Oncologic surgery of the eyelid and orbital region is a challenge in dermatologic surgery. This region presents difficulties and possible complications that do not exist at other sites, including ectropion, epiphora, corneal exposure, keratitis, conjunctivitis, and lagophthalmos. Adequate oncologic surgery associated with the best possible functional and cosmetic result requires extensive knowledge of the anatomy, innervation, and blood supply of the eyelid and anatomy of the lacrimal apparatus. We present examples of reconstructive surgical techniques that can be used after the excision of tumors of the upper or lower eyelid, with descriptions of the different flaps and grafts employed in our department in recent years. We also review the surgical techniques according to the site and size of the lesions.
La cirugía oncológica del párpado y de la región orbitaria supone un reto en cirugía dermatológica, ya que en esta región se encuentran dificultades y posibles complicaciones que no hay en otras localizaciones, como podrían ser el ectropión, la epífora, exposición corneal, queratitis, conjuntivitis o lagoftalmos, entre otros.
Para conseguir una correcta cirugía oncológica, unida a un resultado lo más funcional y cosmético posible, es necesario el correcto conocimiento de las estructuras anatómicas de los párpados, así como su vascularización, inervación y anatomía del aparato lacrimal.
Presentamos varios ejemplos de técnicas quirúrgicas reconstructivas tras exéresis tumorales quirúrgicas, tanto en el párpado superior como en el inferior, con diversos colgajos o injertos, que se han realizado en nuestro servicio en los últimos años, y revisamos las posibles técnicas quirúrgicas según el tamaño y la localización de las lesiones.
The eyelid and the orbital region are anatomically highly complex topographic areas, and this means that they are probably among the most difficult areas for reconstruction in dermatologic surgery. This region also carries additional risks that are not encountered in other anatomic areas. The intricacies of palpebral surgery are a challenge for dermatologists and can make it difficult to perfect the techniques required in this surgical field.
The neoplastic disease that most frequently affects the eyelids is basal cell carcinoma,1 which typically arises on the lower eyelid.2–4 Other tumors can also be found in this area, including, though not limited to, squamous cell carcinoma, sebaceous carcinoma, melanoma, Merkel cell carcinoma, angiosarcoma, various types of lymphoma, microcystic adnexal carcinoma, and malignant fibrous histiocytoma.4 Furthermore, the possibility of tumor spread to deeper structures along the embryonic fusion lines of the medial canthus must also be taken into account.5 The principal objective of oncologic surgery to this area consists, as always, of complete excision of the tumor lesion, whether by conventional excisional surgery or by microscope-assisted surgery. Subsequently, during reconstruction, the aim must be to preserve the maximum possible degree of palpebral function and, finally, to achieve the best possible cosmetic result. Care must be taken to avoid complications such as ectropion, corneal exposure, loss of rigidity of the palpebral margin, lagophthalmos, epiphora, or loss of tension in the upper eyelid, which can cause mechanical ptosis.6
To perform optimal palpebral surgery, it is essential to have a full knowledge of palpebral anatomy, and of the different possible anesthetic techniques. Appropriate surgical instruments should be used and basic reconstruction techniques must be understood.
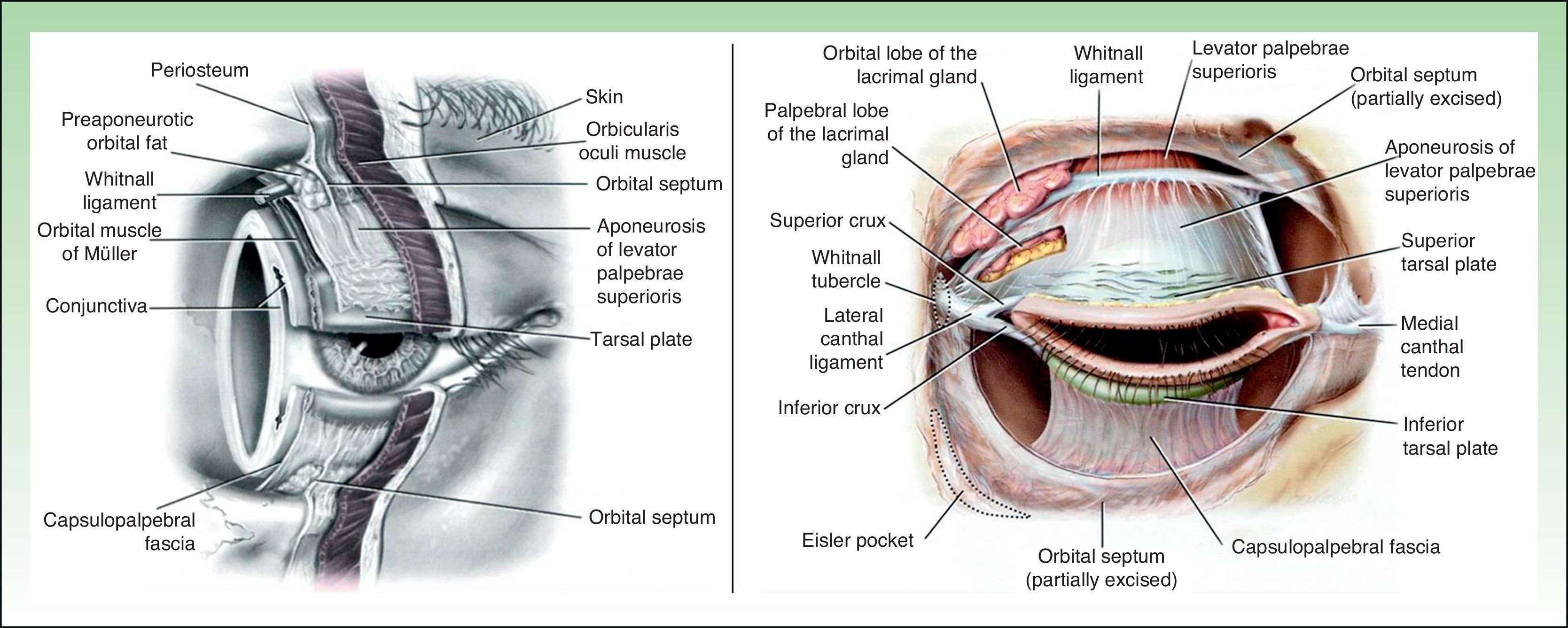
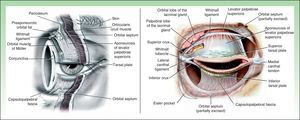
Palpebral AnatomyThe eyelids are complex anatomic structures that act as a shield, protecting the globe and creating and maintaining the lacrimal film.6,7 Each eyelid measures approximately 30mm in width and 8 to 10mm in height.5 The palpebral fissure, which is the space between the open eyelids, varies from 7 to 10mm in men and 8 to 12mm in women.5 The skin of the eyelids is very fine, with a thickness that varies between 700 and 800μm.5 There is virtually no dermis, and the subcutaneous cellular tissue is very loose and is easily distended, which means that hematomas and edema are easy to cause even in minor interventions. In each eyelid, the orbicularis oculi muscle is found deep to the subcutaneous cellular tissue. This muscle is a protractor muscle, meaning that its main function is to close the eyelids; this facilitates lacrimal drainage. Deep to the orbicularis oculi muscle are the superior and inferior tarsal plates, which are 2 fibrocartilaginous plates with an approximate thickness of 0.8 to 1mm. These plates are attached respectively to the superior and inferior orbital margins by the orbital septum, a fibrous layer that separates the eyelids from the contents of the orbit. The medial and lateral extremes of the tarsal plates are attached to the orbital rim by the medial and lateral canthal ligaments. The palpebral conjunctiva is tightly adherent to the tarsal plates and is continuous with the marginal conjunctiva, and subsequently, on reaching the fornix, is reflected over the globe, where it continues to the margin of the cornea, forming the bulbar conjunctiva (Fig. 1).
