Respiratory tract infection due to Mycoplasma pneumoniae can provoke cutaneous and mucosal rashes, which have been classified within the spectrum of erythema multiforme or Stevens-Johnson syndrome. This classification is of therapeutic and prognostic importance and has generated intense debate in the literature. A recent systematic review of 202 cases of mucocutaneous rashes associated with M. pneumoniae infection concluded that these rashes might constitute a distinct entity, for which the term Mycoplasma-induced rash and mucositis was proposed. We describe a patient with acute M pneumoniae respiratory tract infection who presented mucosal and cutaneous lesions that were difficult to classify as erythema multiforme or Stevens-Johnson syndrome; the lesions were compatible with the proposed new disease.
La infección respiratoria por Mycoplasma pneumoniae (MP) puede producir erupciones cutáneo-mucosas que se han considerado parte del espectro eritema multiforme o del síndrome de Stevens-Johnson. La clasificación de estas reacciones cutáneas, que tiene importancia pronóstica y terapéutica, ha generado mucha controversia en la literatura. Recientemente, una revisión sistemática de 202 casos de erupciones mucocutáneas asociadas a infección por MP concluye que pueden constituir una entidad distinta para la que se propone la expresión Mycoplasma-induced rash and mucositis. Presentamos un caso de infección respiratoria aguda por MP con lesiones mucosas y cutáneas difíciles de clasificar como eritema multiforme o síndrome de Stevens-Johnson, y cuyas características son compatibles con la nueva enfermedad propuesta.
Mycoplasma pneumoniae infection affects the skin and mucosas in up to 25% of cases,1 and can cause erythema multiforme (EM)2 and Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN).3 The clinical overlap between these conditions, which has led to long-standing debate in the literature,4–9 makes diagnosis difficult in some cases.10,11 An extensive review of 202 cases of M pneumoniae-induced EM, SJS, and mucositis without rash was published recently.12 In their conclusions, the authors proposed a new entity which they called Mycoplasma-induced rash and mucositis. We present a case that we found difficult to classify and that was consistent with the new entity described. As suggested by those authors, we believe this entity could be helpful in the diagnosis and treatment of these cases in daily practice.
Case DescriptionThe patient, a previously healthy 16-year-old girl, presented a 7-day history of fever of 38.5°C, odynophagia, cough, and wheeze. She was diagnosed with acute bronchitis and received treatment with inhaled budesonide and ibuprofen. She was subsequently seen for the rapid onset of lesions on the skin and mucosas. She had not received other drugs and she did not report a history of herpes infection.
Physical examination revealed intense stomatitis with confluent ulcers and scabs affecting all of the lips and the oral, palatine, and pharyngeal mucosas, associated with bilateral conjunctival hyperemia with discharge. Numerous irregular, edematous erythematous plaques with central vesicles and an erythematous halo, giving them the appearance of atypical target lesions, were observed on the skin of the face, trunk, limbs, perineum, and genital mucosa (Fig. 1). The palms and soles were not affected. No tonsillar exudate was observed and there were no palpable lymph nodes in the head and neck. Auscultation of the chest revealed crepitations. Abdominal examination was normal.
A, Bilateral conjunctival hyperemia with discharge. B, Irregular, edematous erythematous papules with central vesicles and an erythematous halo, forming palpable atypical target lesions, widespread over the face, trunk, limbs, and perineal and genital mucosas, without affecting the palms and soles. C, Erosions, confluent ulcers, and scabs on the lips and mucosa. D, Changes in the skin lesions 2 days after onset of the rash. E, Detail of the atypical target lesions (corresponds to the area of the star in image B).
