP, after the poor response to the administration of multiple cycles of topical and systemic corticosteroid therapy, topical tazarotene, ciclosporin at a dose of 3mg/kg/d (whose efficacy cannot be adequately evaluated due to treatment interruption after a month because of failure to attend follow-up), and methotrexate at a maximum dose of 20mg/wk, which the patient continues to receive. Interestingly, despite hypertrophic LP being considered one of the most refractory variants, the lesions present on our patient's legs responded very well to corticosteroid treatment.
In conclusion, we have described a patient with a rare variant of LP. This case exemplifies the broad clinical spectrum that this disease can present on the palms and soles. The patient developed keratosis punctata-type lesions limited to the palmar creases, a clinical manifestation not previously described, hyperkeratotic interdigital plaques mimicking a superficial fungal infection, and diffuse palmoplantar keratoderma with a marked deterioration of her quality of life. Despite generally being considered a self-limiting disease, the lesions in our case showed a recalcitrant course, with plantar lesions even more refractory to treatment than the hypertrophic LP lesions. The broad morphological variety of palmoplantar lesions, with absence of the classic LP papules, makes diagnosis difficult, and this disease must be included in the differential diagnosis of hyperkeratotic palmoplantar dermatoses. Histology, which shows the typical features of LP, is essential for diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Our thanks to the patient, who gave her written permission for publication of the images.
Please cite this article as: Burillo-Martínez S, Tous-Romero F, Rodríguez-Peralto JL, Postigo-Llorente C. Liquen plano palmoplantar: espectro de manifestaciones clínicas en un paciente. Actas Dermosifiliogr. 2017;108:790–792.