In some people a fine gray line can be distinguished at the free border of the eyelid. This is the line of separation between the anterior and posterior lamellae of the eyelid. The anterior lamella is formed of skin and the orbicularis oculi muscle, and the posterior lamella by the tarsal plate, the retractor muscles, and the conjunctiva. The eyelashes are found in 2 or 3 irregular rows in front of the gray line, with 100 to 150 eyelashes in the upper eyelid and approximately half that number in the lower lid. The openings of the Meibomian glands are present behind the gray line.
The limits of the upper eyelid are the inferior border of the eyebrow superiorly and the free palpebral margin inferiorly. The superior palpebral fold divides the eyelid into pretarsal (inferior) and preseptal (superior) portions. The limits of the lower eyelid are the palpebral margin superiorly and the malar sulcus and nasojugal folds inferiorly. The inferior palpebral fold low is less apparent in adults; it is more clearly visible in children.
The medial and lateral canthi are the sites of union of the upper and lower eyelids at their medial and lateral ends, respectively. The lacrimal caruncle is found at the medial canthus, together with the double lacrimal drainage via the superior and inferior canaliculi.
MusclesIn addition to the orbicularis oculi muscle, the protractor muscles of the eyelids include the corrugator superciliaris muscle (situated deep to orbicularis oculi and occipitofrontalis muscles), which draws the eyebrows down and together, and procerus, whose contraction causes horizontal wrinkles to appear on the bridge of the nose.5
The retractor muscles open the eyelids. These muscles in the upper eyelid are levator palpebrae superioris and the orbital muscle of Müller. The retractor muscles of the lower eyelid are the inferior tarsal muscle and the capsulopalpebral fascia, which arises from the antero-inferior surface of the inferior rectus muscle.5
Arterial and Venous Blood SupplyThe main arterial blood supply of the eyelids is via the superior and inferior palpebrales arteries, lateral branches of the ophthalmic artery that reach the eyelids above and below the medial canthal ligament, respectively. These arteries run laterally across the eyelids, between the tarsal plate and orbicularis oculi muscle, and anastomose at the lateral canthus. This main blood supply is supplemented by another arterial network of smaller caliber vessels; this network arises from the supra- and infraorbital and lacrimal arteries. Venous drainage is via a double pre- and retrotarsal network that drains mainly into the superficial temporal, facial, and angular veins.
InnervationMotor innervation is derived from the facial nerve (VII cranial nerve) and from the oculomotor nerve (III cranial nerve). Sensory innervation runs via the first 2 branches of the trigeminal nerve (V cranial nerve).
Lacrimal ApparatusThe lacrimal apparatus contains both a secretory system and a collector system. The secretory system has 2 components: basic and reflex. The reflex system comprises the main lacrimal gland, which is found in the anterolateral area of the roof of the orbit and opens onto the conjunctiva 4 to 5mm above the lateral end of the superior tarsus, and the accessory palpebral glands. The collector system comprises the lacrimal papillae and the superior and inferior canaliculi; thus there is a double drainage route for the tear fluid. These canaliculi drain into the lacrimal sac, which drains via the nasolacrimal duct into the nasal cavity.5
Anesthesia in Palpebral SurgeryThere are various techniques available to anesthetize the skin in palpebral surgery. The injection of local anesthetic is useful for small lesions that do not require mobilization of a large volume of tissue. The local anesthesia is usually infiltrated into the subcutaneous cellular tissue, although injection deep to the orbicularis oculi muscle can sometimes be necessary. Peripheral nerve blocks provide a large area of anesthesia using small volumes of anesthetic. The most widely used blocks in palpebral surgery are the supraorbital, supratrochlear, and infraorbital blocks (Fig. 2).
Regional nerve blocks: A, Supraorbital nerve; B, Supratrochlear and infratrochlear nerves, nasociliary nerve, and external nasal branch of the anterior ethmoidal nerve; C, Infraorbital nerve: D, Zygomatico-facial, zygomatico-temporal, and lacrimal nerves. Figure courtesy of Dr. F. J. Vázquez Doval.5
In the supraorbital nerve block, approximately 0.5-1cc of the anesthetic agent is injected at the level of the supraorbital notch in the superior orbital margin.5 The needle must penetrate parallel to the roof of the orbit and perforate the orbital septum. This block anesthetizes the middle two thirds of the upper eyelid and the corresponding area of the forehead.
A block of the infra- and supratrochlear nerves and of the nasociliary nerve anesthetizes the medial third of the upper eyelid, the caruncle, medial conjunctiva, medial canthus, and superomedial part of the nose.5 To perform this block, we palpate the notch in the medial third of the superior orbital margin, above the medial canthus, and the needle must penetrate 1-2cm from the orbital margin, along the medial wall of the orbit.
In the infraorbital or superior maxillary nerve block, the site of injection of the anesthetic agent is 1cm below the inferior orbital margin, vertically in line with the union of the medial third and lateral two thirds of that margin.5 This block anesthetizes the lateral wall of the nose, the cheek, the upper lip and the lower eyelid.
In addition to local anesthesia and peripheral nerve blocks, topical anesthesia can also be used in palpebral surgery. This is applied as anesthetic eyedrops, such as 4% lidocaine. Despite the short duration of action, this type of anesthesia can be useful prior to the injection of an anesthetic agent into the conjunctiva, which may be used in cases of full-thickness resections.