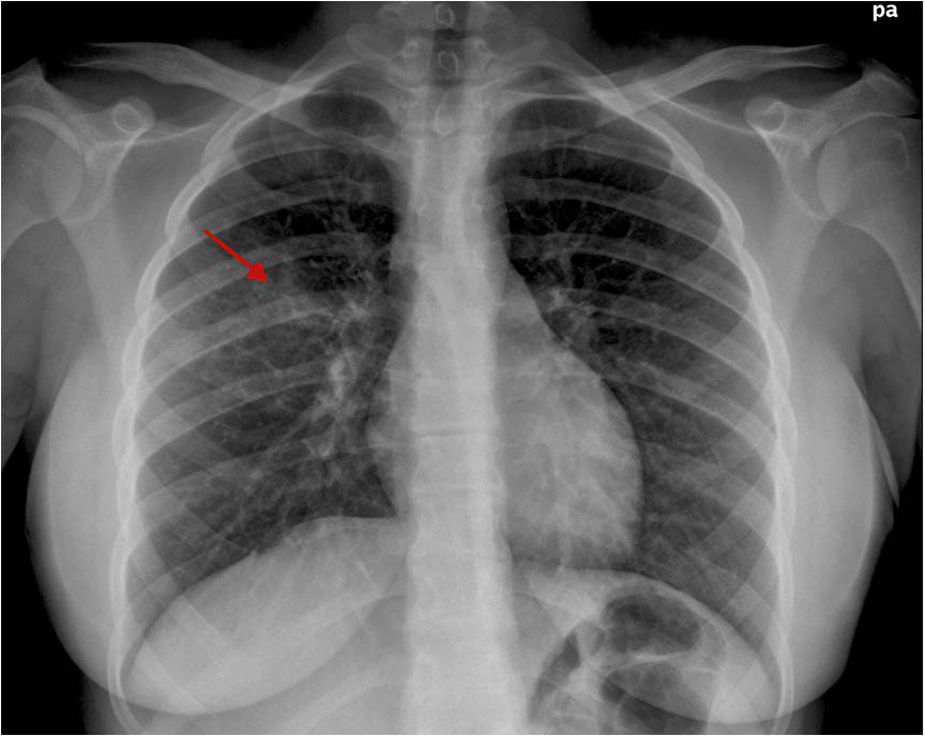
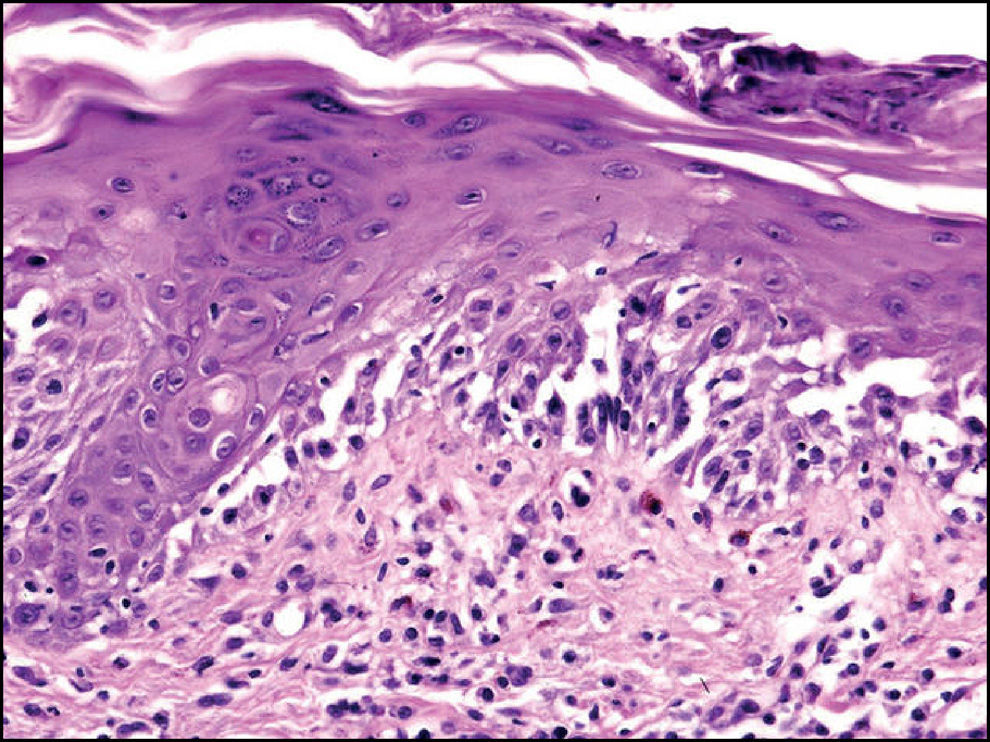
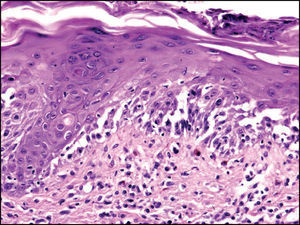
The patient was admitted with a clinical suspicion of erythema multiforme major secondary to M pneumoniae infection. Laboratory tests were as follows: C-reactive protein, 21mg/dL; anti-streptolysin O titer, 222U/mL; white cell count, 22850cells/μL (82.3% neutrophils, with no atypical lymphocytes); M pneumoniae IgM antibody, 292U; herpes simplex virus, Epstein-Barr virus, and cytomegalovirus serology, negative. Chest x-ray showed a pneumonia infiltrate in the right upper lobe (Fig. 2). Skin biopsy revealed an intense vacuolar interface lesion, isolated necrotic keratinocytes, and extensive dermoepidermal separation, with no epithelial necrosis (Fig. 3).
