Solar urticaria is an uncommon photodermatosis. First-line treatment is with antihistamines; second-line treatment includes induction of light tolerance using UV phototherapy.
ObjectivesWe aimed to describe and evaluate the effectiveness of a desensitization protocol with narrowband UV-B in patients with solar urticaria.
Material and methodsWe performed a retrospective study of patients with solar urticaria with an action spectrum in the UV-A range, the visible light range, or both who had received therapy with narrowband UV-B for induction of light tolerance. Short courses of treatment were administered (<20 sessions, 3 per week) during spring. The initial dose was determined according to the skin type. The Skindex-29 was administered before treatment and after summer; a nonvalidated questionnaire was also administered after summer to evaluate disease activity and satisfaction with treatment.
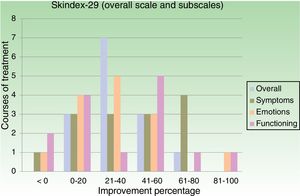
ResultsWe included 8 patients with an action spectrum (4 with visible light and 4 with UVA plus visible light). Seventeen courses (1-6 per patient) were administered per year. The number of sessions per year ranged from 11 to 20. The mean dose of narrowband UV-B per course was 7.45J/cm2. No patients experienced flares or adverse effects during treatment. The response was satisfactory in 6 patients. The improvement in the overall Skindex-29 score was greater than 20% in 78.6% of cases. The improvement in the function and symptoms subscales was over 20% in 71% and 64% of cases, respectively.
ConclusionInduction of light tolerance with narrowband UV-B in solar urticaria is safe and effective in a high percentage of patients.
La urticaria solar (US) es una fotodermatosis infrecuente. Los antihistamínicos constituyen la primera línea de tratamiento, incluyéndose en segunda línea la inducción de fototolerancia mediante fototerapia con ultravioleta.
ObjetivosDescribir y evaluar la eficacia de un protocolo de desensibilización, con UVB de banda estrecha (UVB-BE) en pacientes con US.
Material y métodosEstudio retrospectivo de pacientes diagnosticados de US con espectro de acción en UVA, luz visible (LV) o ambas, que habían realizado fototerapia con UVB-BE para inducir fototolerancia. Se realizan cursos cortos (menos de 20 sesiones, 3 por semana) durante la primavera, con dosis inicial determinada por el fototipo. Se recogen resultados del Skindex-29 antes del tratamiento y después del verano, y un cuestionario no validado de efectividad terapéutica después del verano para valorar actividad de la enfermedad y grado de satisfacción.
ResultadosSe incluyen 8 pacientes con espectro de acción: 50% LV y 50% UVA más luz visible. Se realizaron 17 cursos anuales (1-6 cursos por paciente), de 11 a 20 sesiones. La dosis media de UVB-BE por curso fue 7,45J/cm2. Ningún paciente presentó brotes o efectos adversos durante el tratamiento. La respuesta fue satisfactoria en 6 pacientes. En el 78,6% de los tratamientos la mejoría en el Skindex-29 global fue superior al 20%. La mejoría en las subescalas sintomática y funcional fue superior al 20% en el 71% y el 64% respectivamente.
ConclusiónLa inducción de fototolerancia con UVB-BE en la US es un procedimiento seguro y efectivo en un elevado porcentaje de pacientes.
Solar urticaria (SU) is an uncommon idiopathic photodermatosis, accounting for 7% of all photodermatoses, and is classified as a chronic inducible (physical) urticaria, accounting for between 0.08% and 0.4% of all urticarias.1 Clinically, it is characterized by pruritus, erythema, or wheals in sun-exposed areas, generally appearing within an hour of exposure to sunlight or artificial light.2 Symptoms are triggered by exposure to certain action spectra, most commonly visible light only (31%-57%) or UV-A and visible light (7%-42%). The action spectrum involved can be determined by photobiologic testing.3 First-line treatment is with antihistamines; most consensus statements include phototherapy as a second- or third-line treatment, primarily on the basis of isolated case reports or small series of fewer than 5 patients, most of which describe induction of light tolerance using UV-A or psoralen–UV-A (PUVA) phototherapy.4–10 The aim of this study was to describe and evaluate the effectiveness and safety of a short desensitization protocol with narrowband UV-B in patients with SU.
