Port wine stains (PWSs) are commonly treated by the pulsed dye laser. However, treatment of hypertrophic or resistant PWSs is a major therapeutic challenge. The long-pulsed Alexandrite laser could be a safe and effective treatment for resistant PWSs, due to an increase depth of penetration of 50–75% over PDL.
ObjectiveThe aim of this study was to assess the efficacy and safety of a long-pulsed Alexandrite laser in patients with hypertrophic, dark and/or resistant PWSs. Pink pale resistant PWS were excluded from the study.
MethodsTwenty-one patients (age 20–75 years), phototypes I–IV on the Fitzpatrick scale, with PDL dark resistant PWSs were treated with long-pulsed Alexandrite laser. We excluded high phototypes and PDL pink resistant PWSs. All patients were treated with 3 laser sessions at settings of 3-ms pulse duration, 10-mm spot, 35–55J/cm2, with cooling (Dynamic Cooling Device 50ms with delay 30ms). Laser sessions were repeated approximately every 2 months. Three dermatologists evaluated treatment effectiveness by means of photographs of the patients before and after laser treatment (scale from 0 to 4). Adverse events were registered. Patient satisfaction was also assessed (scale from 0 to 10).
ResultsMean global improvement was rated as 2.28. Long-lasting side effects included minimal scarring after blistering in 1 patient. Mean patient satisfaction was 8.5.
ConclusionsOur study concludes that long-pulsed Alexandrite laser was effective for treatment of resistant PWSs, although the therapeutical window is narrow with this treatment.
Las manchas en vino de oporto (MVO) son normalmente tratadas con láser de colorante pulsado. Sin embargo, el tratamiento de MVO hipertróficas o resistentes continúa siendo un importante reto terapéutico. El láser de Alejandrita de pulso largo podría ser un método seguro y eficaz para el tratamiento de estas lesiones, debido a que la profundidad que alcanza puede superar entre un 50–75% al láser de colorante pulsado.
ObjetivoEl objetivo de este estudio fue evaluar la eficacia y la seguridad del láser de Alejandrita de pulso largo en pacientes con MVO hipertróficas y/o resistentes. Los pacientes con MVO resistentes de color rosa pálido fueron excluidos del estudio.
MétodosVeintiún pacientes (Edades entre 20–75 años), fototipos I-IV en la escala Fitzpatrick, con MVO oscuras, resistentes al tratamiento con láser de colorante pulsado fueron tratados con láser de Alejandrita de pulso largo. Se excluyeron los fototipos altos y las MVO de color rosado pálido. Todos los pacientes fueron tratados con 3 sesiones de láser con los siguientes parámetros: duración de pulso de 3ms, spot de 10mm de diámetro, fluencias comprendidas entre 35 y 55J/cm2, con refrigeración (Dynamic Coolong Device). El intervalo de tiempo entre sesiones fue de 2 meses aproximadamente. Tres dermatólogos evaluaron la efectividad del tratamiento a través de las fotografías de los pacientes antes y después del tratamiento con láser (escala de 0 a 4). Se registraron los eventos adversos acontecidos. La satisfacción del paciente también se evaluó (escala de 0 a 10).
ResultadosLa mejoría global media fue de 2,28. Los efectos adversos duraderos fueron lesiones cicatriciales mínimas en un paciente. La satisfacción media de los pacientes fue de 8,5.
ConclusionesNuestro estudio concluye que el láser de Alejandrita de pulso largo puede ser eficaz en el tratamiento de MVO resistentes, aunque la ventana terapéutica es estrecha con este tratamiento.
Port Wine Stains (PWS) are congenital capillary malformations that affect 0.3% of all births.1 The concept of selective photothermolysis with the 585-nm pulsed dye laser (PDL) revolutionized treatment of relatively common port wine stain (PWS) birthmarks. The majority of PWS can be significantly lightened with the PDL. However, few PWS are lightened completely with PDL and up to 20% hardly lighten at all. PDL-resistant PWS exist in any large cutaneous laser practice and constitute a difficult management problem.