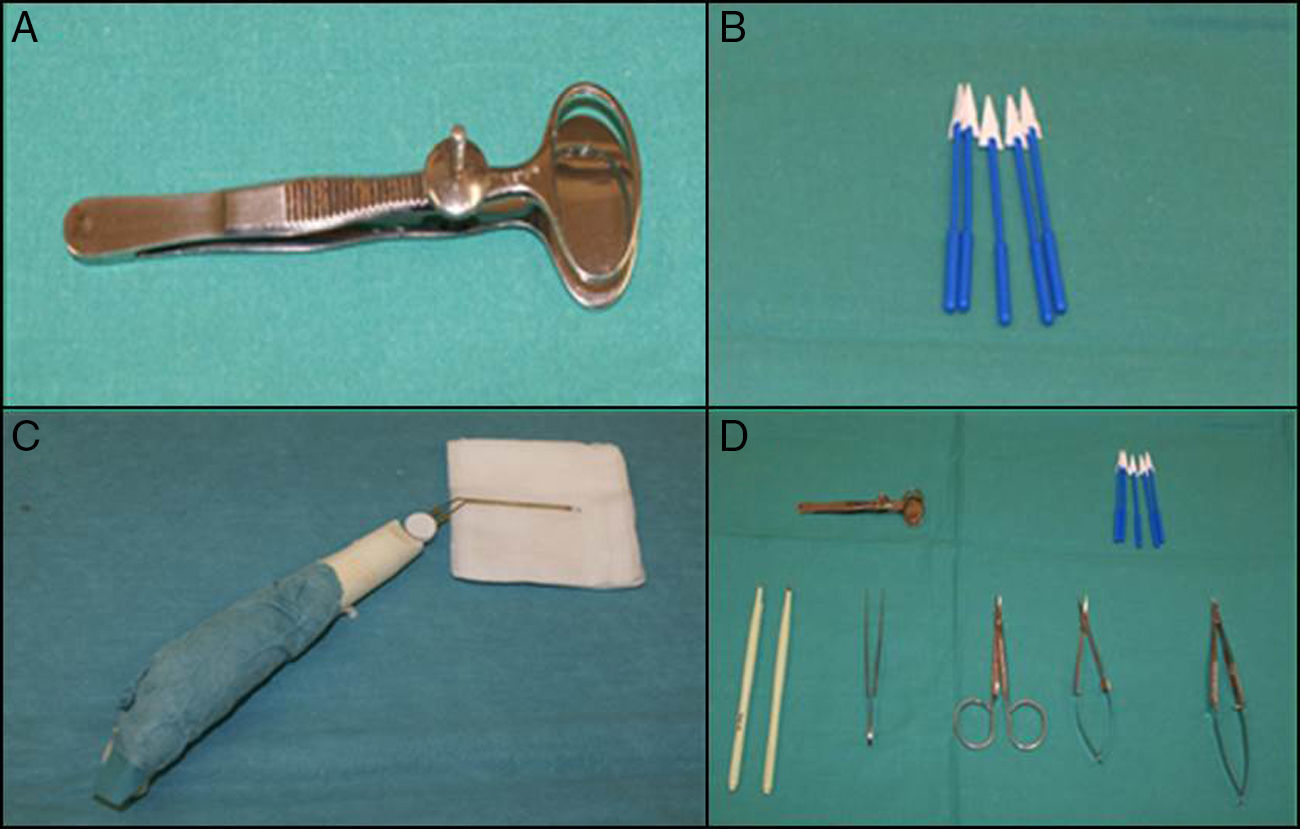
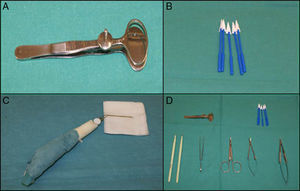
Surgical Instruments in Palpebral SurgeryApart from the usual instruments employed in dermatologic surgery, there is a particularly useful and practical instrument that facilitates more precise palpebral surgery, the chalazion forceps (Fig. 3A). These forceps are very useful in full-thickness resections as they protect the globe and also perform hemostasis.8 In small surgical fields, Weck-Cel sponges (Fig. 3B) can be much more precise than swabs. Colorado microdissection needles have a very fine tip that does not produce excessive thermal damage; they are used in unipolar mode both for dissection and for the electrocoagulation of small vessels. Ophthalmologic cautery (Fig. 3C) also produces little thermal damage and can be useful in patients with pacemakers. Other examples of fundamental surgical instruments for oculoplastic surgery are the Wescott scissors, the Castroviejo needle holder, and the no. 15 keratome (Fig. 3D).
Perioperative Care in Palpebral SurgeryIn palpebral surgery, there are certain aspects of intraoperative care that differ from the care actions performed in other areas of the skin. These include the use of a corneal shield, which protects the cornea against possible trauma, irrigation with saline solution to prevent the formation of keratitis or ulcers, the use of corticosteroid and antibiotic eyedrops, and leaving long suture ends, which can subsequently be fixed to the skin of the eyelid or cheek by adhesive strips to avoid the possible continuous abrasion of short suture ends against the cornea, with the consequent annoyance for the patient and the risk of corneal ulcers. In the postoperative period, the local application of ice can help to reduce the edema and inflammation frequently provoked by palpebral surgery. Finally, tarsorrhaphy is considered to be the most effective method of ensuring immobilization after surgery.
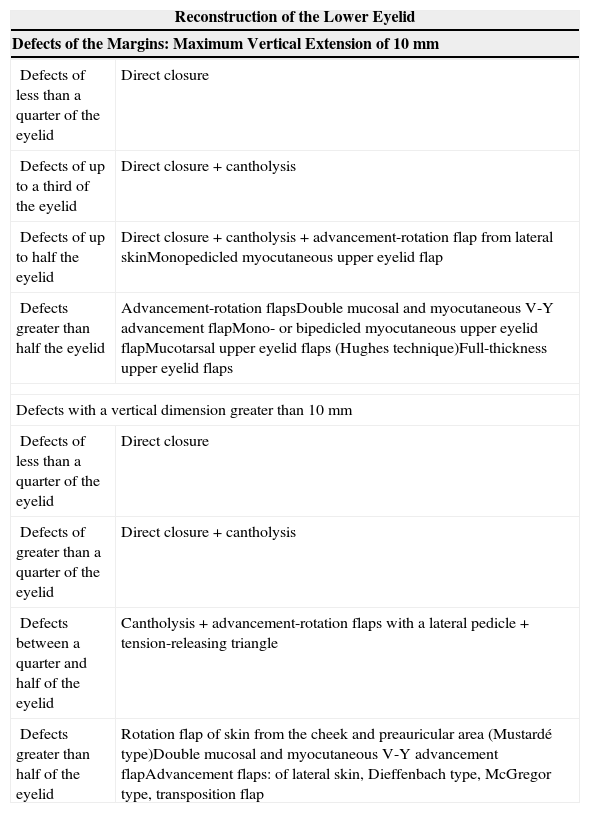
Basic Reconstruction Techniques1,2,5–7,9–18Many techniques can be used both for upper and for lower eyelid reconstruction; the choice depends to a great extent on the size of the defect created and on its site,2,7,9 though the histology of the lesion and other factors, such as the age of the patient, must be taken into account (Table 1). Whenever possible, the eyelashes should be preserved, as they are an excellent point of reference during surgery.
Basic Palpebral Reconstruction Techniques.
| Reconstruction of the Lower Eyelid | |
|---|---|
| Defects of the Margins: Maximum Vertical Extension of 10mm | |
| Defects of less than a quarter of the eyelid | Direct closure |
| Defects of up to a third of the eyelid | Direct closure+ cantholysis |
| Defects of up to half the eyelid | Direct closure+ cantholysis+ advancement-rotation flap from lateral skinMonopedicled myocutaneous upper eyelid flap |
| Defects greater than half the eyelid | Advancement-rotation flapsDouble mucosal and myocutaneous V-Y advancement flapMono- or bipedicled myocutaneous upper eyelid flapMucotarsal upper eyelid flaps (Hughes technique)Full-thickness upper eyelid flaps |
| Defects with a vertical dimension greater than 10mm | |
| Defects of less than a quarter of the eyelid | Direct closure |
| Defects of greater than a quarter of the eyelid | Direct closure+ cantholysis |
| Defects between a quarter and half of the eyelid | Cantholysis+ advancement-rotation flaps with a lateral pedicle+ tension-releasing triangle |
| Defects greater than half of the eyelid | Rotation flap of skin from the cheek and preauricular area (Mustardé type)Double mucosal and myocutaneous V-Y advancement flapAdvancement flaps: of lateral skin, Dieffenbach type, McGregor type, transposition flap |
| Reconstruction of the Upper Eyelid | |
|---|---|
| Defects at the Eyelid Margins | |
| Defects of less than a quarter of the eyelid | Direct closure |
| Defects up to a third of the eyelid | Direct closure+ cantholysis |
| Defects between a quarter and half of the eyelid | Direct closure+ cantholysis+ advancement-rotation flaps from lateral skinMonopedicled myocutaneous flap from the lower eyelid |
| Defects greater than half of the eyelid | Bipedicled flaps of preseptal skin from the upper eyelidSliding flaps of preseptal skin from the upper eyelidFull-thickness lower eyelid flaps (Cutler-Bread type) |
| Vertically Orientated Defects | |
| Defects up to half of the eyelid | Same reconstruction plan as for the lower eyelid |
| Defects greater than half of the eyelid | Full-thickness rotation flaps from the lower eyelid, with direct closure of the lower eyelid defectFull-thickness rotation flaps from the lower eyelid, with closure of the lower eyelid defect using lateral advancement-rotation flaps |
| Subtotal or full-thickness defects of the upper eyelid | Full-thickness rotation flaps from the lower eyelid with reconstruction of the lower eyelid using a rotation flap of skin from the cheek (Mustardé type) |
Horizontal elliptical incisions are recommended for small skin lesions of the upper or lower eyelid, unless, for example, the vertical height of the residual lower eyelid would be too small, with a risk of ectropion, in which case the incision should be vertical.
