The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) has some shortcomings when it comes to coding certain dermatological disorders. To overcome these shortcomings, a compatible version of the ICD-10 specifically adapted to dermatology was produced in Spain in 1999. The recent DIADERM study recorded 10 999 dermatological diagnoses using a representative sample of dermatologists working at outpatient clinics in Spain. The aims of the current study were to identify diagnoses from the DIADERM study that could not be coded using the adapted ICD-10, determine why, and check if they could be coded using the draft ICD-11.
Material and methodsWe included all dermatological diagnoses from the DIADERM study that could not be assigned a code from the adapted ICD-10. We then quantified and recorded all the diagnoses that could not be coded using either the adapted ICD-10 or the draft ICD-11.
ResultsOf the 10 999 diagnoses analyzed, 41 had not been assigned a code. Of these, 19 were assigned an adapted ICD-10 code on reassessment. However, the adapted ICD-10 and the draft ICD-11 lacked specific codes for 22 and 17 diagnoses, respectively.
ConclusionsThe adapted ICD-10 can be used to correctly code the vast majority of dermatological diagnoses seen in routine clinical practice. Nevertheless, the system does have some minor shortcomings when it comes to coding certain diseases, particularly newly discovered and emerging diseases. Some of these problems, however, were resolved with the new ICD-11. Based on our findings, we propose some modifications to the ICD-11.
La codificación de la enfermedad dermatológica en la 10.ª edición de la Clasificación Internacional de Enfermedades (CIE-10) presenta algunas carencias, motivo por el cual en 1999 se desarrolló una adaptación para Dermatología. En el estudio DIADERM se recogieron 10.999 diagnósticos de consulta ambulatoria realizados por dermatólogos a través de una muestra representativa nacional en España. El objetivo del presente trabajo es analizar los diagnósticos de DIADERM en los que no fue posible asignar un código diagnóstico con la CIE-10 adaptada, encontrar las causas y comprobar si la nueva CIE-11, en fase de borrador, permite codificar el diagnóstico.
Material y métodosSe incluyeron todos los diagnósticos dermatológicos de DIADERM en los que no se pudo asignar un código diagnóstico con la CIE-10 adaptada. Se cuantificaron y se recogieron los diagnósticos incluidos para los que la CIE-10 adaptada y el borrador de la CIE-11 carecen de códigos específicos.
ResultadosA partir de un total de 10.999 diagnósticos del estudio DIADERM, se incluyeron 41 diagnósticos dermatológicos que no tenían código asignado, de los que, tras ser revaluados, 19 pudieron ser codificados, pero en 22 y en 17 diagnósticos, la CIE-10 adaptada y la CIE-11 provisional carecían de código específico, respectivamente.
ConclusionesLa CIE-10 adaptada a Dermatología contiene códigos diagnósticos que permiten clasificar adecuadamente a la inmensa mayoría de los diagnósticos dermatológicos vistos en consulta habitual. No obstante, presenta pequeñas carencias a la hora de clasificar ciertas enfermedades dermatológicas, sobre todo las de descubrimiento o desarrollo más reciente; algunos de estos problemas han sido resueltos en la nueva CIE-11. Con base en los resultados, se proponen algunas modificaciones para la CIE-11.
Patient diagnoses must be classified according to definitions that are consistent across countries and over time if health records are to be used for research in epidemiology or the management of health care systems. Consistency is provided by applying diagnostic coding systems, the most widely used of which is the one maintained by the World Health Organization (WHO): the International Classification of Diseases, currently in its 10th revision (the ICD-10).1 This revision of the ICD was completed in 1992 and its latest version was published in 2016. The ICD-10 is a simple alphanumeric coding system that facilitates diagnostic classification for both clinical and epidemiologic purposes. It provides the data for computing mortality and morbidity rates in countries belonging to the WHO, and some countries use it to allocate health care resources.2
Certain ICD-10 codes have been reported to be imprecise.3 Recent studies have found deficiencies in the classification of allergic conditions2,4: as a result, events such as anaphylaxis are rendered less visible by underreporting, data collection is compromised, and statistical analyses are less precise, possibly leading to underfunding. A new revision —the ICD-11 —is currently being developed with the aim of solving some of these problems.1
An additional concern is that the ICD-10 coding of dermatologic diseases includes areas of difficulty and imprecision, the reason why an adaptation for this specialty was developed in Spain in 1999.5 The adapted version was developed to complement, not replace, the general ICD.
The literature on the shortcomings of the ICD-10 is scant, and an analysis of the reasons for coding problems in dermatology could provide useful information and point toward modifications that could be incorporated into the draft ICD-11. Such an analysis could also provide verification that the drafted revisions are going in the right direction.