Clinically it is difficult, if not impossible to predict which PWS will or will not respond to PDL before initiating treatment.2
Generally, factors resulting in decreased treatment efficacy include those that reduce light penetration, such as superimposed vasculature, high melanin content, and an increased PWS vascular density, diameter, or depth.3–7
The purpose of this article is to report our experience in the treatment of patients with purple, hypertrophic and/or resistant PWS with a long-pulsed 755-nm Alexandrite laser. Treatment response, safety parameters and patient satisfaction were evaluated. Histochemical analysis correlation of nine consenting patients confirmed vessel damage selectivity.
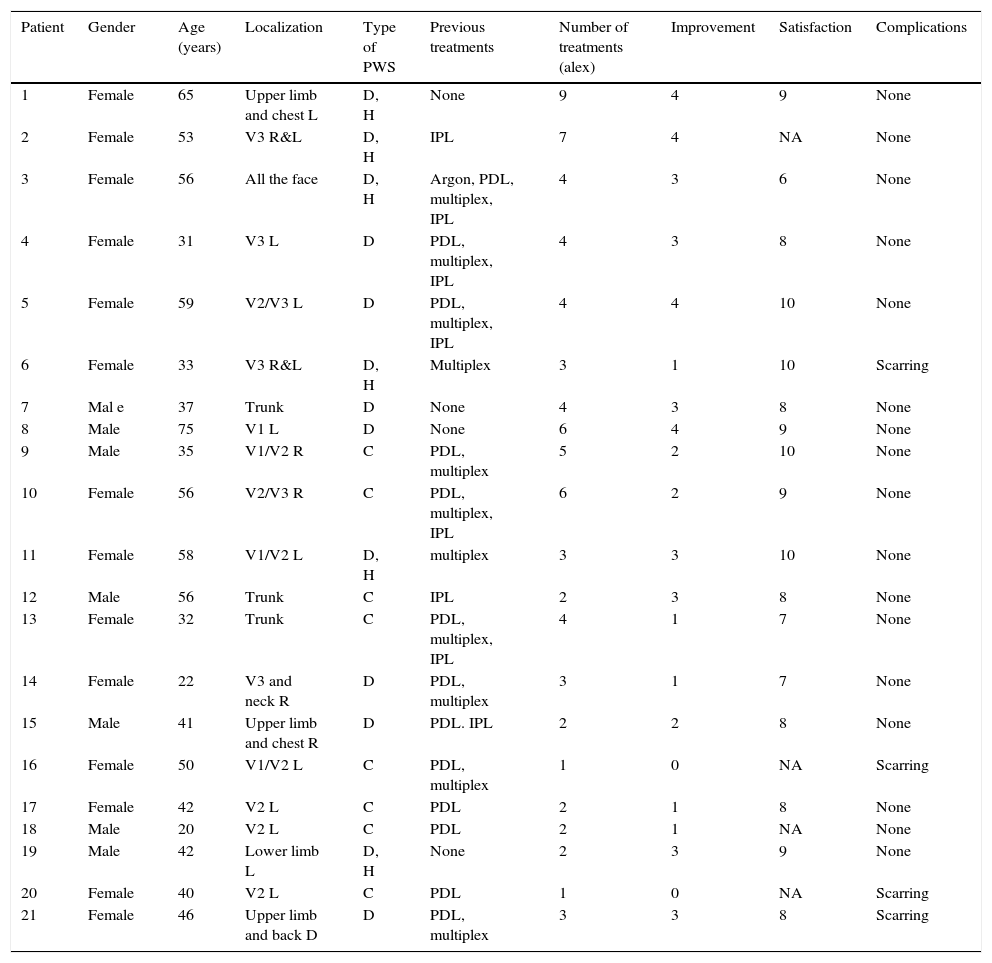
Materials and methodsThis prospective study included 14 females and 7 males patients, phototypes I–IV on the Fiztpatrick scale, with hypertrophic, dark and/or resistant PWS. We excluded high phototypes and PDL pink resistant PWSs because of the higher risks of side effects for the intense absorption of 755nm laser light by melanin. Their age ranged from 20 to 75 years (median 45, 19 years). Patients were treated in the Dermatology Department of Ramon y Cajal Hospital from January 2012 to October 2012. Most lesions were located on head or neck region (n=14), but lesions on extremities and trunk (n=7) were also treated. PDL resistant PWSs were defined as no result or no more improvement with PDL treatment. Table 1 shows the clinical characteristics and previous treatments of the patients. The hospital's ethics committee approved the study. Fully informed written consent was obtained from all patients before the first treatment.
