Primary cutaneous lymphomas have a low incidence in the general population. The clinical presentation is very variable, often making the diagnosis unexpected for the dermatologist. Although the diagnosis of these lesions always requires histopathologic confirmation, skin ultrasound is an additional tool that can be helpful for the initial diagnosis of malignancy. We present a case of primary cutaneous CD4+ small/medium T-cell lymphoproliferative disorder (PCSM-TCLD) and its ultrasound findings.
A 55-year-old woman with a past history of hypothyroidism and dyslipidemia came to the emergency department for a pruritic lesion in the right scapular region; the lesion had grown rapidly in the previous 2 months. She reported no fever, asthenia, or weight loss, and she denied any previous lesions or trauma.
Physical examination revealed a solid, tender erythematous-violaceous nodule of 2×1.5cm in the right scapular region (Fig. 1). The nodule was not adherent to deeper planes. A surgical drainage-aspiration procedure performed in the emergency department excluded the presence of fluid collections. There were no palpable lymph nodes or hepatosplenomegaly.
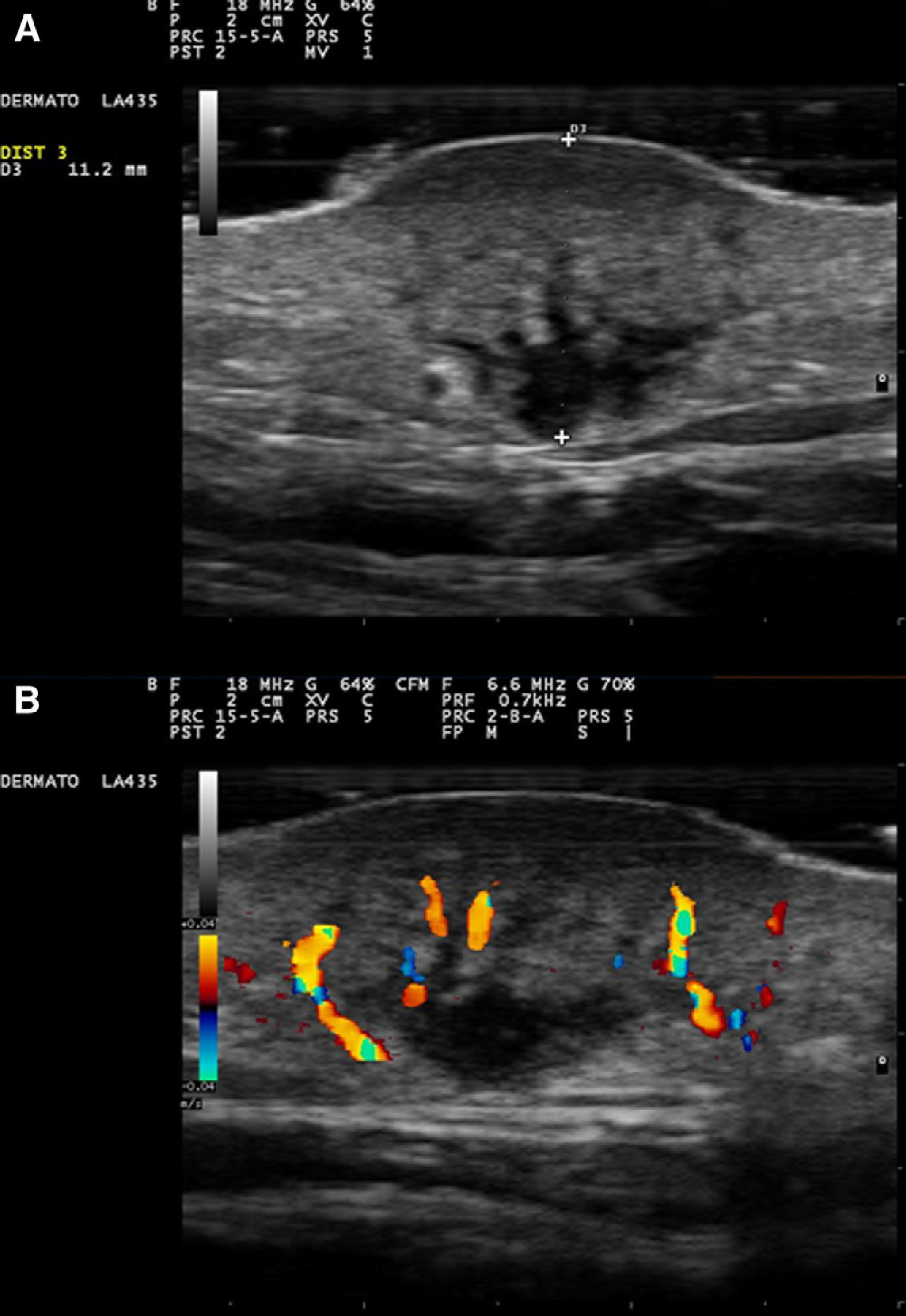
Skin ultrasound of the lesion was performed in dermatology outpatient clinic. Examination in B mode (18MHz probe, MyLab 25 Gold, Esaote, Italy) revealed a dermal nodule of 20×15×11mm, with deep extension into the subcutaneous cellular tissue. The nodule had a heterogeneous content, was not encapsulated, and had poorly defined borders (Fig. 2A). The superficial or dermal plane of the lesion and its deeper or hypodermal plane were noticeably more hypoechoic than the intermediate plane that separated them, and contained hypoechoic tubular tracts. Color Doppler examination revealed the presence of extensive neovascularization, with large vessels within the tumor (Fig. 2B).