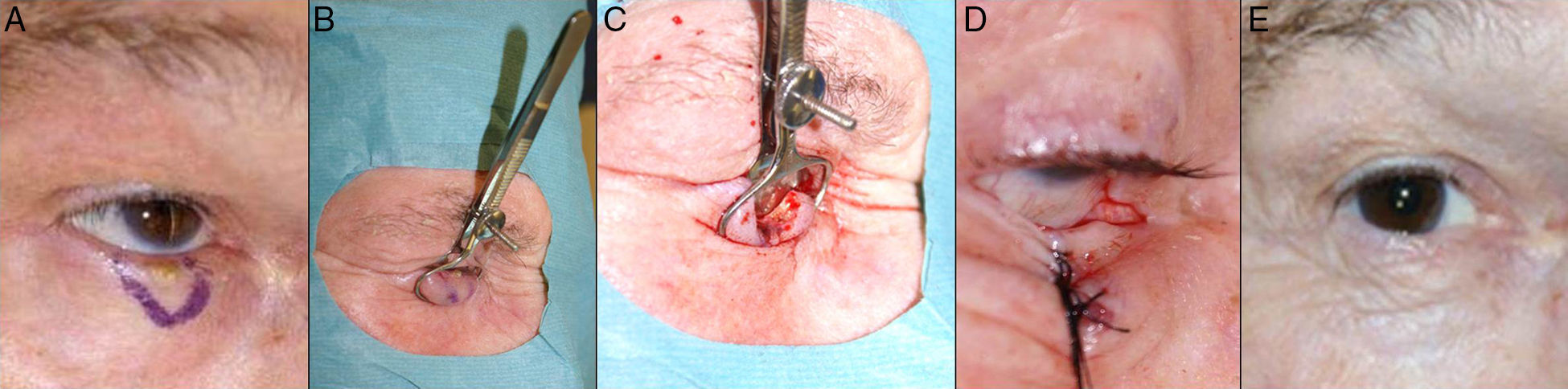
Defects Affecting Less Than a Quarter of the Total Area of the Lower EyelidWhen full-thickness excisions are performed leaving defects with a vertical dimension greater than 10mm, the recommended method of reconstruction depends on the defect created. Applying the basic principles of eyelid surgery, defects of less than a quarter of the total area of the lower eyelid can be closed by direct suture9,12(Fig. 4).
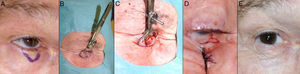
A, V-shaped en bloc full-thickness resection of an incipient basal cell carcinoma leaving a defect of less than a quarter of the lower eyelid. B and C, The chalazion forceps aid hemostasis and facilitate the full-thickness resection. D, Suture of the tarsal plate and mucosa with 6/0 Vicryl and 5/0 silk. Long ends of the silk suture to avoid abrasion against the cornea. E, Outcome 1.5 months after the operation.
With defects affecting more than a quarter of the area of the lower eyelid, canthotomy and cantholysis are performed to reduce the tension and facilitate closure.9,12 In a lateral canthotomy, a horizontal incision is made from the lateral canthus to the lateral orbital margin, and the orbicularis oculi muscle is then sectioned to reveal the periostium.5 Cantholysis consists of sectioning the canthal tendon, which can be identified by pulling the lateral part of the eyelid upwards and outwards, with the tendon incision being made in the area of resistance to this