Clinical characteristics, previous treatments, clinical results, patients’ satisfaction and side effects.
| Patient | Gender | Age (years) | Localization | Type of PWS | Previous treatments | Number of treatments (alex) | Improvement | Satisfaction | Complications |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 65 | Upper limb and chest L | D, H | None | 9 | 4 | 9 | None |
| 2 | Female | 53 | V3 R&L | D, H | IPL | 7 | 4 | NA | None |
| 3 | Female | 56 | All the face | D, H | Argon, PDL, multiplex, IPL | 4 | 3 | 6 | None |
| 4 | Female | 31 | V3 L | D | PDL, multiplex, IPL | 4 | 3 | 8 | None |
| 5 | Female | 59 | V2/V3 L | D | PDL, multiplex, IPL | 4 | 4 | 10 | None |
| 6 | Female | 33 | V3 R&L | D, H | Multiplex | 3 | 1 | 10 | Scarring |
| 7 | Mal e | 37 | Trunk | D | None | 4 | 3 | 8 | None |
| 8 | Male | 75 | V1 L | D | None | 6 | 4 | 9 | None |
| 9 | Male | 35 | V1/V2 R | C | PDL, multiplex | 5 | 2 | 10 | None |
| 10 | Female | 56 | V2/V3 R | C | PDL, multiplex, IPL | 6 | 2 | 9 | None |
| 11 | Female | 58 | V1/V2 L | D, H | multiplex | 3 | 3 | 10 | None |
| 12 | Male | 56 | Trunk | C | IPL | 2 | 3 | 8 | None |
| 13 | Female | 32 | Trunk | C | PDL, multiplex, IPL | 4 | 1 | 7 | None |
| 14 | Female | 22 | V3 and neck R | D | PDL, multiplex | 3 | 1 | 7 | None |
| 15 | Male | 41 | Upper limb and chest R | D | PDL. IPL | 2 | 2 | 8 | None |
| 16 | Female | 50 | V1/V2 L | C | PDL, multiplex | 1 | 0 | NA | Scarring |
| 17 | Female | 42 | V2 L | C | PDL | 2 | 1 | 8 | None |
| 18 | Male | 20 | V2 L | C | PDL | 2 | 1 | NA | None |
| 19 | Male | 42 | Lower limb L | D, H | None | 2 | 3 | 9 | None |
| 20 | Female | 40 | V2 L | C | PDL | 1 | 0 | NA | Scarring |
| 21 | Female | 46 | Upper limb and back D | D | PDL, multiplex | 3 | 3 | 8 | Scarring |
R (right), L (left), D (dark), H (hypertrophic), C (clear) PDL (pulse dye laser), IPL (intense pulse light), multiplex (dual wavelength 595–1064nm laser), NA (not available).