A, B-mode ultrasound, 18MHz. Dermal nodule with extension into the subcutaneous cellular tissue, with a heterogeneous content and poorly defined borders. Lower echogenicity of the superficial and deep planes compared with the intermediate plane. B, Color Doppler ultrasound showing large-caliber vessels within the tumor.
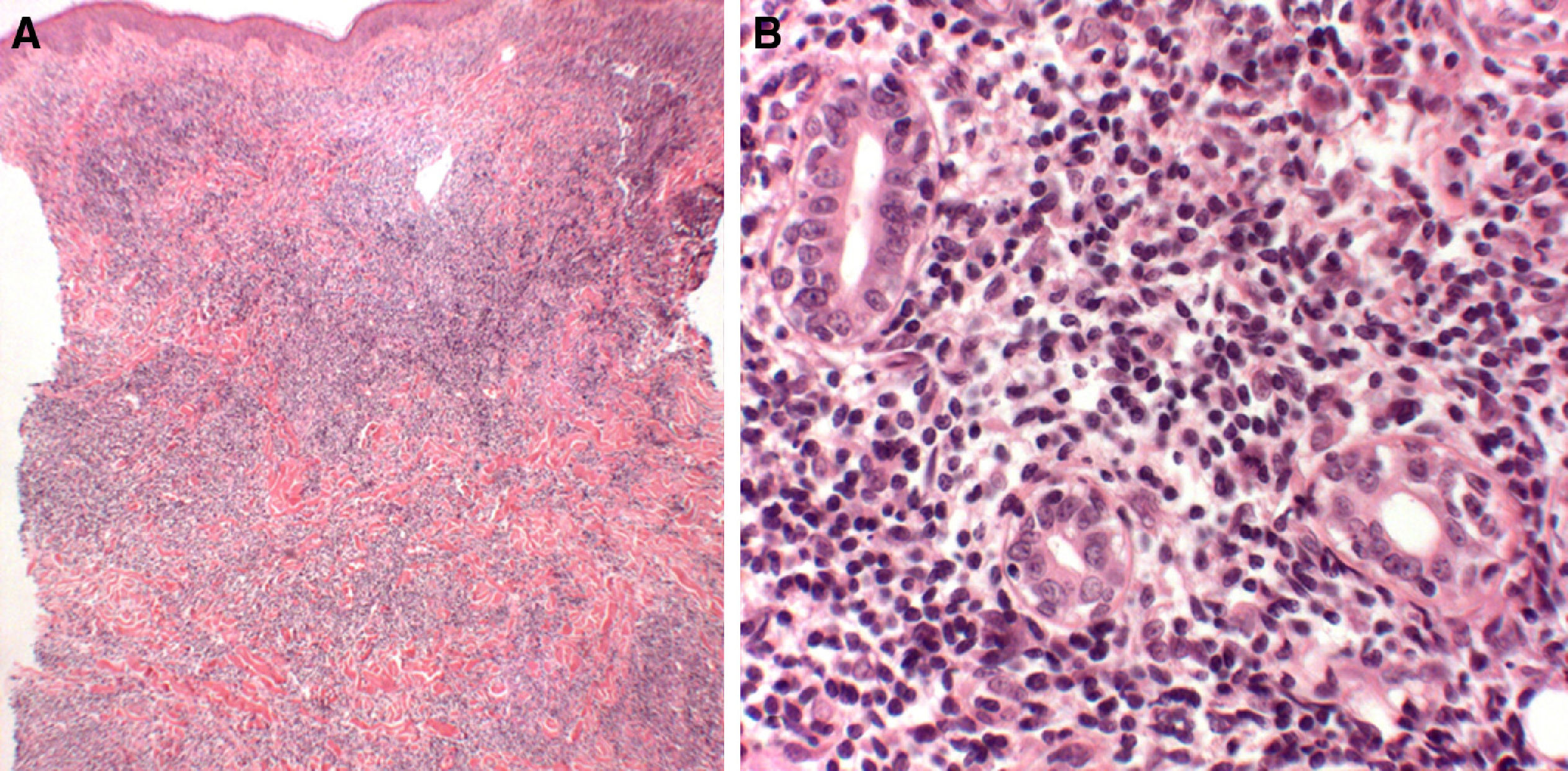
These ultrasound findings supported the clinical suspicion of malignancy, and a 4mm punch biopsy was therefore performed for histopathology study. Analysis of the sample showed a dense perivascular and periadnexal interstitial lymphocytic infiltrate that extended into the hypodermis and did not affect the epidermis; the infiltrate was formed of small/medium-sized lymphocytes with mild-to-moderate pleomorphism (Fig. 3, A and B). Immunohistochemistry was positive for CD2, CD3, CD4, CD5, and BF1 and negative for CD8, CD30, granzyme, perforin, CD56, CD57, CD20, and CD79. Molecular analysis detected a monoclonal rearrangement of the T-cell receptor gene that, together with the previous findings, was consistent with a diagnosis of PCSM-TCLD.
Perivascular and periadnexal interstitial lymphocytic infiltrate that extends into the hypodermis and respects the epidermis. The infiltrate is formed of small/medium-sized lymphocytes with mild-to-moderate pleomorphism. A, Hematoxylin and eosin, original magnification x10. B, Hematoxylin and eosin, original magnification x40.
No significant alterations were detected in the metastatic work-up with cervico-thoraco-abdominopelvic computed tomography and a blood test including lymphocyte subpopulations, lactate dehydrogenase, and β2-microglobulin. The patient was offered radiotherapy, which achieved a good response, and there has been no recurrence of the disease.
Primary cutaneous CD4+ small/medium T-cell lymphoma was a provisional entity in the 2008 World Health Organization classification of hematologic tumors.1 Because of its uncertain malignant potential, the term lymphoproliferative disorder has been recommended instead of lymphoma in the more recent 2016 classification.2 The disease typically presents clinically as an erythematous-violaceous