Necrobiosis lipoidica (NL) is an uncommon degenerative disorder of unknown etiology that affects connective tissue. Although very often associated with diabetes mellitus, NL does occur in nondiabetic patients.1,2
The diagnosis of NL has traditionally been based on clinical presentation and histologic findings, which are distinctive in many cases. However, atypical presentations and variations in the appearance of the lesions as they evolve can make diagnosis difficult.1,2 We report the cases of 3 patients with NL lesions at different stages with a view to establishing a correlation between dermoscopic and histologic findings.
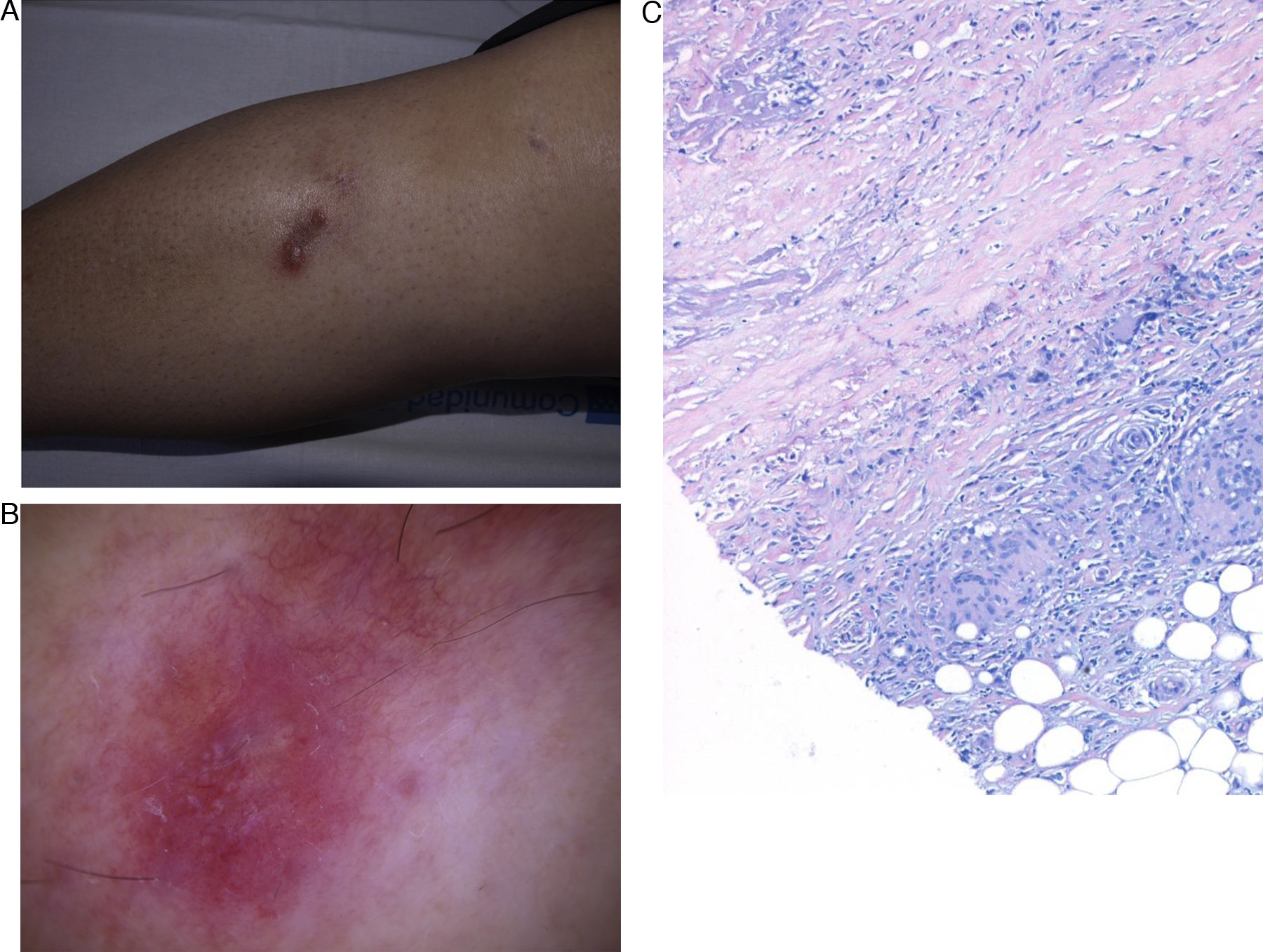
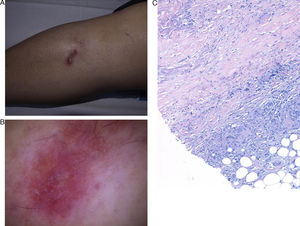
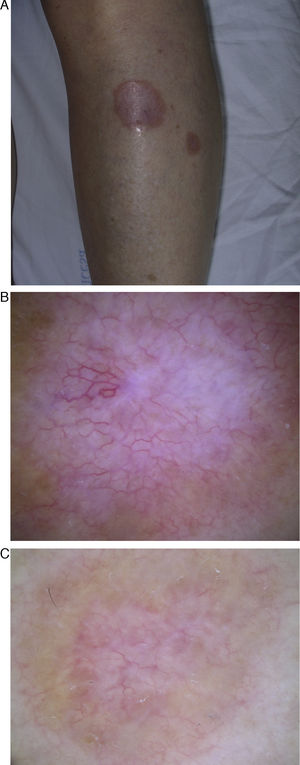
Patient 1 was a 65-year-old woman with no past history of interest who presented an asymptomatic erythematous-violaceous plaque on her right leg that had appeared 2 months earlier (Fig. 1A). Dermoscopy revealed comma-shaped vessels, whitish structures on a pink background, orange-brown areas, and a fine network of vessels in the upper part of the dermoscopic image (Fig. 1B). Biopsy results were consistent with a diagnosis of NL (Fig. 1C).