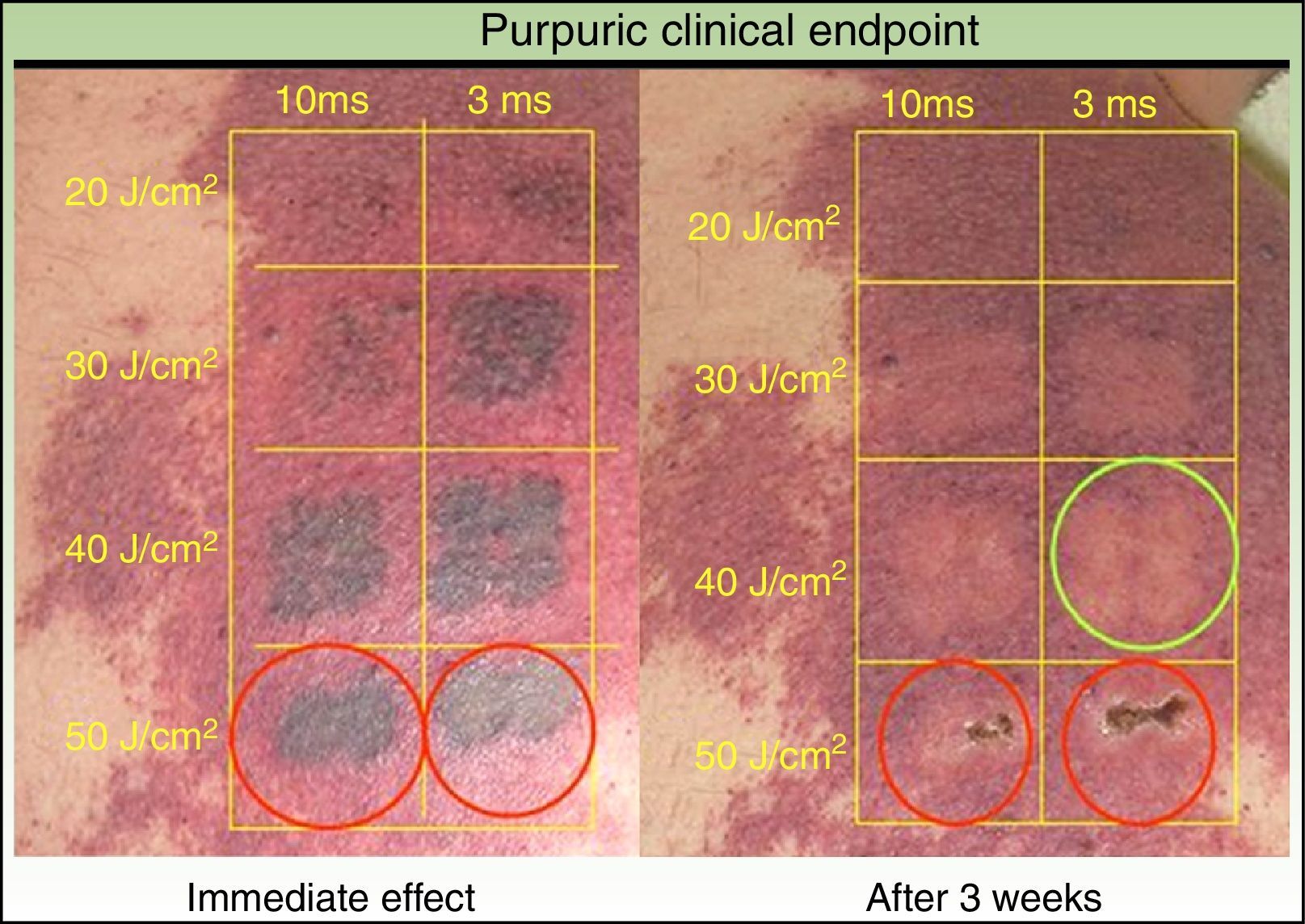
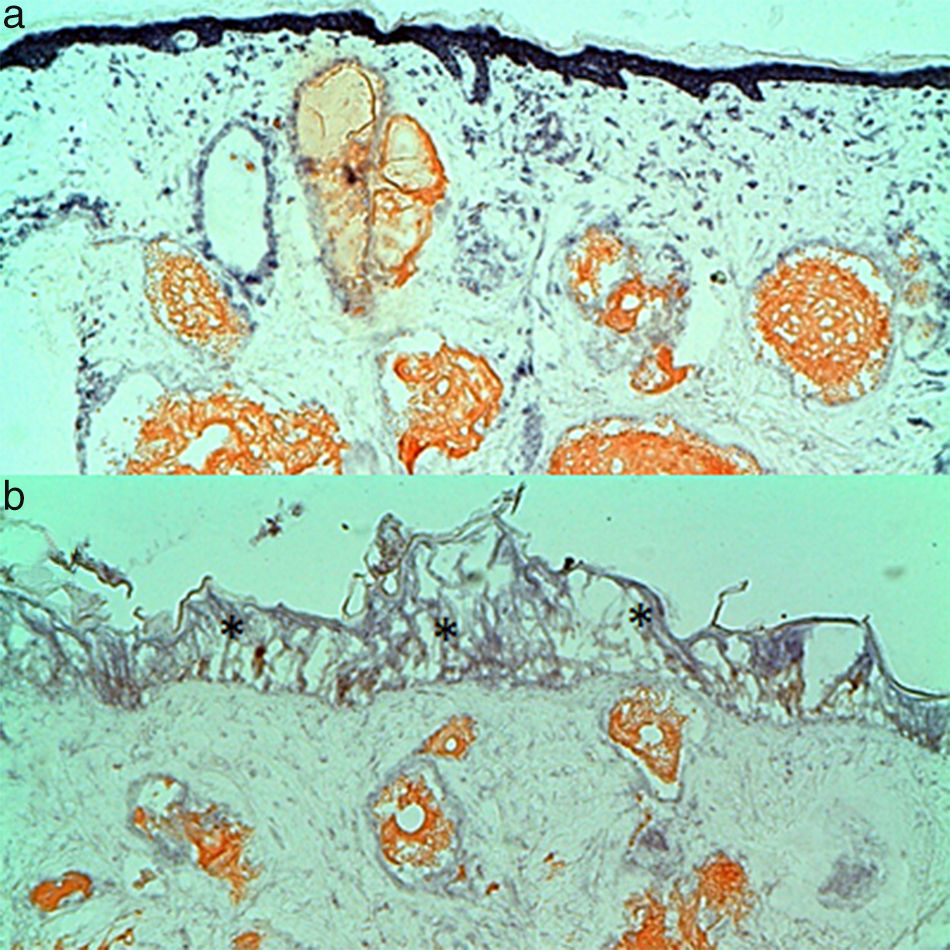
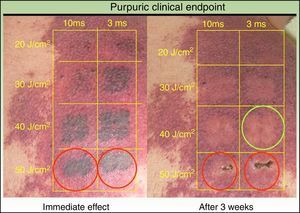
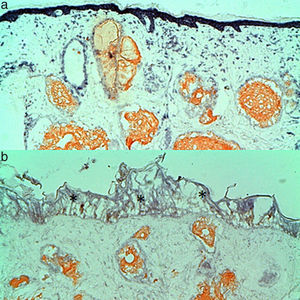
PWSs were treated with the 755nm-Alexandrite laser (Gmax, Candela & V-beam, Candela). Before each laser treatment, a cream containing a lidocaine base and a prilocaine base (Eutetic Mixture of Local Anesthetics, EMLA©, AstraZeneca, Wedel, Germany) was applied topically under occlusion during 1h to reduce pain on cutaneous lesions. Parameters used were: 10mm spot size with 3ms fixed pulse and 35–55J/cm2, with epidermal cooling (Dynamic Cooling Device 50ms with delay 30ms). There were no double-pulsed areas. The optimal fluence settings were chosen following the achievement of purpura as a clinical endpoint base (looking for a transient gray color that gradually evolves into persistent deep purpura which is the correct therapeutic finding).11 We tested different fluences and spot sizes for each patient in small areas of the PWS to achieve purpura. Post-treatment biopsies using a 4-mm punch were performed in 9 consenting patients after the single treatment of a test area. Biopsy specimens were frozen in liquid nitrogen and the tissue sections were stained with NTBC to make the histochemical correlation and to confirm selective vessel damage as described in studies with the PDL and the argon laser.4 This enzyme is a redox indicator that is reduced by NADPH-diaphorase. The enzymatic activity stops immediately after cell death and it is present in the endothelial cells, fibroblasts and smooth muscle but not in the dermis connective matrix. Therefore, only the viable tissue stains blue, allowing easy differentiation from thermally damaged tissue.