Materials and MethodsThis was a single-center retrospective study with the following inclusion criteria for patients: (1) age >18 years; (2) SU was diagnosed between 2012 and 2017; (3) SU was diagnosed in the photobiology unit of our hospital; (4) the action spectrum involved was visible light, UV-A, or visible light and UV-A; and (5) the patient had not responded to treatment with H1 antihistamines or heliotherapy and had undergone phototherapy with narrowband UV-B to induce light tolerance. The exclusion criteria were as follows: (1) association of other photodermatoses; and (2) the use of photosensitizing drugs.
Diagnosis was established on the basis of clinical history and a complete photobiologic study carried out using a solar simulator (Solar Light Company, Philadelphia, United States), Gigatest continuous-spectrum UV-B and UV-A lamps (Medisun, Brühl, Germany), and a slide-projector lamp (Kodak AG, Stuttgart, Germany). Phototest results were read at 10, 30, and 60minutes, with a final reading at 24hours.
The following clinical data were collected: age, sex, skin phototype, time since onset, activities associated with flares, and action spectra identified in the photobiologic study. Blood tests for autoimmune disorders (antinuclear antibodies, including anti-Ro) were carried out.
For narrowband UV-B phototherapy, we used a Medisun 2800 PC 44B cabin equipped with 44 TL01 lamps from 2007 and a Medisun 2800 Innovation cabin equipped with 20 TL01 lamps from 2011 (Medisun, Brühl, Germany). Short courses of treatment (10-20 phototherapy sessions, 3 per week) were administered in the second half of May. In accordance with our unit's usual protocol, the initial dose and subsequent increases (10%-20%) were established according to skin phototype and tolerance. After treatment with phototherapy, patients were asked to maintain sun exposure of up to 15-20minutes per day between the hours of 12:00 PM and 4:30 PM throughout the summer months. Annual courses of treatment were administered in accordance with the dermatologist's clinical judgment and the disease progression in each patient. All patients gave informed consent prior to each course of treatment.
In order to assess the response to each course of treatment, the patients completed Skindex-29,11 a questionnaire on health-related quality of life, both before and after the summer. This questionnaire consists of 29 questions and gives a score on a scale of 0 to 100, where 100 represents the maximum impact on quality of life. In addition to an overall score, the questionnaire provides scores on 3 subscales: symptoms, emotions, and functioning. We also designed our own nonvalidated questionnaire on treatment effectiveness and patient satisfaction, which patients completed after the summer. This questionnaire consisted of the following questions and answers (with scores shown in parentheses): Did you have multiple episodes of disease during the summer? Yes (1), no (0). How many episodes did you have? 0 (0), 1-5 (1), 6-10 (2), 11-15 (3), >15 (4). To what extent did you have to reduce your outdoor activity? Not at all (0), a little (1), somewhat (2), a lot (3). How would you rate the outcome of the treatment to prevent flares during the summer? Bad (2), good (1), very good (0). A final score was calculated on a scale of 0-10, where 0-3 indicates good control, 4-7 indicates moderate control, and >7 indicates poor control.
The baseline data for the statistical analysis were expressed as mean and range, and the Skindex-29 results were expressed as absolute figures and improvement percentages.
