Measles is a highly contagious disease caused by a virus of the Paramyxoviridae family. Since humans are the only reservoir of the virus and an effective vaccine exists, measles is considered to be a potentially eradicable disease. In 1998, the World Health Organization's Regional Office for Europe established the goal of eradicating indigenous measles from the region by 2007. However, since 2009 there have been several outbreaks of the disease.1–3 These outbreaks have affected practically all age groups and have been associated with a decrease in vaccination rates, which is probably the result of a fear of possible side effects on the part of parents and the existence of marginal social groupings whose members do not use the public health services.4,5
An outbreak of measles affecting our area (Alicante, health district 19 in the Community of Valencia) has afforded us the opportunity to observe several cases of measles in our hospital. Preliminary data obtained from the Epidemiology Department of the public health authorities in Alicante indicate that 339 cases of measles were recorded in our health district between January 1 and April 1 2012. In 170 cases, the diagnosis was confirmed by serology and in 112 by epidemiological link. Confirmation is still pending in the remaining cases. The age of affected patients ranges from 2 months to 60 years, with a predominance of patients over 20 years of age (127 cases); both sexes were affected equally (55.16% men). In total, 40 patients (12%) required hospitalization. Complications detected to date include 37 cases of otitis and 9 of pneumonia; there have been no deaths.
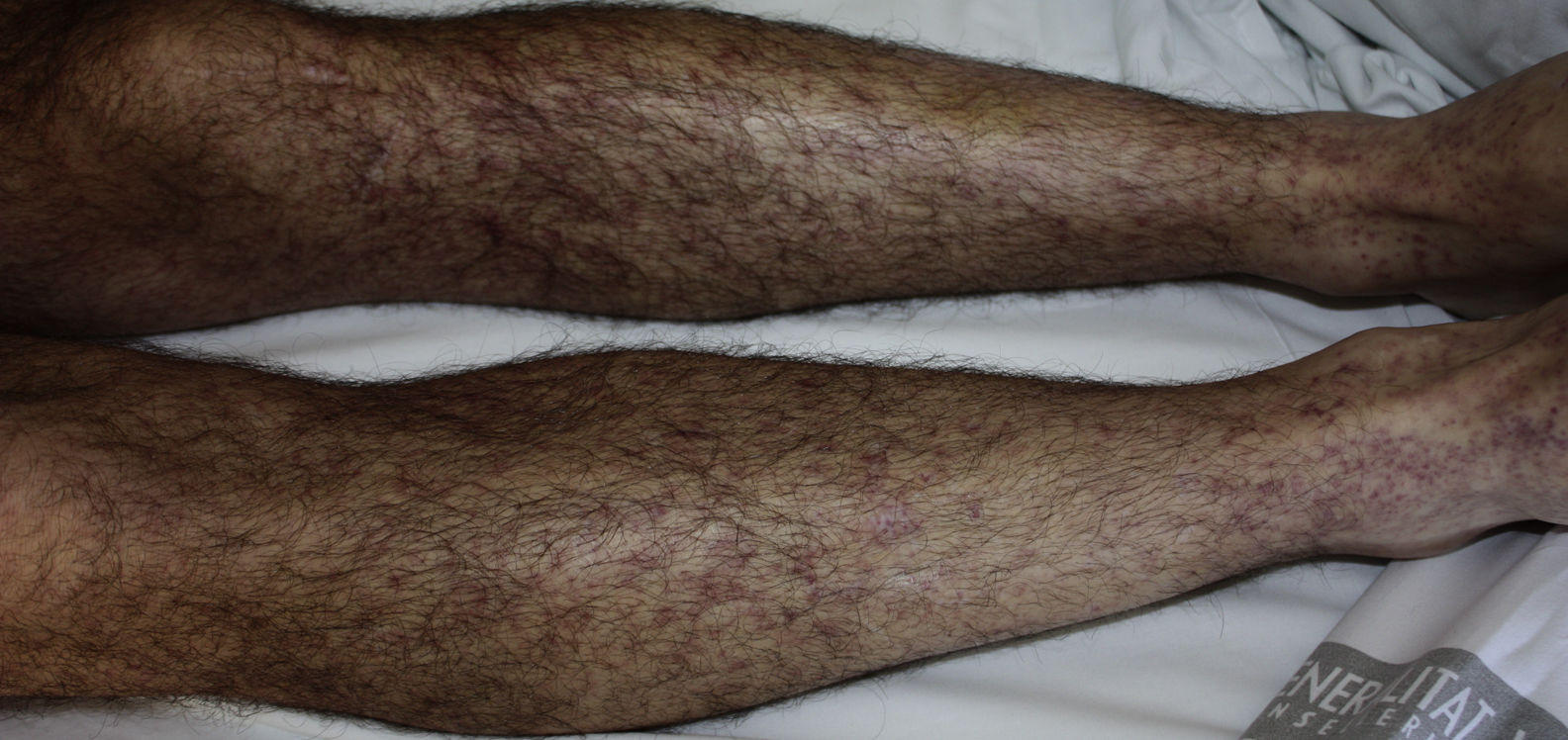
We recently attended 2 patients hospitalized with measles. The patients were 2 men of Spanish nationality aged 31 and 28 years who presented with the typical clinical picture: a prodromal phase of fever and general malaise followed by the development of a diffuse nonpruritic rash several days later. In both cases, the rash had started on the head and later spread to the trunk (Fig. 1) and limbs (Fig. 2). The maculopapular and confluent rash was associated with marked involvement of the eyes in the form of nonpurulent bilateral conjunctivitis with photophobia. Of note was the fact that neither of these patients presented the characteristic Koplik spots, which have been described as pathognomonic but actually appear in a variable percentage of cases (50%-70%).6,7 The reason for admission in both cases was the patient's generally deteriorated condition. Serology for exanthematous viral disease, which yielded a positive result for immunoglobulin M for measles, finally provided the key to the diagnosis. Neither of the 2 patients remembered having been vaccinated against measles. The patients were discharged following symptomatic treatment after 3 and 4 days, respectively.
The purpose of this letter is to highlight the continuing presence of measles today, as has been demonstrated by the present outbreak in our health district and those that have occurred elsewhere in Spain and the rest of Europe. Although measles has been somewhat forgotten in recent years because of its low incidence, it should be kept in mind and included in the differential diagnosis in febrile patients presenting with rash.
We would like to thank Dr. María Vicenta Rigo Medrano, Head of the Epidemiology Department of the Public Health Center of Alicante for providing the epidemiological data that appear in this article.
Please cite this article as: Latorre N, Blanes M. El sarampión como enfermedad reemergente. Actas Dermosifiliogr. 2013;104:533-4.