DCD (Dynamic Cooling Device) was set to: 50ms spurt duration pre-treatment with 30ms delay and 30ms spurt duration post-treatment for epidermal protection.
Post-laser care consisted of a daily application of topical antibiotic ointment (fusidic acid, Fucudine™, LEO Pharma, Barcelona, Spain) for a week and sunscreen with a sun protection factor of 50 up to two months after therapy to prevent postinflammatory hyperpigmentation when lesions where located on skin. Three treatment sessions spaced two months between each other were performed.
Three dermatologists evaluated treatment effectiveness by photographic means before starting and at a minimum of one month after finishing the last treatment session. Color, elevation and cutaneous texture of the PWS were considered. The clinical response was evaluated as ‘4’ (76–100% improvement), ‘3’ (51–75%), ‘2’ (26–50%), ‘1’ (1–25%) or ‘0’ (no improvement or worsening). The reviewers also evaluated the presence of side effects in the photographs including scarring, hyperpigmentation, and hypopigmentation. Patients’ satisfaction was rated on a scale from ‘0’ to ‘10’, ‘0’ being the lowest and ‘10’ the maximum value.
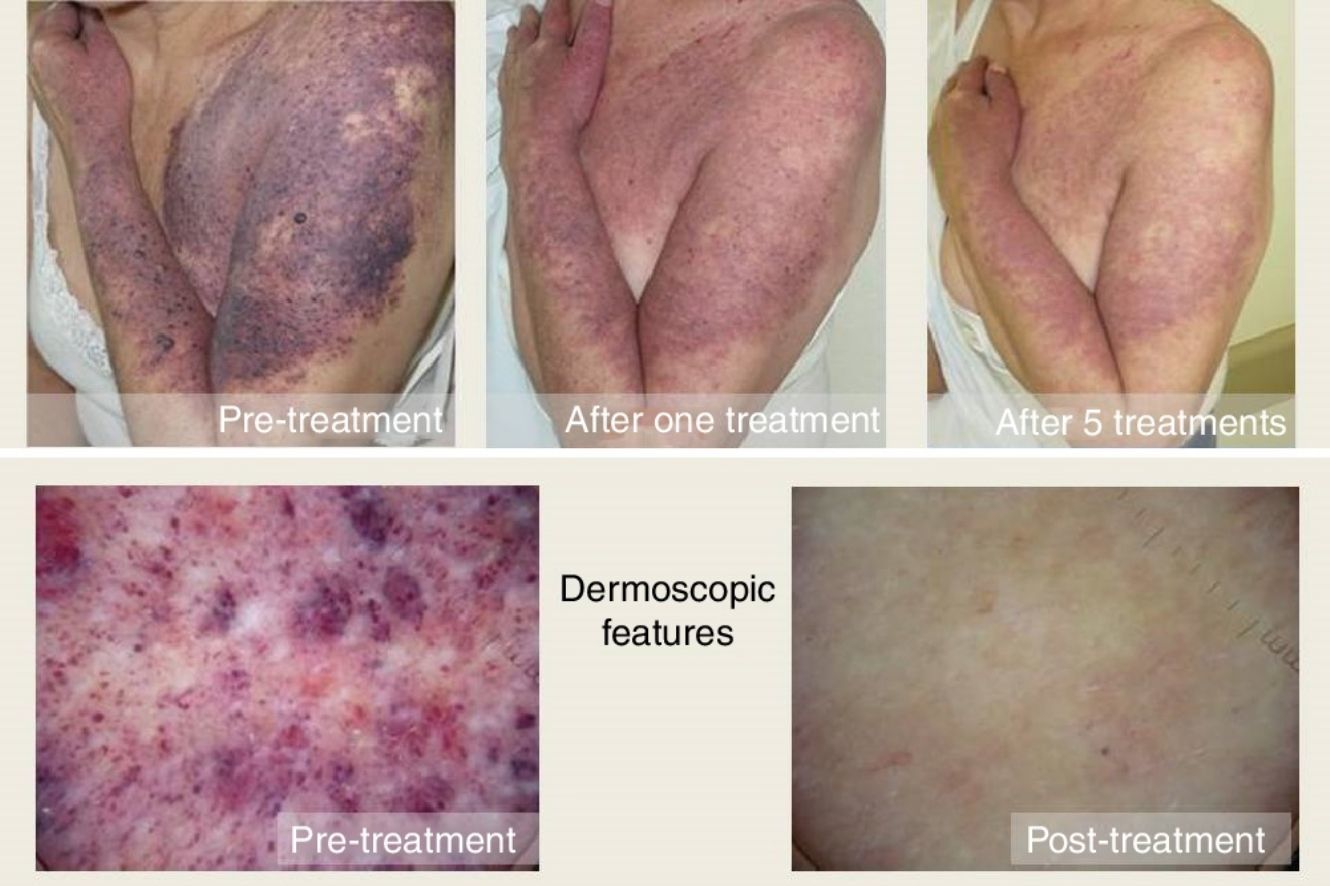
ResultsClinical results, patients’ satisfaction and side effects are shown in Table 1. Three laser treatment sessions were performed in each patient. The mean global improvement was 2.28. The success rate (complete or partial resolution) of laser treatment was higher than 75% in 4 patients, between 75 and 50% in 7 patients, between 50 and 25% in 3 patients, lower than 25% in 5 patients and 2 patients did not show any improvement. The most significant lightening was observed in patients with hypertrophic and/or dark PWS (Figs. 1 and 