The recent DIADERM study included nearly 11000 diagnoses representative of routine clinical practice in outpatient dermatology clinics in Spain.6 Data for 8832 patients were contributed by a stratified random sample of 80 Spanish dermatologists. Diagnoses were collected on 3 consecutive days in January and 3 consecutive days in May, and the diagnoses were coded by a dermatologist familiar with the ICD-10 adapted for dermatology.5 The present study aims to identify all the cases in the DIADERM database that were not assigned a code, analyze the reasons for difficulty, identify problems that could be eliminated through revision, and determine whether the draft ICD-11 has improved classification by correcting the shortcomings of the ICD-10.
Material and MethodsStudy Design and Data SamplingThe reference population for this cross-sectional descriptive study consisted of patients who came to a dermatology outpatient clinic in Spain. The data were collected for the DIADERM study,6 in which 10 999 diagnoses were recorded for 8832 patients who consulted 80 randomly selected Spanish dermatologists. The sample was stratified by location. Data were collected on 3 consecutive days in January and May. The unit of analysis was the diagnosis.
We recorded only diagnoses for this study, excluding information on procedures. One dermatologist (A.M.L.) then coded the diagnoses according to the Spanish ICD-10 adaptated for dermatology.5 If no code was found in that system, the Spanish electronic edition of the ICD-107 was consulted. If no code consistent with the physician's description was found, the case was marked as noncodifiable and a brief description of the problem was noted. All doubtful coding and diagnoses for which no code was found were reviewed by 3 dermatologists (I.G.D., R.T., and Y.G.) before it was decided that they definitely could not be coded.6 The 3 dermatologists also reviewed a random sample of codes.
Inclusion and Exclusion CriteriaDiagnoses for which no ICD-10 code had been found previously were included for analysis. Diagnoses that caused coding problems were also included. We excluded diagnoses if they corresponded to nondermatologic diseases, were illegible, or included unclear comments. The dermatologists who were the sources of the entries were anonymous, so we were unable to ask them to review the excluded records.
Study Variables and Statistical AnalysisOne dermatologist (G.G.L.) reviewed the included diagnoses. The reasons why a diagnosis could not be coded in the Spanish dermatology adaptation of the ICD-105 were analyzed and classified in the following categories: 1) diseases not specifically present in the classification and not falling under any of the available codes, 2) diseases not listed in the adapted ICD-10 but which could be placed in a higher-level category, or 3) diseases listed in the adapted ICD-10 that had erroneously been considered noncodifiable previously.
The included diagnoses were then classified according to the draft ICD-11 codes, which are available for access on the internet.8
If diagnoses could not be classified according to either the ICD-10 or the draft ICD-11 systems, we consulted their indexes. Certain diagnoses do not have individual codes assigned, but they figure in the alphabetical index, where the entry indicates the higher-level code under which they fall.
Descriptive statistics in the form of absolute frequencies and percentages were compiled for the diagnoses and corresponding ICD-10 or ICD-11 codes. We used Stata Statistical Software, release 14 (StataCorp, LP; College Station, Texas, USA). The DIADERM study6 was approved by the clinical research ethics committee of the province of Granada, Spain.