Treatment was started with intravenous methylprednisolone, 1mg/kg/d, clarithromycin, and acyclovir. The acyclovir was withdrawn after the serology results were received. Topical corticosteroids and antibiotics were applied to the conjunctival and oral mucosas, and fluid support and analgesia were administered until the patient's condition improved.
The skin lesions increased for a further 3 days, affecting up to 20% of the body surface, and took on a crusted, purpuric appearance, with lesions simultaneously observed in distinct stages. Some lesions developed flaccid blisters that did not coalesce or rupture. The Nikolski sign was negative and exfoliation did not occur. After 10 days the patient's condition had improved sufficiently for her to be discharged with only a residual hyperpigmentation.
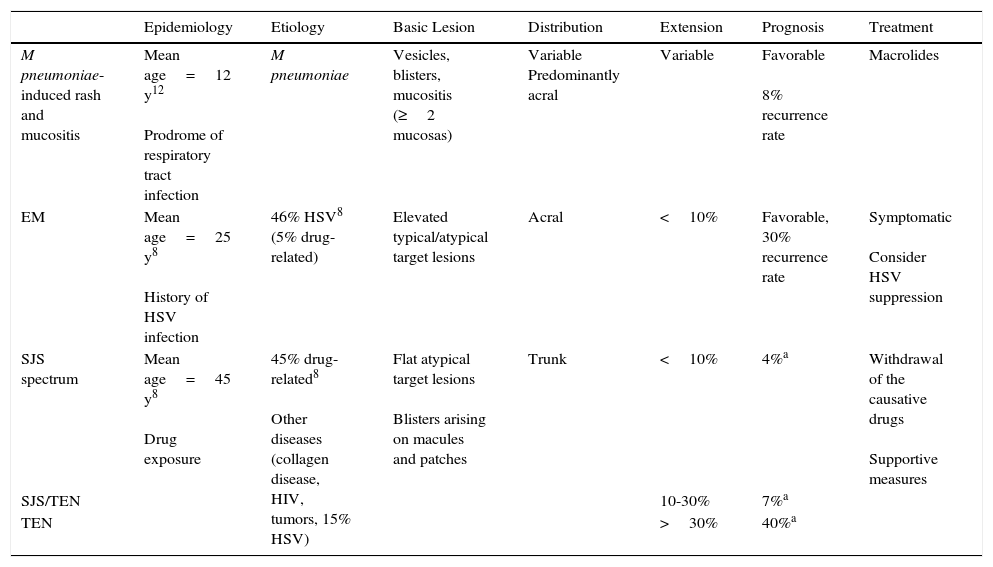
DiscussionM pneumoniae is implicated in up to 40% of atypical pneumonias, particularly in children and young adults.1 It provokes changes in the skin in up to a fourth of patients, with nonspecific rash being most common, though stomatitis, vaginal ulcers, pityriasis rosea, Kawasaki disease, leukocytoclastic vasculitis, subcorneal pustular dermatosis, Sweet syndrome, thrombotic thrombocytopenic purpura, Raynaud disease, Henoch-Schonlein purpura, and other conditions are also observed.10 The exact incidence of EM in children and young adults who develop infection due to M pneumoniae and other Mycoplasma species13 is unknown, while that of SJS has been estimated at approximately 5%, though these data may be affected by the confusing nomenclature.10,11 Because of the clinical overlap between these syndromes, EM, SJS, and TEN have for decades been considered part of a spectrum. However, the Severe Cutaneous Adverse Reactions study concluded that EM and SJS/TEN can be separated into 2 distinct groups based on their clinical characteristics.5 A later multicenter study confirmed the validity of that classification and its correlation with etiologic and prognostic factors,8 and the 2 conditions are now considered separate entities.9 It was difficult to confidently classify our patient into 1 of these groups, because the infectious origin, the acute onset, the target morphology of the lesions, and the favorable clinical course supported a diagnosis of EM, while the general symptoms, the central distribution with centripetal spread, and the large area affected by the lesions, together with intense involvement of 3 mucosas, was consistent with SJS. The differences between these conditions are summarized in Table 1.