2) and the worst results were obtained in patients with flat dark PWSs. Side effects were usually transient and predictable, including mild to moderate pain, mild edema, erythema and purpura, however it did not require discontinuation of the treatment. Long-term complications were noted, except minimal scarring after blistering in 1 patient. Degree of satisfaction ranged from 6 to 10 and mean of satisfaction was 8.47.
The correct therapeutic clinical endpoint (Fig. 3) (transient gray color that gradually evolves into persistent deep purpura) was correlated with a coagulation and wall destruction of dermal vessels with preserved epidermis in the histochemical analysis (Fig. 3, green circle). However, a suboptimal clinical endpoint (immediate slight gray color that immediately fades) showed absence of dermal vessel wall destruction and/or coagulation. An overtreatment area (persistent gunmetal gray or white color) showed coagulation and wall destruction of dermal superficial vessels with epidermal damage (Fig. 4, red circle). The same laser settings in different patients got different clinical endpoints, grades of clinical improvement and histochemical selectivity. Maintaining the same laser parameters, we observed a different clinical response for each patient and a different histochemical selectivity due to architectural differences in the vessels of each patient.
(a) Complete coagulation and wall destruction of dermal vessels with preserved epidermis in the histochemical analysis. The histological picture corresponds to the green circle in Fig. 3. (b) High fluences lead to intense epidermal (*) and dermal tissue damage. Note the permanent gray in the central area following treatment with high fluence (Fig. 3, red circle).