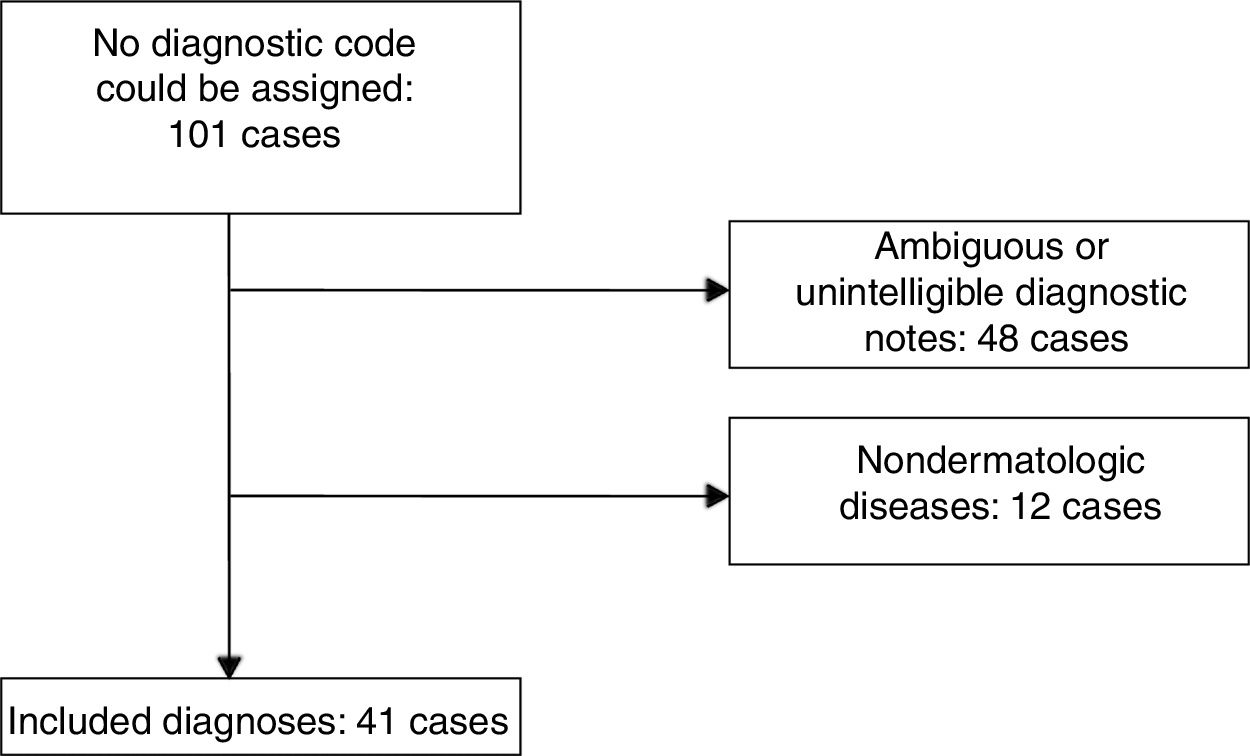
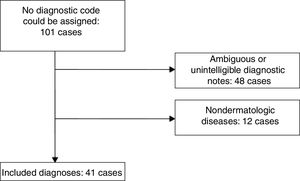
ResultsWe found 101 cases with diagnoses that had not been assigned a code. After excluding unintelligible or unclear notes and nondermatologic diseases, there remained 41 dermatology cases to analyze (Fig. 1).
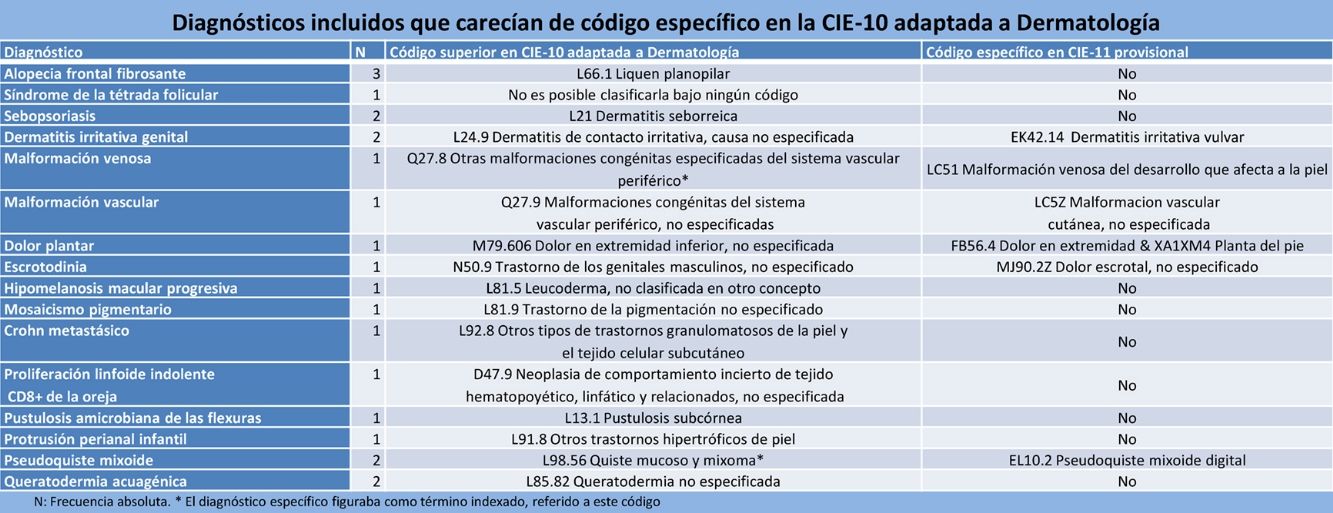
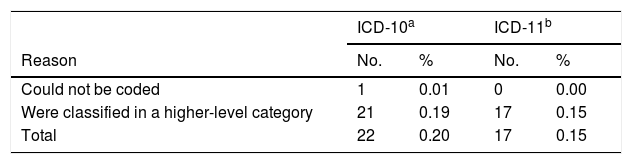
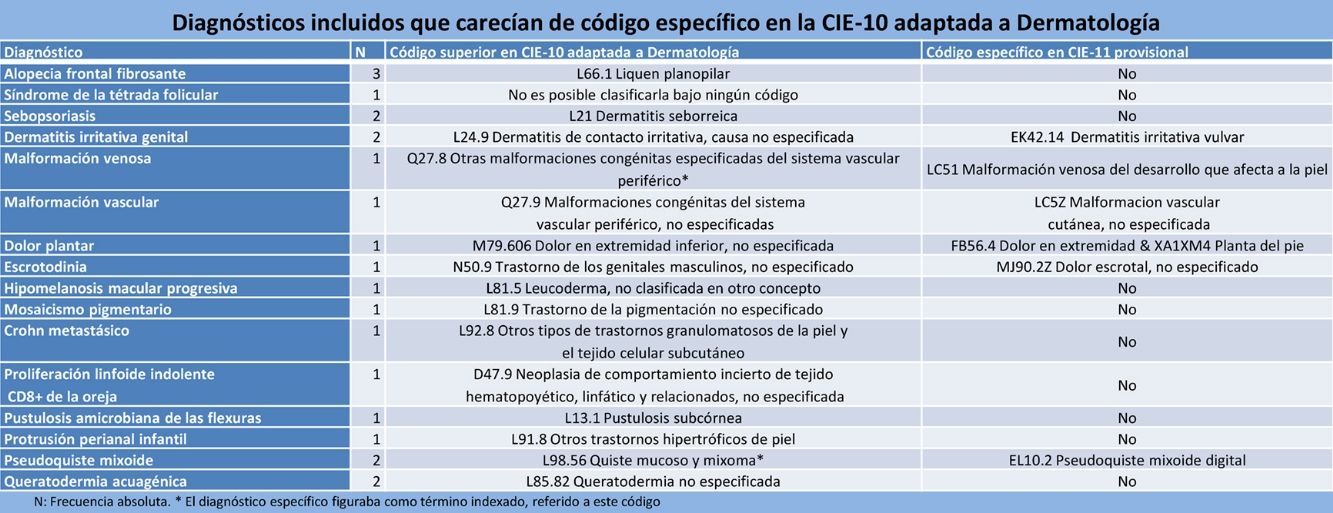
Coding With the ICD-10 Adapted for Dermatology5We were able to assign specific codes in 19 of the 41 cases when we used the ICD-10 adapted for dermatology,5 leaving only 22 cases with diagnoses that were still uncoded. Those 22 cases (Table 1) represented 0.20% of all diagnoses in the DIADERM database.6 Sixteen different diagnoses were represented. All but one of them (follicular occlusion syndrome, or the follicular occlusion tetrad) could be grouped under the next highest category (Table 2a).
Dermatologic Diagnoses Not Classified With the ICD-10 Adapted for Spanish Dermatology or the Draft ICD-11.
| ICD-10a | ICD-11b | |||
|---|---|---|---|---|
| Reason | No. | % | No. | % |
| Could not be coded | 1 | 0.01 | 0 | 0.00 |
| Were classified in a higher-level category | 21 | 0.19 | 17 | 0.15 |
| Total | 22 | 0.20 | 17 | 0.15 |
Data are absolute number of cases and relative frequencies (percentages of the total number of diagnoses in the DIADERM study).