A, Well-defined, erythematous-violaceous plaque 2 cm in diameter on the right pretibial region. B, Comma-shaped vessels, whitish structures on a pink background, brownish-orange patches, and a fine network of vessels in the upper part of the dermoscopic image. C, Histology reveals alternating layers of palisading granuloma and degenerated collagen in the dermis together with an intense perivascular inflammatory infiltrate (hematoxylin-eosin ×100).
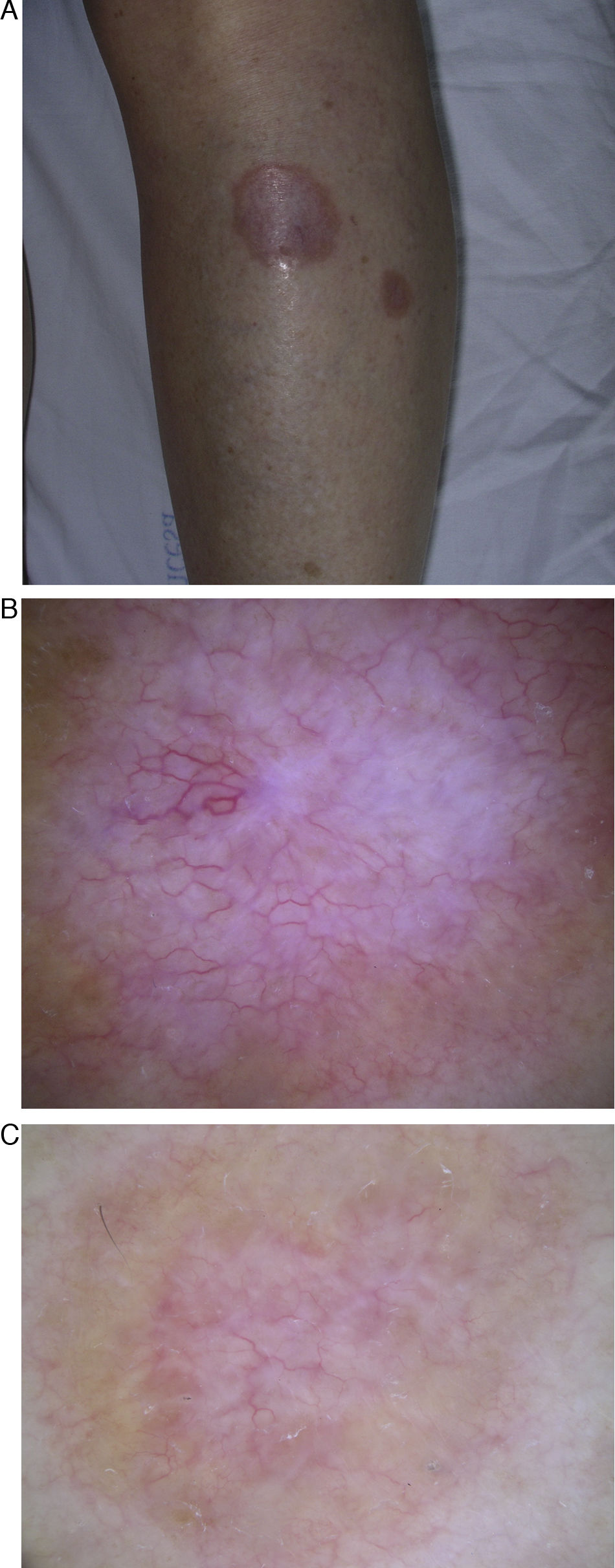
Patient 2 was a 38-year-old woman who presented 2 erythematous plaques on the left pretibial region; the larger lesion had appeared 1 year earlier and the smaller lesion 1 month before the consultation (Fig. 2A). Dermoscopically, both lesions were characterized by a fine network of abundant vessels on a pink background and homogeneous orange-yellow areas (Fig. 2, B and C). A biopsy of the larger lesion revealed the layered pattern of palisaded granuloma and necrobiosis typical of NL.