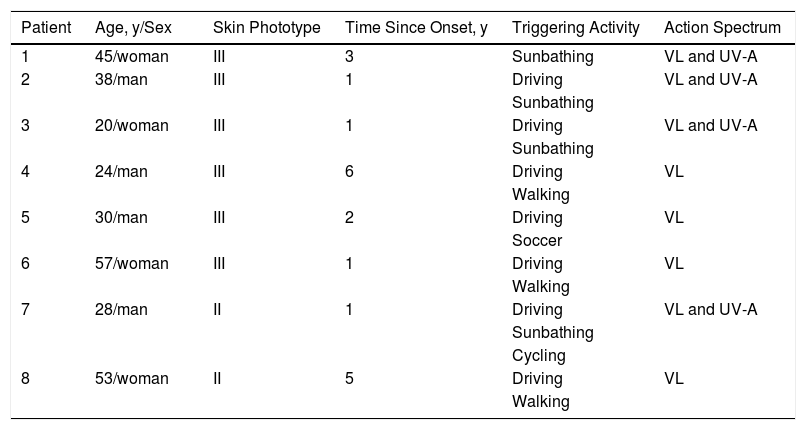
ResultsTable 1 shows the baseline patient data. Eight patients (4 men and 4 women) were included in the study. The mean age was 36.8 years (range, 20-57). Seventy-five percent of the patients had skin phototype iii and 25% had skin phototype ii. The mean time since onset was 2.5 years (range, 1-6). For 50% of the patients, the action spectrum involved was visible light; for the other 50%, it was UV-A plus visible light. Blood tests revealed no important alterations; results for autoimmune disorders were negative in all patients.
Baseline Data.
| Patient | Age, y/Sex | Skin Phototype | Time Since Onset, y | Triggering Activity | Action Spectrum |
|---|---|---|---|---|---|
| 1 | 45/woman | III | 3 | Sunbathing | VL and UV-A |
| 2 | 38/man | III | 1 | Driving | VL and UV-A |
| Sunbathing | |||||
| 3 | 20/woman | III | 1 | Driving | VL and UV-A |
| Sunbathing | |||||
| 4 | 24/man | III | 6 | Driving | VL |
| Walking | |||||
| 5 | 30/man | III | 2 | Driving | VL |
| Soccer | |||||
| 6 | 57/woman | III | 1 | Driving | VL |
| Walking | |||||
| 7 | 28/man | II | 1 | Driving | VL and UV-A |
| Sunbathing | |||||
| Cycling | |||||
| 8 | 53/woman | II | 5 | Driving | VL |
| Walking |
Abbreviation: VL, visible light.
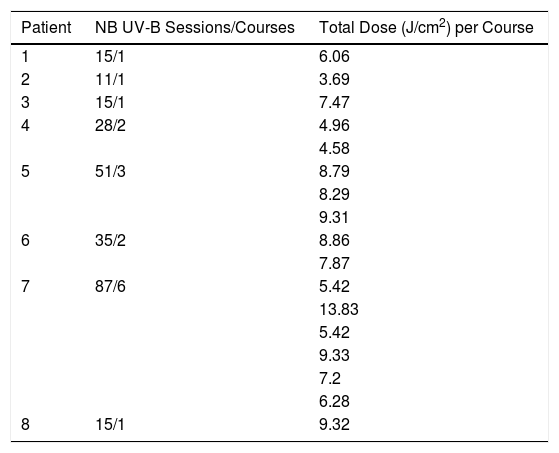
Seventeen courses (1-6 per patient) were administered per year. The number of sessions per year ranged from 11 to 20. The mean dose of narrowband UV-B per course was 7.45J/cm2 (range, 3.69-13.83). No patients experienced flares or adverse effects during phototherapy. After the treatment, all patients underwent progressive sun exposure throughout the summer months. The treatment data are shown in Table 2.