Included Diagnoses That Lacked a Specific Code in the ICD-10 Adapted for Dermatology in Spain5
| Diagnosis | No. | Higher-Level Code in the Adapted Spanish ICD-105 | Specific Code in the Draft ICD-11? |
|---|---|---|---|
| Frontal fibrosing alopecia | 3 | L66.1 Lichen planopilaris | No |
| Follicular occlusion syndrome (or follicular occlusion tetrad) | 1 | Could not be coded under any category | No |
| Sebopsoriasis | 2 | L21 Seborrheic dermatitis | No |
| Irritant dermatitis of the genitals | 2 | L24.9 Irritant contact dermatitis, unspecified cause | EK42.14 Irritant dermatitis of the vulva or EJ82.1 Irritant contact dermatitis organized by the body part affected; & XA7QV2 Penis |
| Venous malformation | 1 | Q27.8 Other specified congenital malformaciones of peripheral vascular systema | LC51 Developmental venous malformations involving the skin |
| Vascular malformation | 1 | Q27.9 Congenital malformation of the peripheral vascular system, unspecified | LC5Z Cutaneous vascular malformation, unspecified |
| Plantar pain | 1 | M79.606 Pain in lower limb, unspecified | FB56.4 Pain in limb; & XA1XM4 Sole of foot |
| Scrotodynia | 1 | N50.9 Disorder of male genital organs, unspecified | MJ90.2Z Scrotal pain, unspecified |
| Progressive macular hypomelanosis | 1 | L81.5 Leukoderma, not elsewhere classified | No |
| Pigmentary mosaicism | 1 | L81.9 Disorder of pigmentation, unspecified | No |
| Metastatic Crohn disease | 1 | L92.8 Other granulomatous disorders of the skin and subcutaneous tissue | No |
| Indolent lymphoid CD8+ proliferation of the ear | 1 | D47.9 Neoplasm of uncertain behavior of lymphoid, hematopoietic and related tissue, unspecified | No |
| Amicrobial flexural pustulosis | 1 | L13.1 Subcorneal pustular dermatitis | No |
| Infantile perianal protrusion | 1 | L91.8 Other hypertrophic disorders of the skin | No |
| Myxoid pseudocyst | 2 | L98.56 Mucinosis of the skin and Myxomaa | EL10.2 Digital myxoid pseudocyst |
| Aquagenic keratoderma | 2 | L85.82 Keratoderma, unspecified | No |
Abbreviation: ICD, International Classification of Diseases.
Data are absolute frequencies (number of cases).
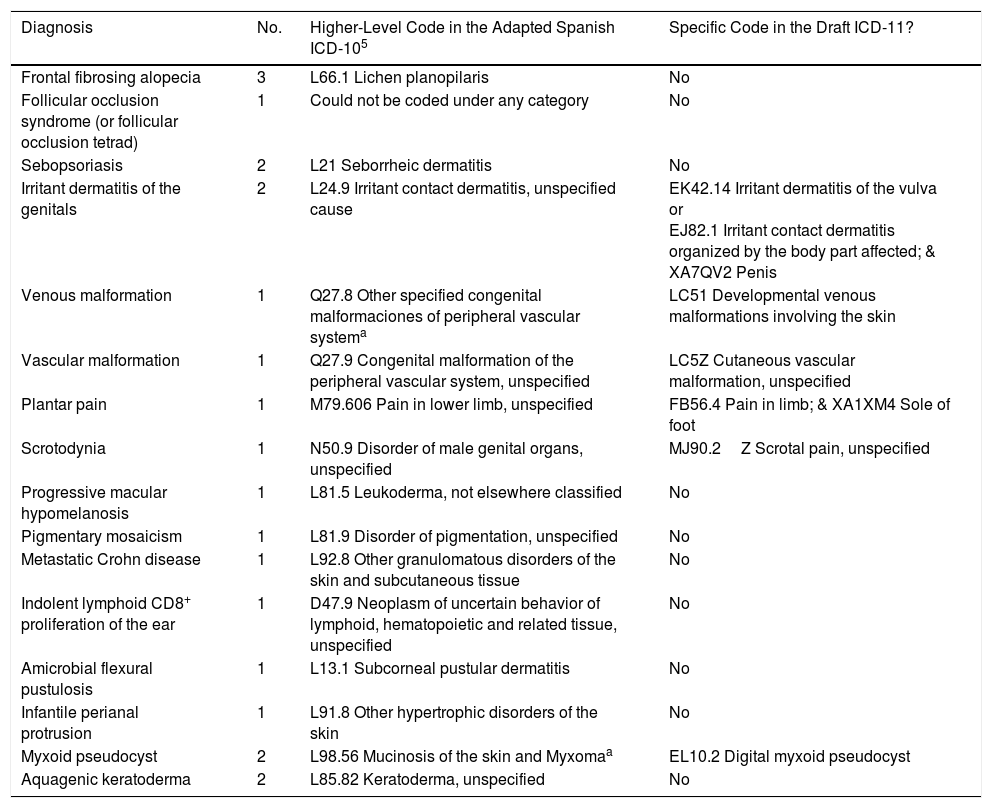
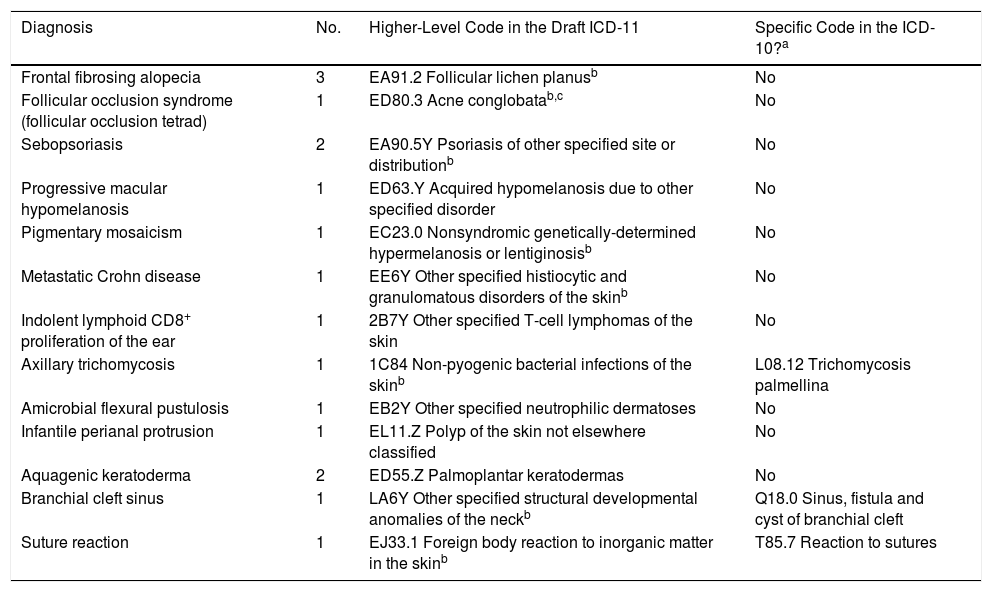
The diagnoses in 24 of the 41 cases could be assigned specific codes with the draft ICD-11 system, leaving only 17 cases uncoded (Table 2b). These 17 cases involved 13 different conditions, all of which could be grouped under the next highest category. Eight of the 13 conditions could not be given specific codes but were found in the draft ICD-11 index.