Most adult patients with hypertrophic, dark and/or resistant PWS present some grade of improvement after Alexandrite laser therapy with few complications. Particularly, the best results were observed in patients with dark hypertrophic PWS which showed significant improvement; the worst results were obtained in patients with flat PWSs. It is likely that these malformations with small, deep vessels show no improvement in this type of laser with longer thermal relaxation time. Li et al.8 compared the efficacy and complications of the long-pulse pulsed dye laser (LPPDL) and the long-pulse pulsed Alexandrite laser (LPPAL) in the treatment of PWSs. They concluded that LPPAL works best with hypertrophic, purple PWS, while LPPDL yields better clinical improvements with the flat, pink PWS but a risk of dyspigmentation exists when using the LPPAL. Due to the depth of penetration of the Alexandrite laser in the skin and its capacity to produce deep dermal damage, including scarring, it is important to use a correct tissue response endpoint. A transient gray color that evolves into deep purpura is the optimal clinical endpoint and it may be observed after 1 or 2min of watchful waiting after test pulse.9
We agree with these authors and accept the correct therapeutic clinical endpoint with a transient gray color that gradually evolves into persistent deep purpura. This endpoint was correlated with a coagulation and wall destruction of dermal vessels with preserved epidermis in the histochemical analysis. However, a suboptimal clinical endpoint (immediate slight gray color that immediately fades) showed absence of dermal vessel wall destruction and/or coagulation. An overtreatment area (persistent gunmetal gray color) showed coagulation and wall destruction of dermal superficial vessels with epidermal damage. The same laser settings in different patients got different clinical endpoints, grades of clinical improvement and histochemical selectivity. Maintaining the same laser parameters, we observed a different clinical response for each patient and a different histochemical selectivity. For this reason, careful attention to tissue response endpoints and constant readjustment of fluences based on such responses are important during the course of each treatment. The reasons for such difference in responses remain unknown but illustrate the considerable intralesional heterogeneity of PWS.
Tierny et al.10 treated 8 patients with PDL resistant PWSs with long pulsed Alexandrite laser with similar results to our study. After an average of 2.6 laser sessions they found improvements in color (56.3% improvement), texture (59.4% improvement) and cosmetic skin (62.6% improvement).
Izikson et al.11 treated hypertrophic PWS and showed significant lightening after treatment with a 755nm laser in combination with PDL. Most PDL-resistant PWS showed moderate improvement after treatment with either a 755nm laser alone or in combination with another laser, including PDL. Serious side effects were infrequent.
When using the correct skin cooling cryogen spray parameters for epidermal protection and teaching the precise clinical endpoint, the treatment with 755-nm Alexandrite laser produces relatively few serious complications.12 All the patients display some pain, edema, transient purpura and erythema during or after therapy. If necessary, treatment can be performed under topical or general anesthesia or with the use of preoperative narcotic analgesics and sedatives. Permanent removal of dark hair is expected and should be discussed with the patient prior to treatment. Occasional mild superficial blistering and subsequent mild desquamation and transient or long-lasting pigmentation changes are other side effects that may occur despite the use of the correct endpoint.
Although serious side effects are rare after Alexandrite laser treatment, the use of a supra-therapeutic clinical endpoint is likely to produce a dermal burn and skin necrosis that could lead to scarring. In our series of cases, there was one case of minimal scarring. More experience is needed with Alexandrite laser due to its narrow therapeutic window.
Patients’ satisfaction was very high. The grade of improvement of their lesions was the major factor to evaluate their satisfaction.
Histochemical analysis using NTBC stain allows a simple and highly sensitive assessment of cell viability. NBTC enable us to establish the best parameters to evaluate the results of different laser treatment parameters on vessel wall destruction or epidermal sparing.
A limitation of this study is that the low number of patients and the absence of comparable groups do not allow us to realize a statistical study to compare the clinical results in the different types of PWS. Another limitation of the study is the exclusion of people with higher phototypes and pink pale PWSs.
ConclusionThis study allows us to conclude that Alexandrite laser could be a good therapeutic alternative for hypertrophic, dark and/or resistant PWS due to the good results obtained. The Alexandrite laser needs more experience along with other lasers because of its narrow therapeutic window.
Ethical disclosuresProtection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestThe authors declare no conflict of interest.