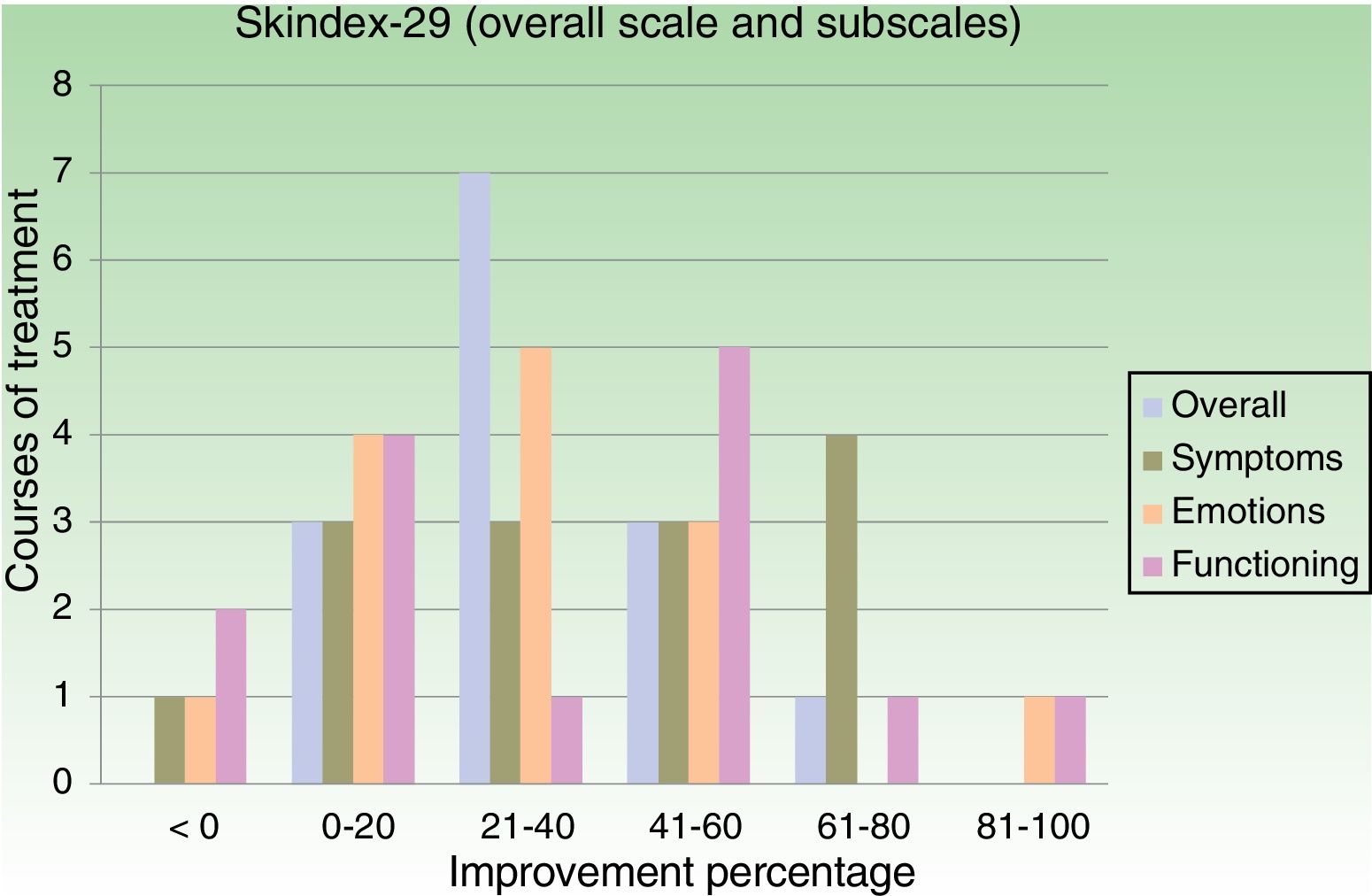
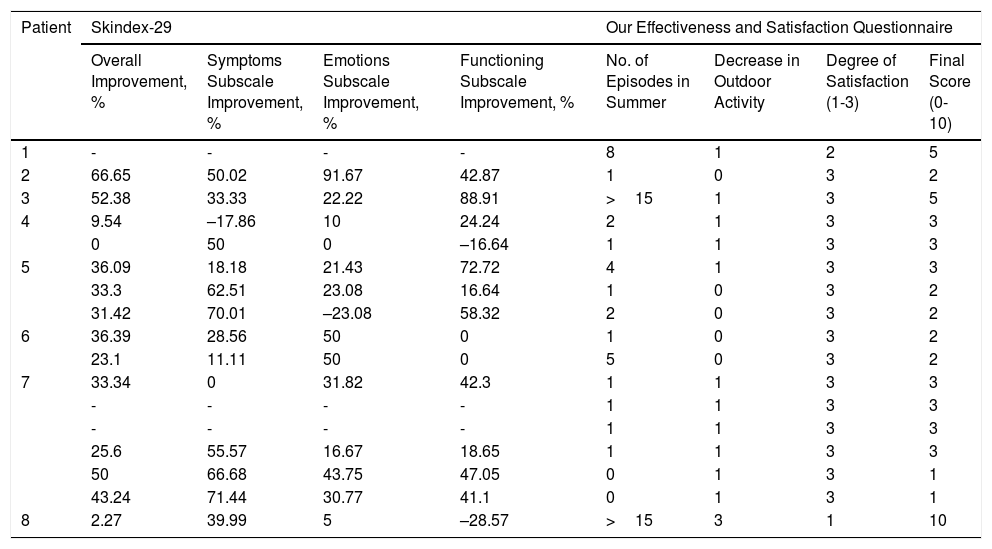
Table 3 shows the improvement results from the Skindex-29 and our own questionnaire. Skindex-29 results were obtained in 14 of 17 courses. On the overall Skindex-29 scale, improvement was >20% in 79% of courses and >40% in 28.6% of courses. On the symptoms subscale, improvement was >20% in 71% of courses and >40% in 50% of courses. On the emotions subscale, improvement was >20% in 64% of courses and >40% in 28.6% of courses. Finally, on the functioning subscale, improvement was >20% in 57% of courses and >40% in 50% of courses. Figure 1 shows how the improvement percentages break down according to number of courses.
Improvement per Course of Treatment According to Results from Skindex-29 and Our Effectiveness and Satisfaction Questionnaire.
| Patient | Skindex-29 | Our Effectiveness and Satisfaction Questionnaire | ||||||
|---|---|---|---|---|---|---|---|---|
| Overall Improvement, % | Symptoms Subscale Improvement, % | Emotions Subscale Improvement, % | Functioning Subscale Improvement, % | No. of Episodes in Summer | Decrease in Outdoor Activity | Degree of Satisfaction (1-3) | Final Score (0-10) | |