movement; this will release the lower eyelid from the orbital ring.5 Several techniques have been described, including transconjunctival lateral cantholysis without associated lateral canthotomy, to permit the closure of defects of the eyelid that are too large for direct closure.19,20
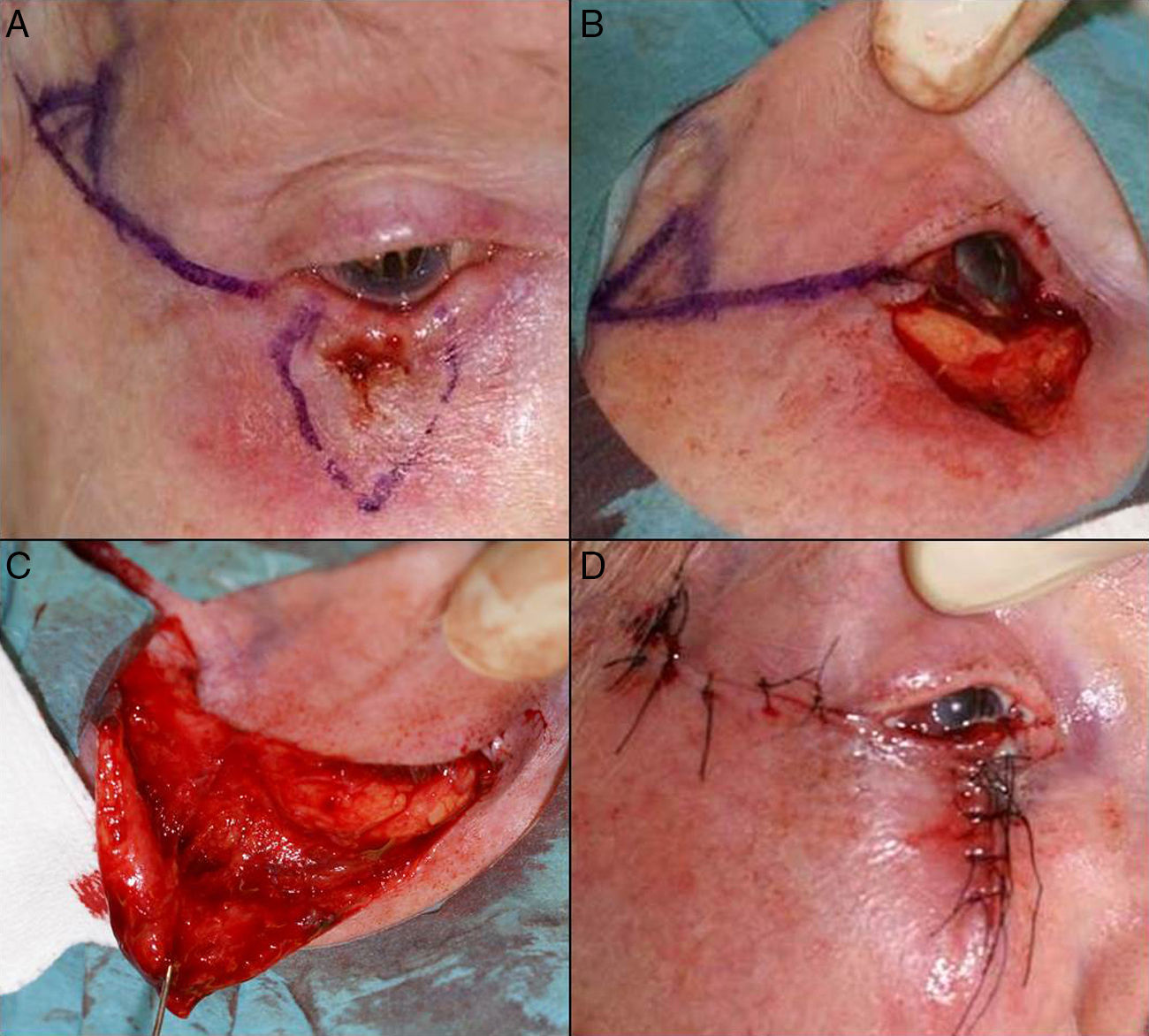
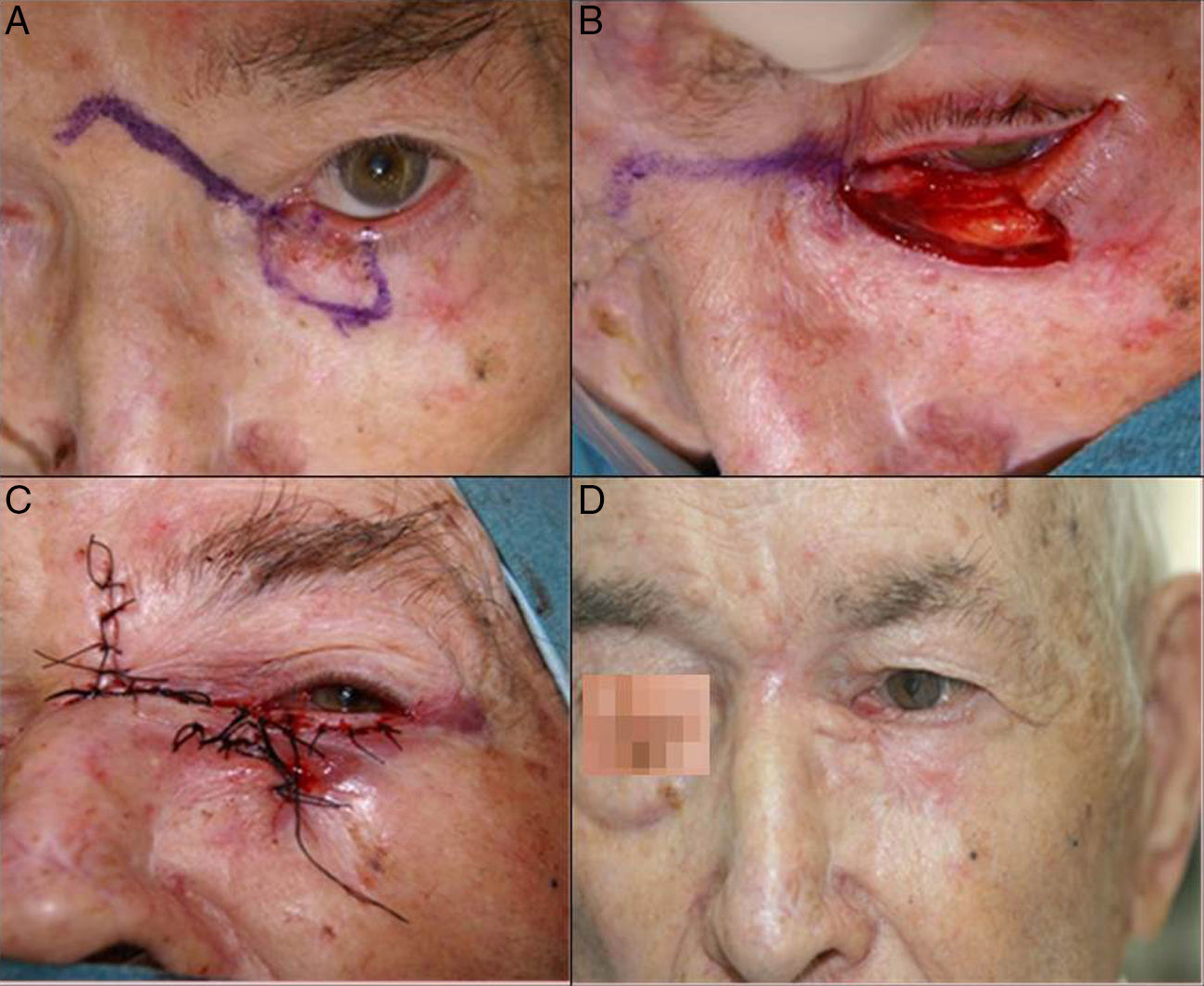
Defects Affecting More Than Half of the Total Area of the Lower EyelidIn defects affecting more than half of the lower eyelid, cantholysis associated with advancement-rotation flaps is recommended9 (Fig. 5).
A, Squamous cell carcinoma that produced retraction, provoking ectropion. B, V-shaped en bloc full-thickness resection leaving a defect greater than half of the lower eyelid. C, Cantholysis and an advancement flap. D, Suture with 4/0 and 5/0 silk, with long suture ends on the lower eyelid to avoid abrasion against the cornea. Eyelid edema and hematoma and hyposphagma (subconjunctival hemorrhage).
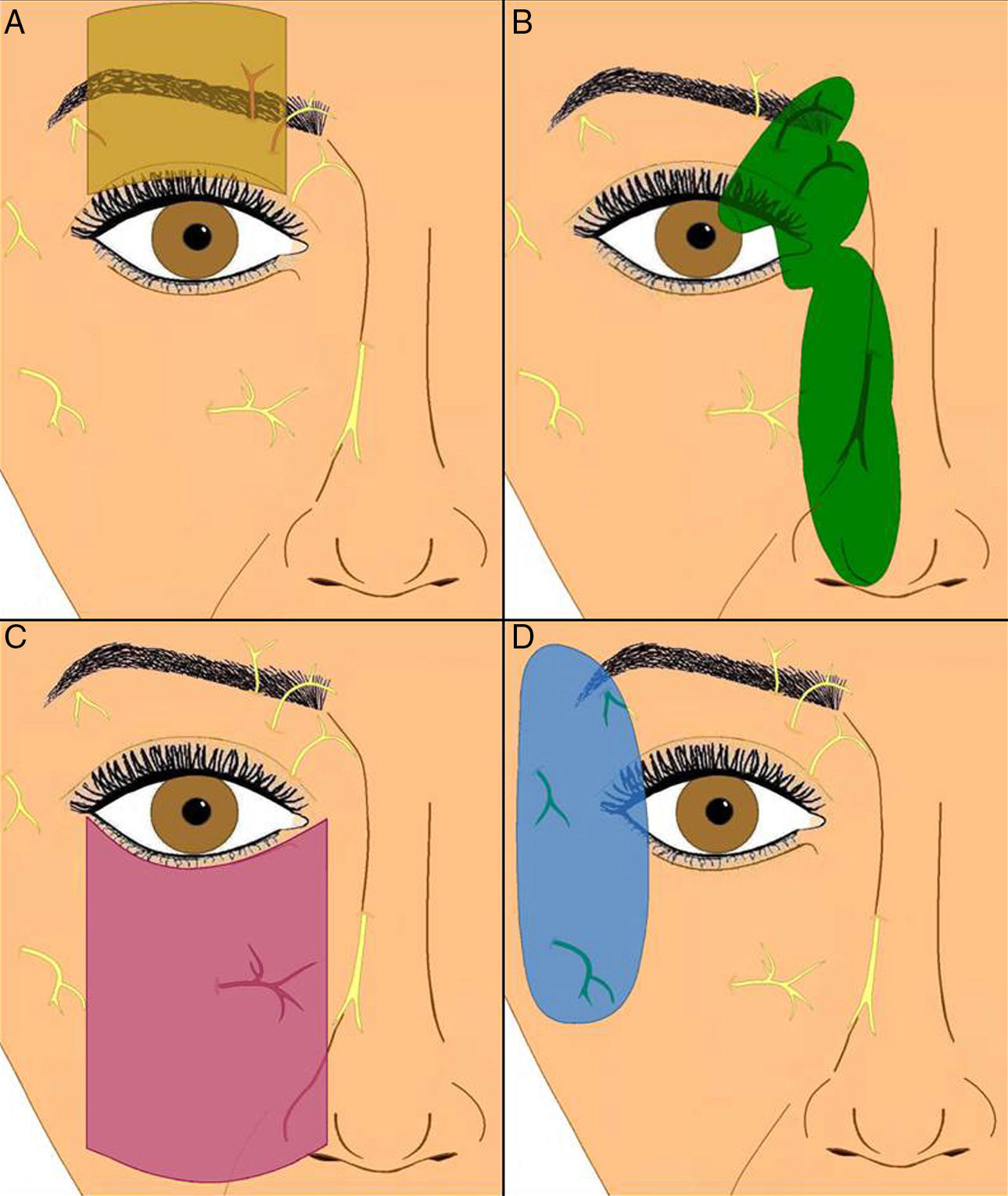
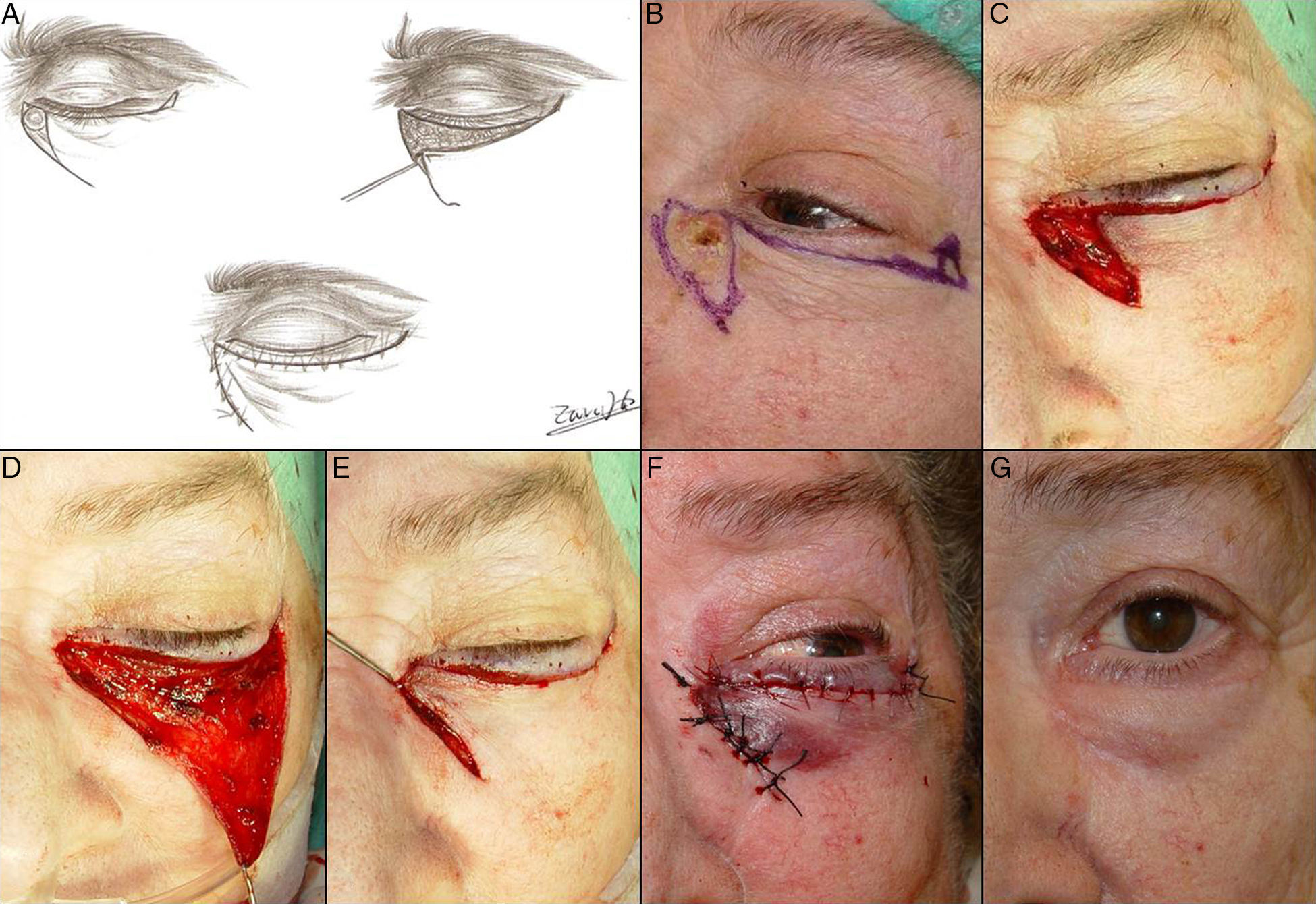
When performing skin flaps or myocutaneous flaps of the skin and orbicularis oculi muscle, it must not be forgotten that the tension forces created must always be horizontal, never vertical, to avoid ectropion, and anchoring sutures must be used to reduce tension at the surface. Advancement flaps of the lower eyelid allow defects of the skin and orbicularis oculi muscle to be reconstructed (Figs. 6 and 7). When the lesion