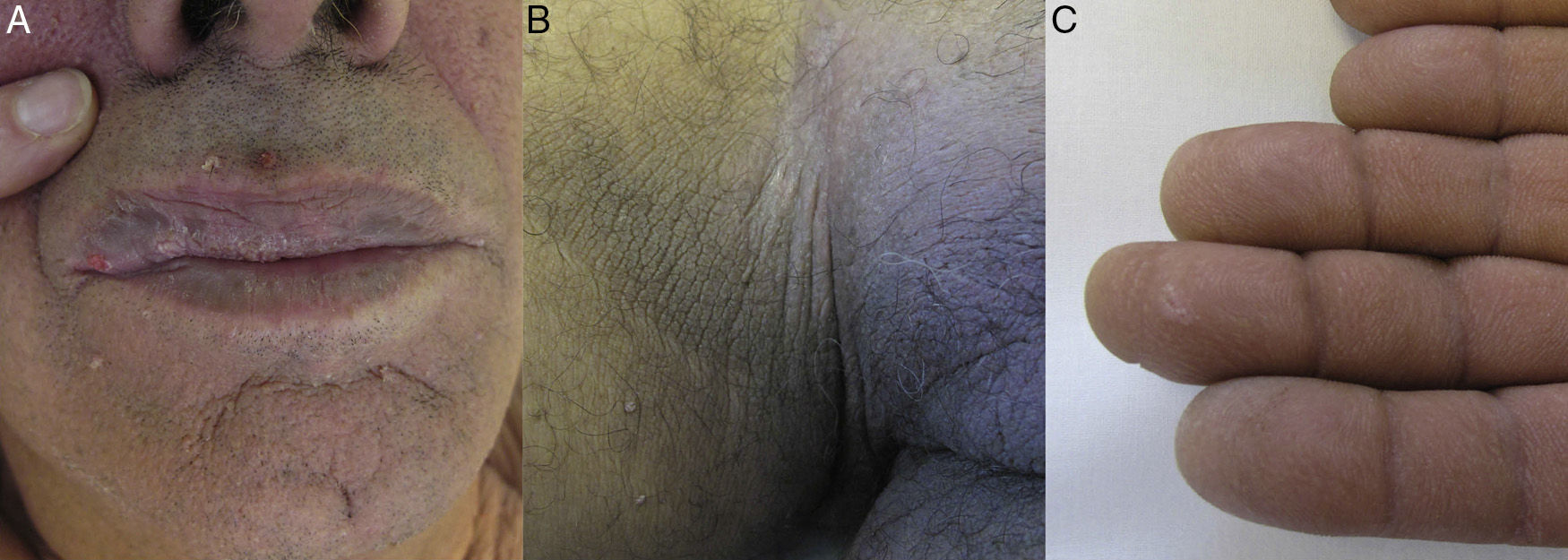
We describe the case of a 67-year-old man with a clinical history of smoking, hypertension, and hyperhomocysteinemia. The patient was referred for verrucous lesions on the face that had appeared more than 1 month earlier. A dermatological examination revealed several small, hyperkeratotic lesions on the cheeks and around the mouth (Figure 1A), as well as brownish plaques in the axillary and inguinal folds (Figure 1B). Both hands showed marked accentuation of the dermatoglyphics (Figure 1C). The patient reported that these symptoms had appeared abruptly within a period of less than 2 months. Based on clinical suspicion of a paraneoplastic dermatosis, additional tests were requested to identify the primary tumor.
Analyses revealed a cholestatic pattern with elevated levels of alkaline phosphatase and γ-glutamyl transpeptidase. Tumor marker analysis revealed only a slight increase of α-fetoprotein levels.
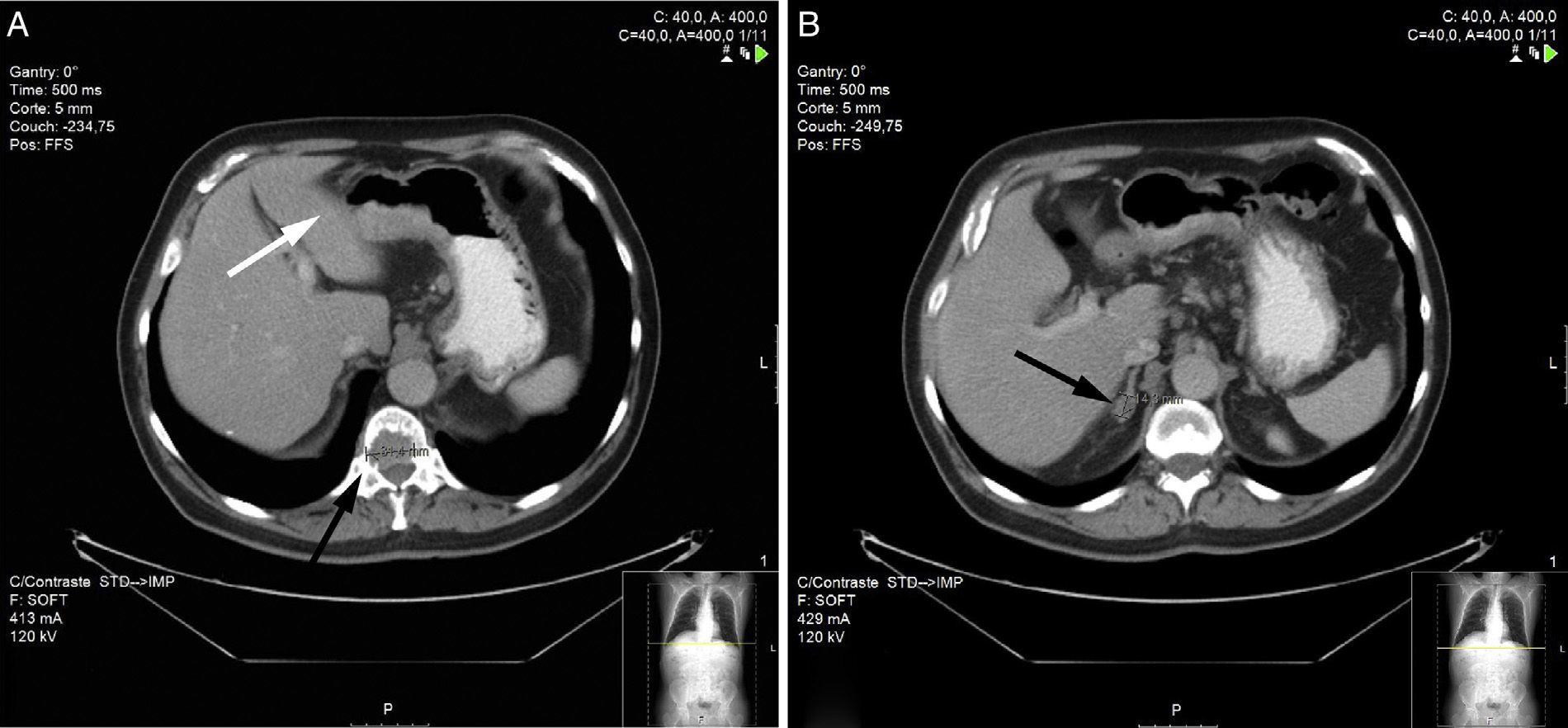
A thoracoabdominopelvic computed tomography scan revealed a lytic lesion in the posterior third of the T12 vertebral body, with slight invasion of the medullary canal, minimal thickening of the antral wall (Figure 2A), and swelling of the periaortic lymph nodes and gastrohepatic ligament lymph nodes (Figure 2B). An upper endoscopy revealed a malignant-looking ulcerated lesion with irregular borders in the area of the gastric incisura, extending towards the gastric body. Biopsy of the lesion was compatible with poorly differentiated gastric adenocarcinoma.
After treatment with palliative chemotherapy, the patient's basal state worsened and the neoplastic disease progressed with the appearance of multiple pulmonary nodules. One year after diagnosis the patient died following a respiratory infection.
More than 50 types of cutaneous paraneoplastic manifestations have been described, including malignant acanthosis nigricans (MAN), florid cutaneous and mucosal papillomatosis, and acquired pachydermatoglyphia.1
MAN is characterized by the presence of brownish, symmetric, nonpruritic plaques in the skin folds and on the back of the neck that can infiltrate and present as hyperkeratotic plaques. In contrast to the benign form of acanthosis nigricans, the paraneoplastic form is characterized by abrupt onset, rapid progression, and involvement of a large skin surface area. There is a strong correlation between MAN and intra-abdominal tumors, particularly tumors of gastric origin.2