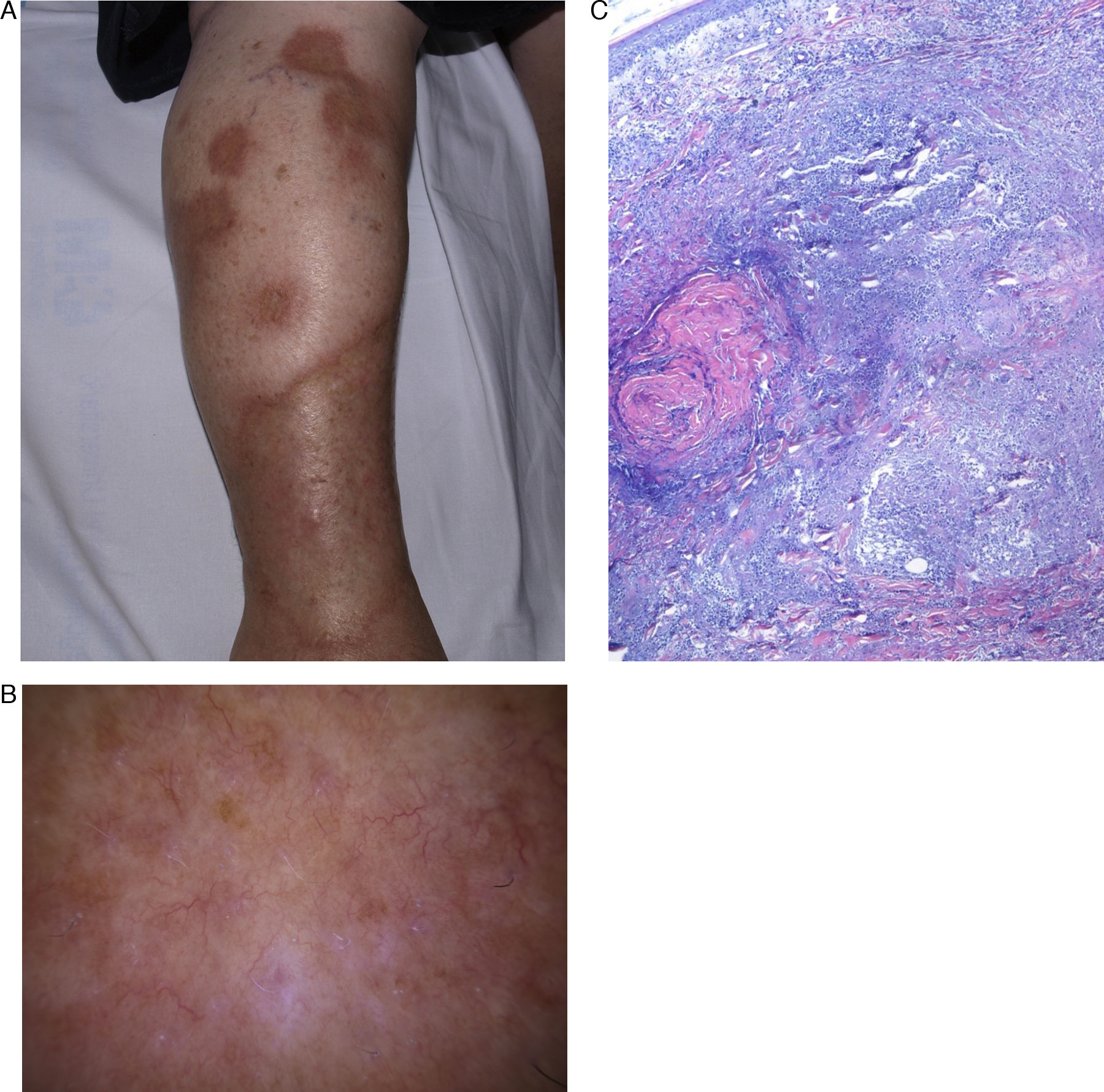
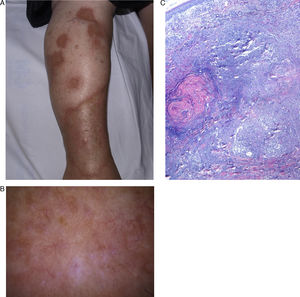
Patient 3 was a 61-year-old woman who presented numerous atrophic plaques with onset more than 15 years earlier (Fig. 3A). Dermoscopy revealed irregular arborizing vessels on a light-brown background, whitish areas, and a patchy pigmented reticulum (Fig. 3B). The findings of histology were consistent with a diagnosis of NL (Fig. 3C).