Included Diagnoses That Lacked a Specific Code in the Draft ICD-11.
| Diagnosis | No. | Higher-Level Code in the Draft ICD-11 | Specific Code in the ICD-10?a |
|---|---|---|---|
| Frontal fibrosing alopecia | 3 | EA91.2 Follicular lichen planusb | No |
| Follicular occlusion syndrome (follicular occlusion tetrad) | 1 | ED80.3 Acne conglobatab,c | No |
| Sebopsoriasis | 2 | EA90.5Y Psoriasis of other specified site or distributionb | No |
| Progressive macular hypomelanosis | 1 | ED63.Y Acquired hypomelanosis due to other specified disorder | No |
| Pigmentary mosaicism | 1 | EC23.0 Nonsyndromic genetically-determined hypermelanosis or lentiginosisb | No |
| Metastatic Crohn disease | 1 | EE6Y Other specified histiocytic and granulomatous disorders of the skinb | No |
| Indolent lymphoid CD8+ proliferation of the ear | 1 | 2B7Y Other specified T-cell lymphomas of the skin | No |
| Axillary trichomycosis | 1 | 1C84 Non-pyogenic bacterial infections of the skinb | L08.12 Trichomycosis palmellina |
| Amicrobial flexural pustulosis | 1 | EB2Y Other specified neutrophilic dermatoses | No |
| Infantile perianal protrusion | 1 | EL11.Z Polyp of the skin not elsewhere classified | No |
| Aquagenic keratoderma | 2 | ED55.Z Palmoplantar keratodermas | No |
| Branchial cleft sinus | 1 | LA6Y Other specified structural developmental anomalies of the neckb | Q18.0 Sinus, fistula and cyst of branchial cleft |
| Suture reaction | 1 | EJ33.1 Foreign body reaction to inorganic matter in the skinb | T85.7 Reaction to sutures |
Abbreviation: ICD, International Classification of Diseases.
Data are absolute frequencies (number of cases).
The specific diagnosis was found as an indexed term, for which a reference to the code shown was provided.
Acne conglobata is not strictly a higher-level term but rather one of the components of follicular occlusion syndrome (or the follicular occlusion tetrad). Nevertheless, the draft ICD-11 specifies that this syndrome should be classified under this code. The ICD-10 adapted for Spain also classifies acne conglobata under code L70.1, but follicular occlusion syndrome is not indexed there. Nor is there an indication that it should be assigned this code.
Six diagnoses that lacked a code in the ICD-10 adapted for dermatology (Table 2a) did have a code in the ICD-11. However, 3conditions with a code in the adapted ICD-10 lacked a code in the ICD-11 (Table 2b); nonetheless, all 3 were indexed.