Differences Between Mycoplasma-Induced Rash and Mucositis, Erythema Multiforme, and Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis Spectrum.
| Epidemiology | Etiology | Basic Lesion | Distribution | Extension | Prognosis | Treatment | |
|---|---|---|---|---|---|---|---|
| M pneumoniae-induced rash and mucositis | Mean age=12 y12 Prodrome of respiratory tract infection | M pneumoniae | Vesicles, blisters, mucositis (≥2 mucosas) | Variable Predominantly acral | Variable | Favorable 8% recurrence rate | Macrolides |
| EM | Mean age=25 y8 History of HSV infection | 46% HSV8 (5% drug-related) | Elevated typical/atypical target lesions | Acral | <10% | Favorable, 30% recurrence rate | Symptomatic Consider HSV suppression |
| SJS spectrum | Mean age=45 y8 Drug exposure | 45% drug-related8 Other diseases (collagen disease, HIV, tumors, 15% HSV) | Flat atypical target lesions Blisters arising on macules and patches | Trunk | <10% | 4%a | Withdrawal of the causative drugs Supportive measures |
| SJS/TEN | 10-30% | 7%a | |||||
| TEN | >30% | 40%a |
Abbreviations: EM, erythema multiforme; HSV, herpes simplex virus; SJS, Stevens-Johnson syndrome; TEN, toxic epidermal necrolysis.
In a study recently published by Canavan et al.,12 the authors reviewed the epidemiological and clinical characteristics of the 202 published cases of mucocutaneous rash associated with M pneumoniae. Their results, which we summarize here, led them to propose the creation of a new entity separate from the EM spectrum. Their patients were young (mean age, 11.9 years), with prodromal symptoms consisting of cough, malaise, and fever the week prior to the skin rash. The distribution of the lesions was acral in 46%, widespread in 31%, and on the trunk in 23%; lesion morphology was variable, the most common forms being vesicles and blisters (77%) and target lesions (48%). Mucosal involvement was intense and was fundamental to the diagnosis. Most common was oral mucositis, which occurred in 94% of cases, followed by bilateral purulent conjunctivitis (82%) and involvement of the urogenital mucosa (63%). The mean number of mucosas affected was 2.5. The disease had a benign course in the majority of patients, with complete recovery in 81%. Only 4% of patients required management in an intensive care unit according to that review article, and the estimated mortality was 3%. Patients were mainly treated with antibiotics (80%) and systemic corticosteroids (35%); a minority (8%) received intravenous immunoglobulin. Recurrence rates were not particularly high (8%). Those authors concluded that the etiology, lesion morphology, and clinical course, as well as the potentially distinct treatment of these patients, justified the designation of a clinical entity distinct from classic herpes simplex virus-associated EM and from drug-induced SJS/TEN. They proposed the term Mycoplasma-induced rash and mucositis (MIRM). This new classification is particularly useful in cases of extensive mucositis due to M pneumoniae without skin rash (MIRM sine rash for those authors), which did not adapt to the previous classifications and which could be due to certain strains of M pneumoniae.
The etiologic and pathogenic hypothesis is that MIRM is caused by the production of immunoglobulins by proliferating clones of B cells, and that this leads to immune complex deposition in the skin and to the activation of complement. This also differentiates the condition from EM and from SJS/TEN, which are caused by a type IV delayed hypersensitivity reaction and by Fas-ligand-mediated cytotoxicity.
ConclusionOur case is compatible with those described by Canavan et al., and its classification within this new entity would dispel the diagnostic doubts that persisted after applying the criteria of the Severe Cutaneous Adverse Reactions study. We would therefore favor accepting the proposal of those authors.
The classification of the severe mucocutaneous diseases secondary to infections and drugs is complex due to the clinical overlap between them. After decades of controversy, EM was separated from SJS/TEN in 2002.8 Likewise, in 2013, drug reaction with eosinophilia and systemic symptoms (DRESS) was separated from the SJS spectrum.14 Acceptance of MIRM as an independent entity could facilitate correct diagnosis and more adequate treatment of our patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this research.
Confidentiality of dataThe authors declare that they followed their hospital's regulations regarding the publication of patient information.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr. Paola Barón Rodiz, of the radiology department of our hospital, for her collaboration.
Please cite this article as: Martínez-Pérez M, Imbernón-Moya A, Lobato-Berezo A, Churruca-Grijelmo M. Exantema mucocutáneo inducido por Mycoplasma pneumoniae: ¿un nuevo síndrome separado del eritema multiforme? Un nuevo caso y revisión de la literatura. Actas Dermosifiliogr. 2016;107:e47–e51.