is in the lateral or medial area of the lower eyelid, a single advancement flap is usually sufficient. However, when the lesion is in the central area of the lower eyelid it can occasionally be necessary to perform a double advancement flap, with one flap from each side. When these lower eyelid flaps are still not sufficient to reconstruct a defect created by the excision of a lesion, a Burow or tension-releasing triangle can be performed or the incision can be extended into the malar region. Another possibility in full-thickness defects that affect more than a third of the length of the lower eyelid is the double mucosal and myocutaneous V-Y advancement flap with a subcutaneous pedicle, which is performed in a single operation, as described by Garcés et al.2(Fig. 8).
A, Basal cell carcinoma affecting the free border of the eyelid. B, The defect created was less than a quarter of the lower eyelid and an advancement flap was designed with a Burow triangle in the area adjacent to the lateral canthus. C, Suture with 5/0 silk. D, Result 20 days after the operation. The scar perpendicular to the free border prevented ectropion.
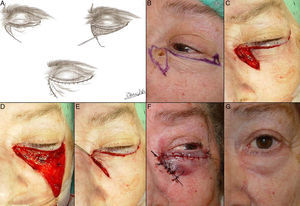
A, Design of an advancement flap. Drawing by Zaira González Fernández. B, Basal cell carcinoma at the medial canthus. C-E, Advancement flap for the lower eyelid and Burow triangle at the lateral canthus. F, Suture with 5/0 silk. Hematoma in the lower eyelid. G, Outcome 1 month after the operation.