DiscussionThe DIADERM study allowed us to obtain data for analyzing problems of diagnostic classification in routine dermatologic practice in Spain. Our analysis leads us to conclude that both the ICD-10 adapted for Spanish dermatology5 and the draft ICD-11 will correctly classify the vast majority of clinical diagnoses we make: only 0.20% of the diagnoses in the DIADERM database corresponded to conditions that were absent from the adapted ICD-10 and that percentage fell to 0.15% when we used the ICD-11.
Some of the most important dermatology classification problems of the ICD-10 had already been reported and corrected in the version adapted for dermatology in Spain.5 Nevertheless, this adaptation still contains shortcomings that affect the coding of certain diagnoses. A systematic review of all the classifications lies outside the aims of this study, and given our finding that only a small number of dermatologic diagnoses lack codes, it is difficult to see which parts of the system work better or worse. However, we have observed problems in the following areas: 1) defining the exact topography of certain diseases in which that information may be of interest (in genital eczema and metastatic Crohn disease, for example) and 2) the lack of inclusion of certain diseases, possibly because they have been described or developed only in recent decades. Examples are frontal fibrosing alopecia9; vascular malformations, whose classification and nomenclature have changed10; progressive macular hypomelanosis11; pigmentary mosaicism12; indolent acral CD8+ lymphoma13; amicrobial flexural pustulosis14; infantile perianal protrusion15; and aquagenic keratoderma.16 Sebopsoriasis also lacks a specific code, and myxoid pseudocyst seems to fall into the same category as cutaneous myxoma (as a mucous cyst) — an unfortunate decision given that a myxoid pseudocyst has no epithelial lining.17
Improvements have been made in the draft ICD-11, as our report reveals. The new system allows the user to combine a root code with one or more extension codes. This flexibility helps the coder define the exact location of a symptom or the area affected by a disease.8 The new revision also includes specific codes for several diseases not included in the ICD-10 adapted for dermatology in Spain5; in fact the new classification of vascular anomalies is a substantial improvement.8 Most of the remaining terms that lack a specific code are in the draft ICD-11 index, where they have higher-level codes indicated for them. It is true that there are 3 diagnoses in the Spanish adaptation of the ICD-10 that still lack codes in the draft ICD-11; however, all of them are present in the index. It is reasonable for a general classification of diseases, such as the ICD, to include a certain degree of “granularity” in the interest of reducing the number of codes.1,5 Here is where adapting the system to the needs of specialties can play a part in achieving greater detail,5 a feature that is essential for compiling statistics on disease prevalence and ensuring that underreporting does not take place.2,4
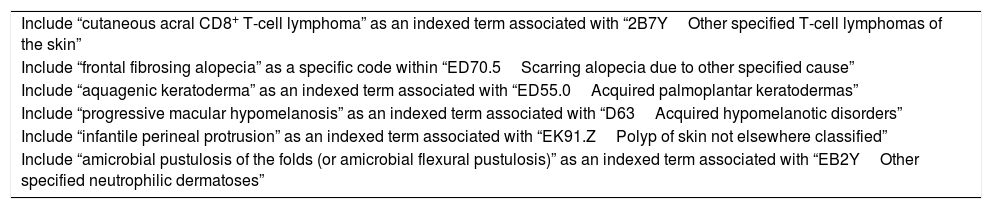
Developing a new classification system requires the collaboration of experts in the material covered, and the Dermatology Topic Advisory Group is currently working on the draft ICD-11.18 Studies to detect coding problems are particularly important at this time if we are to develop new categories. One study that detected problems in the coding of anaphylaxis,4 for example, led to expert collaboration and new codes for the draft ICD-11.19 We believe our study provides a basis for improving the classification of dermatologic diseases. In our view, all the diagnoses mentioned in our Table 3 should receive specific codes in a future dermatology adaption of the ICD-11, and those entities should at least be included as indexed terms in the general version of the tool, as their existence is well established in the literature.9–16 We also believe that frontal fibrosing alopecia should be assigned its own code. Even though incidence and prevalence data are lacking for this condition, it is not an uncommon diagnosis, in our experience, and that of others.20
Revisions Suggested for the ICD-11.
| Include “cutaneous acral CD8+ T-cell lymphoma” as an indexed term associated with “2B7YOther specified T-cell lymphomas of the skin” |
| Include “frontal fibrosing alopecia” as a specific code within “ED70.5Scarring alopecia due to other specified cause” |
| Include “aquagenic keratoderma” as an indexed term associated with “ED55.0Acquired palmoplantar keratodermas” |
| Include “progressive macular hypomelanosis” as an indexed term associated with “D63Acquired hypomelanotic disorders” |
| Include “infantile perineal protrusion” as an indexed term associated with “EK91.ZPolyp of skin not elsewhere classified” |
| Include “amicrobial pustulosis of the folds (or amicrobial flexural pustulosis)” as an indexed term associated with “EB2YOther specified neutrophilic dermatoses” |
Abbreviation: ICD, International Classification of Diseases.