| 1 | - | - | - | - | 8 | 1 | 2 | 5 |
| 2 | 66.65 | 50.02 | 91.67 | 42.87 | 1 | 0 | 3 | 2 |
| 3 | 52.38 | 33.33 | 22.22 | 88.91 | >15 | 1 | 3 | 5 |
| 4 | 9.54 | –17.86 | 10 | 24.24 | 2 | 1 | 3 | 3 |
| 0 | 50 | 0 | –16.64 | 1 | 1 | 3 | 3 | |
| 5 | 36.09 | 18.18 | 21.43 | 72.72 | 4 | 1 | 3 | 3 |
| 33.3 | 62.51 | 23.08 | 16.64 | 1 | 0 | 3 | 2 | |
| 31.42 | 70.01 | –23.08 | 58.32 | 2 | 0 | 3 | 2 | |
| 6 | 36.39 | 28.56 | 50 | 0 | 1 | 0 | 3 | 2 |
| 23.1 | 11.11 | 50 | 0 | 5 | 0 | 3 | 2 | |
| 7 | 33.34 | 0 | 31.82 | 42.3 | 1 | 1 | 3 | 3 |
| - | - | - | - | 1 | 1 | 3 | 3 | |
| - | - | - | - | 1 | 1 | 3 | 3 | |
| 25.6 | 55.57 | 16.67 | 18.65 | 1 | 1 | 3 | 3 | |
| 50 | 66.68 | 43.75 | 47.05 | 0 | 1 | 3 | 1 | |
| 43.24 | 71.44 | 30.77 | 41.1 | 0 | 1 | 3 | 1 | |
| 8 | 2.27 | 39.99 | 5 | –28.57 | >15 | 3 | 1 | 10 |
Patients completed our own questionnaire on effectiveness and satisfaction after every course of treatment. Scores on our questionnaire were between 0 and 3 (good control) for 14 of 17 courses (82.3%). Scores indicated moderate control for 2 courses and poor control for 1 course.
