Cutaneous metastases from hepatocellular carcinoma are very uncommon, and, according to one series, account for just 0.8% of all cutaneous metastases.1 Iatrogenic factors appear to be the most common cause and include needle tract seeding during percutaneous interventional procedures and surface seeding of tumor cells during surgery.2
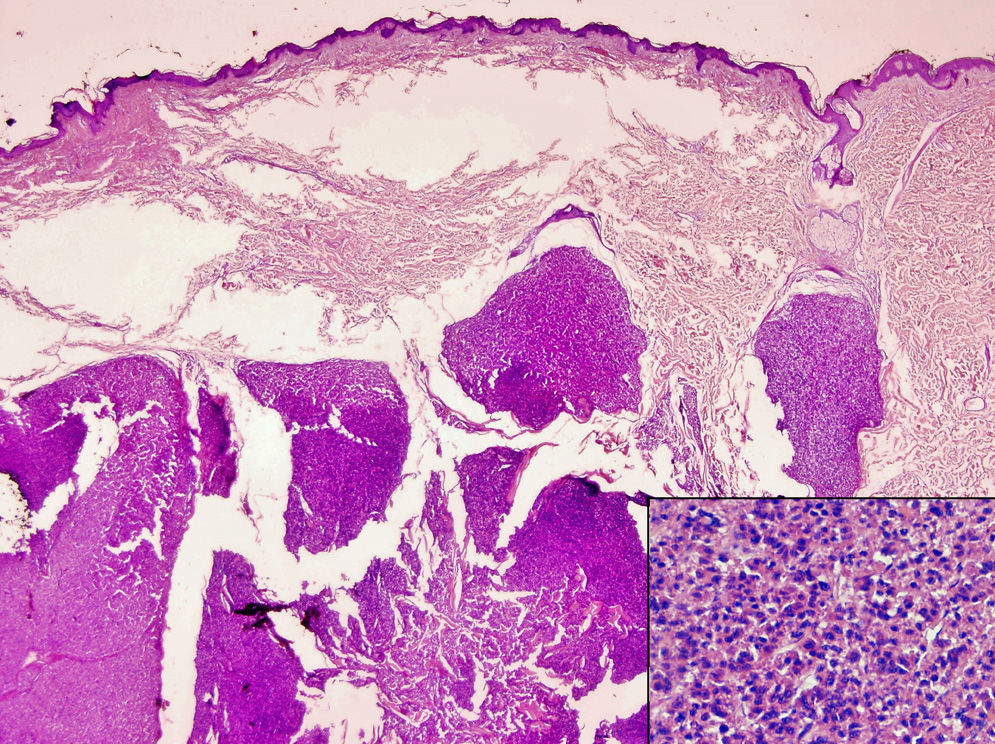
We present the case of a 35-year-old man with a history of chronic hepatitis C virus infection with progression to cirrhosis. He was subsequently diagnosed with hepatocellular carcinoma, which was treated with concomitant radiofrequency ablation and percutaneous ethanol injections. A year after treatment, the patient presented with a subcutaneous nodule in the right costal region (Figure 1). The site of the lesion appeared to coincide with that of the radiofrequency needle tract. Computed tomography showed a large lesion consistent with progression of the hepatocellular carcinoma on the right abdominal wall, in addition to multiple intrahepatic metastatic masses (Figure 2). Skin biopsy confirmed that the cutaneous lesion was a metastasis from the hepatocellular carcinoma (Figure 3). Surgical treatment and chemoembolization were ruled out because of the size of the lesion. The patient was administered chemotherapy (sorafenib) and radiation therapy in the scar area, but died 5 months after diagnosis of the cutaneous metastasis.
Percutaneous interventional procedures have a very important role in the management of hepatocellular carcinoma and are widely used in this setting.3,4 The main procedures are fine-needle aspiration biopsy, percutaneous ethanol injections, and radiofrequency ablation.3,4 These procedures are generally considered to be safe, and while various complications have been described, they are uncommon, can mostly be managed conservatively, and are associated with low mortality.3,4
Needle tract seeding in hepatocellular carcinoma is an exception. While very rare, it can occur throughout follow-up and alters prognosis.4 Needle-tract implantations generally appear as a single or few round or oval nodules along the tract of the needle, which extends from the intraperitoneal region to the skin or subcutaneous tissues through the abdominal or intercostal muscles.4
The overall incidence of tumor seeding (considering all techniques) ranges from 0.5% to 1%, with rates varying slightly according to the technique used.4 In most studies, the reported incidence is less than 2%.5
Several hypotheses have been proposed to explain how tumor cells are disseminated along the needle tract.4 The first is that viable tumor cells adhere to the needle and break off as this is being removed. The second is that tumor cells might be carried to the surface of the skin during the reflux of blood or other fluids up the needle tract, and the third is that tumor cells might enter the tract due to a sudden increase in intratumoral pressure, as commonly occurs during radiofrequency ablation.4
A conservative approach is taken in most cases, as many patients are already in the terminal stages of their disease when the metastases are detected. Surgical excision, however, is sometimes performed. When this is not possible, because of advanced disease, low performance status, or other reasons, radiation therapy appears to be a reasonable alternative.2
In conclusion, needle tract seeding in percutaneous interventional procedures are very rare, but are the most common cause of cutaneous metastases from hepatocellular carcinoma.
Please cite this article as: de León FJ, Blanes MM, Albares MP, Berbegal L. Metástasis cutánea de hepatocarcinoma tras procedimientos percutáneos. Actas Dermosifiliogr. 2015;106:440–441.