Florid cutaneous and mucosal papillomatosis is characterized by the rapid appearance of verrucous papules on the trunk and extremities. The oral or genital mucosa may also be affected. This condition is most strongly correlated with tumors of gastric origin, in particular adenocarcinoma. While these lesions are clinically indistinguishable from viral warts, histologic analysis reveals marked hyperkeratosis with irregular acanthosis and papillomatosis, and no evidence of human papillomavirus infection.3,4
Tripe palms is characterized by the enhancement of the epidermal ridges of the palms, which become slightly thickened and acquire a velvety texture, resembling the intestinal villi. In 90% to 95% of cases this condition is associated with the presence of a solid tumor.
Tripe palms has been associated with many types of cancer, the most common of which are those of the gastrointestinal tract (30%) and lungs (20%).5,6
The presence of all 3 of these paraneoplastic dermatoses (MAN, florid cutaneous and mucosal papillomatosis, and tripe palms) in the same patient has been previously described in the literature, suggesting potentially common etiological and pathogenic mechanisms. In fact, both tripe palms and florid cutaneous and mucosal papillomatosis are considered by some authors as clinical variants of MAN. Several studies suggest that epidermal growth factor alpha is secreted by the tumor and transported in the blood to the skin surface, where it stimulates the development of keratinocytes by activating tyrosine kinase receptors, which promote widespread mitotic and antiapoptotic cellular activity.7–10
Of particular interest in the present case is the association of several distinct paraneoplastic cutaneous manifestations in the same patient. Recognition and identification of these conditions can enable early diagnosis and treatment of associated neoplasms, in some cases resulting in a better long-term prognosis for the patient.
Please cite this article as: Vilas-Sueiro A, Suárez-Amor Ó, Monteagudo B, de las Heras C. Acantosis nigricans maligna, papilomatosis cutáneo-mucosa florida y paquidermatoglifia adquirida en paciente con adenocarcinoma gástrico. Actas Dermosifiliogr. 2015;106:438–439.