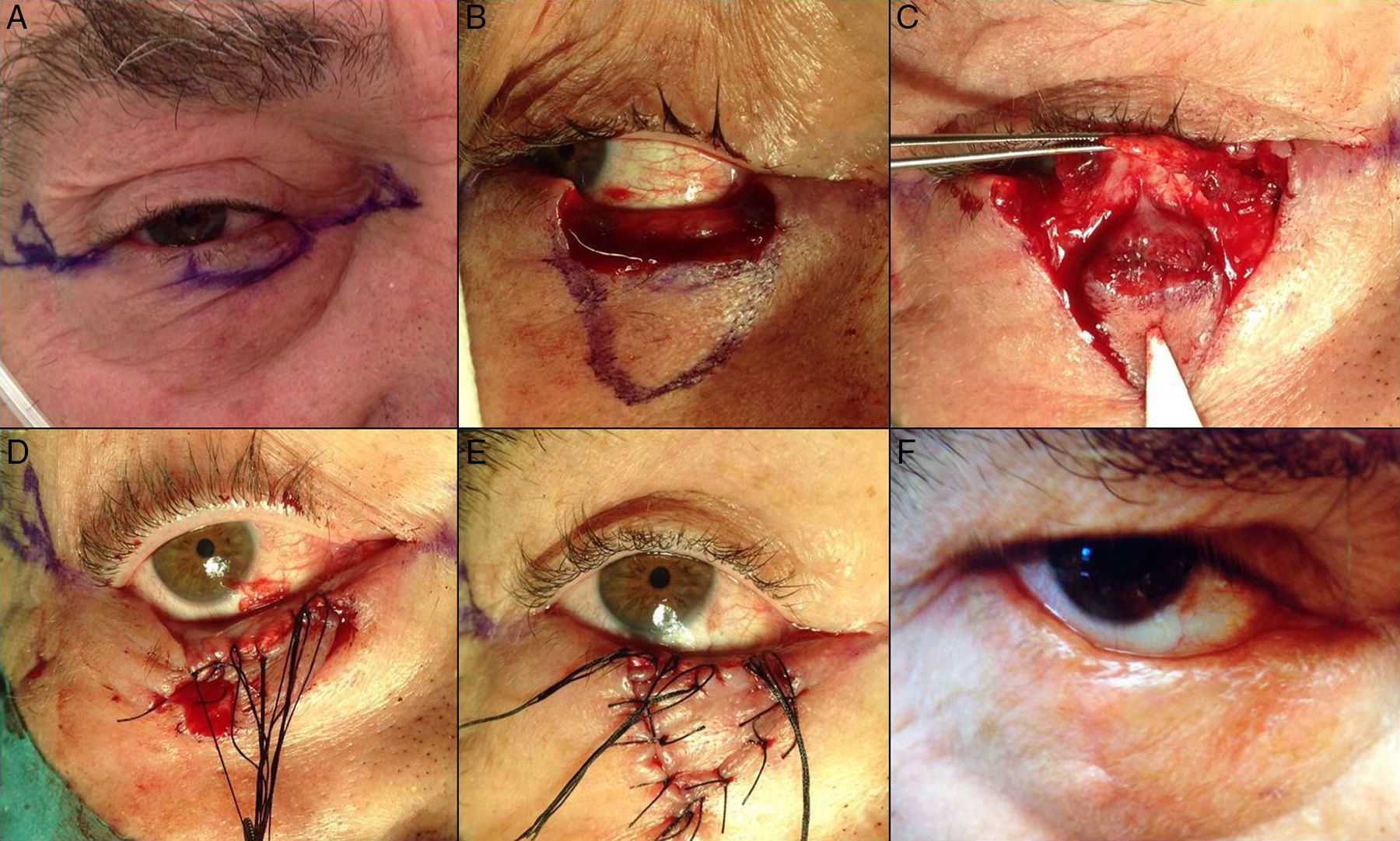
A, Poorly-defined squamous cell carcinoma that affected the lower eyelid up to its free border. B, Excision of the lesion, which included the full-thickness of the eyelid. C, Reconstruction using a double mucosal and myocutaneous V-Y advancement flap. D and E, V-Y advancement flap with a subcutaneous pedicle, sutured with 5/0 silk. F, Result 1 month after the operation, with slight exposure of the sclera.
An alternative technique for defects of the lower eyelid has been described by Moesen et al.3 This consists of the reconstruction of small to large defects of the lower eyelid using a local tarsoconjunctival advancement flap combined with advancement of the orbicularis oculi muscle and subsequently a skin graft. Other techniques that have been described are cartilage grafts, as proposed in 1987 by Matsuo et al.21 Those authors described a new method for reconstruction of the posterior lamella of the eyelid, consisting of the use of an autologous chondroperichondrial graft from the concha of the ear, with flaps from adjacent skin to restore the anterior lamella.17
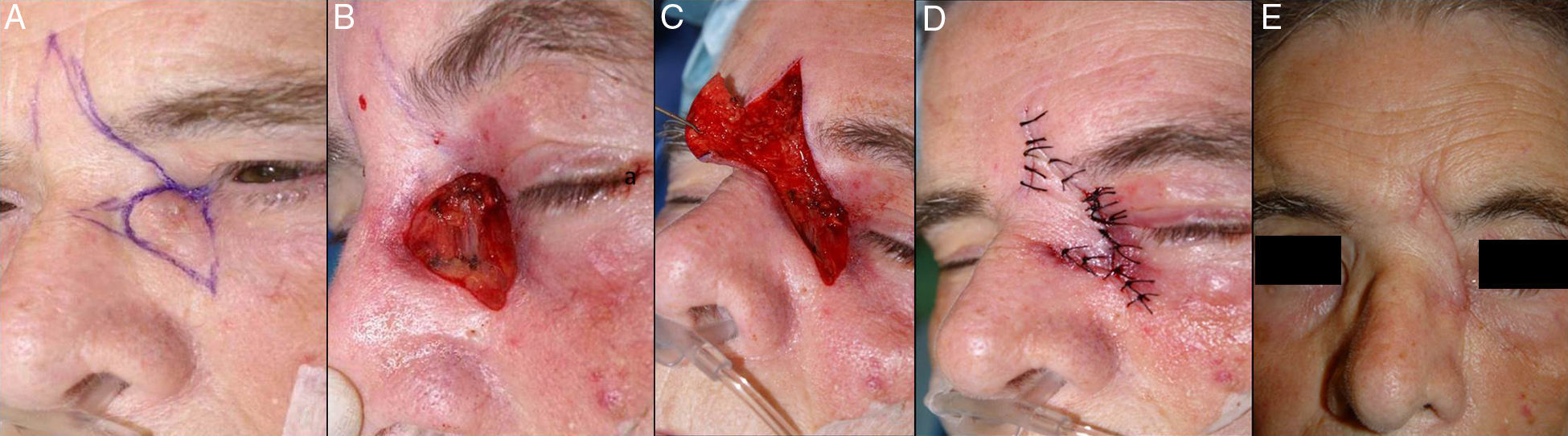
Defects at the Medial CanthusVarious reconstruction techniques, such as the lower eyelid advancement flap or the glabellar rotation flap, can be used to repair defects left by the resection of tumors affecting the area of the medial canthus (Figs. 9–11).
A, Basal cell carcinoma at the medial canthus. Glabellar rotation flap. B, Defect greater than 2cm at the medial canthus but not involving the punctum. C, Lifting of the glabellar area, advancement and rotation of the flap. D, Suture with 4/0 and 5/0 silk. E, Final outcome with slight thickening of distal part of the flap.
A, Basal cell carcinoma that infiltrated the punctum. B, Full-thickness resection leaving a defect of more than half of the lower eyelid. C, Double flap: glabellar flap and advancement flap of the lower eyelid. D, Final outcome showing slight thickening of the skin of the flap, which was corrected in a second operation.