plaque or nodule of firm consistency, usually localized on the trunk or face. It is characterized histologically by a diffuse or nodular dermal infiltrate of atypical CD4+ small- and medium-sized lymphocytes, as in the case described. Although the prognosis of these lesions is usually excellent,3,4 aggressive forms have very rarely been described.5
The widespread incorporation of skin ultrasound into dermatology outpatient clinics has led to the recent development of numerous applications, from the study of inflammatory diseases to definition of the ultrasound characteristics of a number of malignant tumors.6 However, little has been published on the ultrasound findings in cutaneous lymphoma.7
Taking into account the clinical and histopathologic variability of PCSM-TCLD,5 certain diversity is to be expected in the ultrasound findings. Using studies performed on soft-tissue lymphomas as reference,8–11 it can be seen that a diffuse infiltration of atypical lymphocytes usually produces an ultrasound image with hypoechoic and heterogeneous areas with poorly defined borders, as was observed in our patient. The presence of an intense neoangiogenesis on color Doppler appears to be a characteristic finding in soft-tissue lymphomas, and is typically more prominent than in other malignant tumors.9,10
The sonographic differentiation between skin metastases and other tumors can be complicated, but carries important prognostic implications for the patient. Such lesions often present clinical and ultrasound features similar to those described, and this must be taken into account.
In summary, we have presented a case of PCSM-TCLD and its ultrasound findings. These findings helped to orient the initial suspicion of malignancy in a clinically nonspecific lesion. We hope that progressive advances in cutaneous ultrasonography will enable us to better define the diagnosis of this type of tumors.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rodríguez-Lomba E, Molina-López I, Pulido-Pérez A, Ciudad-Blanco C. Ecografía del síndrome linfoproliferativo primario cutáneo T CD4+ de célula pequeña/mediana. Actas Dermosifiliogr. 2017;108:792–794.