During follow-up, a good response was seen in 6 patients: annual courses of desensitization treatment with narrowband UV-B were continued in 5 patients, but 1 patient was switched to induction of light tolerance with heliotherapy. The response was deemed insufficient in 2 patients; treatment was therefore initiated with omalizumab and a good response was observed. These patients scored between 5 and 10 on our questionnaire and neither had any clinical characteristics that distinguished them from the other patients.
DiscussionVarious studies have described the efficacy of UV-A in SU as an inducer of light tolerance in various action spectra.4,6,8 The current consensus statements also include narrowband UV-B phototherapy as an effective treatment for the induction of light tolerance in SU.2,4,5 Besides isolated case reports that have mentioned narrowband UV-B phototherapy in SU,7,9,13 this treatment has only been assessed in 1 study, which was published in 2012 and included 39 patients with SU.12 That study included 29 patients in whom the action spectrum was in the range of UV-A and/or visible light (similar to the present study). In that subgroup of patients, the initial treatment dose was adjusted to 50% of the minimal erythema dose. SU flares occurred during treatment in 31% of those patients and moderate treatment-induced erythema was seen in 86.2%.12 In our patients, however, no SU flares or adverse effects were observed during treatment. In the aforementioned study, response to treatment was assessed in terms of whether or not each patient had experienced 1 or more SU flares 1 month and 3 months after treatment. At 3 months, SU flares had been observed in 20.7% of patients. This percentage was attributed to a lack of daily sun exposure after treatment in these patients.12
Our study was the first to use health-related quality of life questionnaires to measure treatment response in SU. The Skindex-29 questionnaire allowed a more precise evaluation of the impact of SU on quality of life and the various subscales allowed a more specific assessment. We consider the symptoms and functioning subscales to be fundamental in the assessment of treatment response because these factors have the largest impact on patients’ everyday activities. In half of all courses of treatment, an improvement of >40% was observed for both of these subscales. The results on the functioning subscale were particularly evocative in 2 patients whose regular activities required sustained sun exposure (a professional cyclist and professional soccer player). These results are echoed in the results from our own questionnaire, in which the highest possible score for satisfaction with treatment was given in 15 of 17 courses.
Various hypotheses have been proposed regarding the mechanism of action involved in the induction of light tolerance with UV-B in patients whose symptoms are reproduced under other action spectra, including thickening of the stratum corneum, epidermal hyperplasia, and increased melanin production, in all cases avoiding the action spectrum responsible for the condition. Another possible factor is the secondary immunomodulatory effect of UV-B.14,15
In conclusion, based on our findings, we believe that the induction of light tolerance with short courses of narrowband UV-B phototherapy is a safe and effective procedure in patients with SU caused by visible light and/or UV-A. We believe that a specific validated questionnaire is needed in order to assess response to this treatment.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Chicharro P, Rodríguez-Jiménez P, Capusan TM, Herrero-Moyano M, de Argila D. Inducción de fototolerancia con ultravioleta B de banda estrecha en urticaria solar. Actas Dermosifiliogr. 2018;109:888–892.