A, Basal cell carcinoma affecting the medial canthus, lower eyelid and right side of the root of the nose. B, Excision of the lesion, which included the whole medial canthus. C, Design of a glabellar flap for reconstruction of the defect. D, Partial suture of the flap, making a minimal incision to adapt to the anatomic form of the medial canthus. E, Result after completing the suture of the flap.
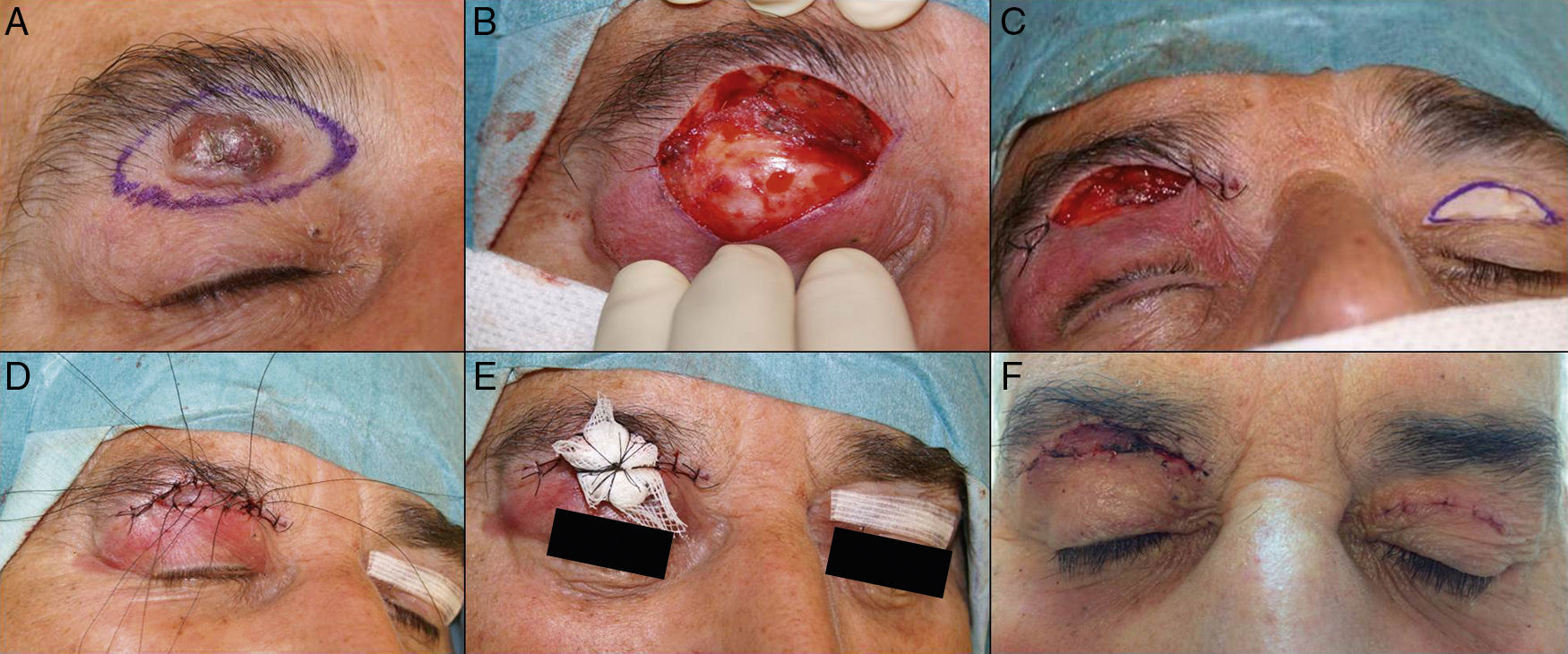
In full-thickness defects of the upper eyelid that involve less than 25% of the eyelid, reconstruction can be performed by direct closure.14,16 In larger defects, various plasties can be employed, such as the full-thickness flap (Cutler–Bread type) from the lower eyelid,7,14 or the forehead galeal-pericranial flap described by Brusati et al.16
When a full-thickness skin graft is used to reconstruct a defect of the upper eyelid, it can be obtained from the contralateral upper eyelid, as this will provide skin with a similar thickness, appearance, and texture to the recipient area22 (Fig. 12). The inferior limit of the optimal area for obtaining the skin for the graft is the superior palpebral fold; the area above this fold has the largest amount of redundant skin. If skin cannot be taken from the contralateral upper eyelid, the most suitable donor sites are the skin of the retroauricular fold or of the preauricular or supraclavicular folds.22
Complications in Palpebral SurgeryMaximum preservation of palpebral function is one of the most important objectives in palpebral surgery, attempting to maintain as far as possible the eye protection afforded by the eyelids and lacrimal drainage function. Certain complications must therefore be avoided: entropion, ectropion, lagophthalmos, epiphora, and corneal exposure. A rigid and stable palpebral margin must also be achieved, as this helps to prevent corneal trauma due to friction by the keratinized epithelium of the eyelid. In addition, the symmetry of the palpebral fissure should be maintained, not only because this could otherwise interfere with vision, but also because it is an important element of facial expression. Palpebral hematomas and edema are very common after palpebral surgery because of the laxity of the skin in this area, and patients must be warned of the possibility of their appearance, as the effect can sometimes be striking. Local application of cold dressings can help in their prevention or subsequent attenuation. Ectropion leads to exposure of the palpebral, bulbar, or corneal conjunctiva, which can cause dry eye and a lacrimation reflex; this may finally lead to complications such as chronic conjunctivitis, pain, and photophobia. To avoid this complication, scars should be vertical or perpendicular to the free palpebral border when the size of the tumor so permits. When a malar flap is used to close a defect in the lower eyelid, the malar incision must ascend diagonally, as this permits greater advancement of the flap and avoids ectropion. It must be ensured that the tension created is always horizontal and never vertical, and if a Burow triangle is created, it should not be made at the level of the malar incision or inferior to the lower eyelid. Lagophthalmos is a situation in which a patient cannot completely close the eyelids, with the consequent corneal exposure and risk of keratitis or ulceration; this can occur with surgery to the upper eyelid. To prevent these complications, the skin excision from the upper eyelid must not extend closer than 1cm to the lower border of the eyebrow. Epiphora is an accumulation of tear fluid that, though produced in normal quantity, cannot drain efficiently. This complication can be observed in tumors that affect the orifices of the lacrimal papillae, requiring their excision. In the glabellar flap for the correction of defects of the medial canthus, care must be taken to avoid the trap-door effect or thickening of the flap with respect to the skin of the eyelid to which it is sutured. To prevent this complication, which is mainly a cosmetic problem, it should be noted that although the plane of dissection is the subcutaneous cellular tissue, the flap should occasionally be thinned so that the thickness of the skin of the flap that is to be rotated is similar to that of the skin of the eyelid to which it is sutured. If a trap-door effect develops despite the above measure, it can be corrected in a second operation.
ConclusionPalpebral surgery is a challenge in dermatology because of the complex anatomy and function of the eyelids. It is essential to have good knowledge of the area, of the instruments, and of the various options available for reconstruction in order to perform consistently successful oncologic surgery associated with an acceptable functional and cosmetic result.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Iglesias ME, Santesteban R, Larumbe A. Cirugía oncológica de párpado y la región orbitaria. Actas Dermosifiliogr. 2015;106:365–375.