A, Yellowish atrophic plaques with raised and irregular erythematous borders on the right leg. B, Dermoscopy reveals irregular arborizing vessels on a light-brown background, whitish structures, and a patchy pigmented reticulum. C. Histology reveals abundant degenerated collagen in the dermis surrounded by palisading granulomas (hematoxylin-eosin ×40).
NL is a granulomatous disease with a characteristic clinical presentation and histologic features. However, the clinical expression may vary depending on the stage and site of the lesions. The initial clinical presentation consists of a well-defined reddish papule that extends peripherally to become an atrophic yellow-brown plaque with a raised erythematous border and telangiectasias. The site most often affected is the pretibial region, but NL can also develop on the trunk or upper limbs, or in atypical sites.1,2
The characteristic histologic finding is alternating horizontal layers of palisading granuloma and degenerated collagen affecting the full thickness of the dermis.3 The inflammatory infiltrate varies depending on the stage of development of the lesion. Initially, neutrophil infiltration is characteristic, but this diminishes when the plaques become atrophic to leave only small granulomas with multinucleated cells interspersed through the degenerated collagen.2
The differential diagnosis should include diabetic dermopathy, stasis dermatitis, erythema nodosum, and tuberculoid leprosy, among others. However, in the early stages, NL can also resemble sarcoid lesions. For example, it may present superficial annular lesions similar to those of granuloma annulare. NL lesions with marked fatty infiltration can mimic xanthomas.1
Dermoscopy can be very useful in the diagnosis of early-stage lesions and lesions located in atypical sites.4,5 There are very few descriptions of the dermoscopic features of NL in the literature. Vazquez-Lopez et al.,6 who assessed the vascular features of several nonneoplastic skin diseases dermoscopically, reported that the presence of linear vessels was the only common feature in 6 cases of NL. On the basis of 2 cases studied in the early stages, Bakos et al.5 proposed the presence of arborizing telangiectasias, hairpin vessels, and a yellowish background as features suggestive of NL, and suggested that these findings corresponded to the vascular plexus of the reticular dermis, papillary vessels, and necrobiosis, respectively. In our descriptive study, we present 3 cases with lesions in different stages of development ranging from months to years. Under dermoscopy, incipient lesions displayed comma-shaped vessels, more developed lesions revealed a fine network of vessels, and advanced lesions presented an irregular pattern of arborizing vessels. These findings could be explained by the visualization initially of the papillary vessels and later, as atrophy progresses, the increasing visibility of the vessels of the deep plexus.
The whitish structures observed would correspond to degenerated collagen and the orange patches to granulomatous inflammatory infiltrate. The pigmented reticulum and brown background observed in advanced lesions would appear to be due to the stimulation of melanocytes at the dermoepidermal junction, a common phenomenon in inflammatory lesions.
The dermoscopic description of other granulomatous diseases can be found in the literature. Lupus vulgaris has been described as a yellow-gold coloration with fine telangiectasias,7 and sarcoidosis is associated with translucent globular orange structures and linear vessels.8
Dermoscopy could become a very useful aid to the diagnosis of early-stage NL or NL lesions in atypical sites. Descriptive series with more cases are needed to confirm the findings on the dermoscopic features of NL presented in this paper.
Please cite this article as: Conde-Montero E, et al. Dermatoscopia de la necrobiosis lipoídica. Actas Dermosifiliogr. 2013;104:534-7.