We think that most of the DIADERM diagnoses that lack codes in the ICD-10 adapted for Spanish dermatology5 have been included in this study, given that the error rate of the initial coder was low and 3 dermatologists revised any coding for which doubts arose.6 However, it is still possible that we may have failed to include some diagnoses that had been assigned to higher-level categories in the database. Another important limitation is that the review of uncoded diagnoses in the present study — and thus their inclusion or exclusion as diagnoses that lacked a specific code in the ICD-10 for dermatology or the draft ICD-11 — was managed by a single coder (G. G. L.), in spite of the admitted degree of subjectivity involved. We think these limitations do not substantially change the conclusions that can be reached.
In summary, we conclude that the ICD-10 adapted for dermatology in Spain5 and the draft ICD-11 appropriately classify the vast majority of diagnoses made routinely in dermatology practices. Since the methods used to create the DIADERM database ensure that the diagnoses listed are highly representative of practice in this country,6 we conclude that these classification systems allow us to study the real characteristics of our caseloads. Nonetheless, we were able to detect shortcomings in the dermatology adaptation of the ICD-10,5 particularly with respect to diagnoses that have emerged in recent decades. Classification systems clearly need to be kept up to date, and once the final version of the ICD-11 is published it would be useful to form a group to collaborate on that task. We think that including the suggestions we have made for the ICD-11, and also adapting the new system for dermatology, would help with the problem of underreporting as well as with the compiling of statistics on mortality rates in dermatology and the prevalence of currently underdiagnosed skin diseases.
FundingThe DIADERM study, which is supported by the Healthy Skin Foundation of the Spanish Academy of Dermatology and Venereology (AEDV), has received funding from Novartis. Novartis did not participate in data collection, data analysis, or interpretation of the results. Guillermo González-López received a Juan de Azúa Grant from the AEDV's Healthy Skin Foundation to support his work on this paper.
Conflicts of InterestThe authors do not recognize any conflicts of interest in relation to this article.
The DIADERM project was made possible thanks to the collaboration of regional coordinators and local participants.
Section coordinators: Agustín Buendía, Pablo Fernández-Crehuet, Husein Husein-ElAhmed, Jesús Vega, Agustín Viera, José Manuel Carrascosa, Marta Ferrán, Enrique Gómez, Lucia Ascanio, Ignacio García Doval, Salvador Arias, and Yolanda Gilaberte.
Participants: Juan A. Sánchez, Amalia Serrano, Rosa Castillo, Ramón Fernandez, José Armario, Carolina Lluc Cantalejo, Cristina Albarrán, María Cruz Martín, Juan Antonio Martín, Román Barabash, Lara Pérez, Manuel Salamanca, Carlos Hernández, José Francisco Millán, Inmaculada Ruiz, Susana Armesto, Marta González, Valia Beteta, Concepción Cuadrado de Valles, Pilar Cristóbal, María Magdalena Roth, Juan Garcias, Ricardo Fernandez de Misa, Estela García, María del Pino Rivero, José Suárez, Birgit Farthmann, Alba Álvarez, Irene García, Caridad Elena Morales, María Cristina Zemba, Trinidad Repiso, Carmen Sastre, María Ubals, Alejandro Fernández, Urbà González, Ramón Grimalt, Sara Gómez, Ingrid López, Franco Antonio Gemigniani, María José Izquierdo, Fernando Alfageme, Nuria Barrientos, Laura María Pericet, Santiago Vidal, Celia Camarero, Pablo Lázaro, Cristina García, María Pilar de Pablo, Pedro Herranz, Natalia del Olmo, María Castellanos, Natalia Jiménez, Sonsoles Aboín, Isabel Aldanondo, Adriana Juanes, Dulce María Arranz, Olga González, Luis Casas, Juan José Vázquez, Carmen Peña, José Luis Cubero, Carlos Feal, María Eugenia Mayo, Nicolás Iglesias, Rafael Rojo, Elfidia Aniz, Sabrina Kindem, Nerea Barrado, Marisa Tirado, Ester Quecedo, Isabel Hernández, Antonio Sahuquillo, Rebeca Bella, Ramón García, Anaid Calle, Francesc Messeguer, Alberto Alfaro, Luisa Casanova, Libe Aspe, María Pilar Moreno, Izaskun Trébol, Gonzalo Serrano, Víctor Manuel Alcalde, Patricia García, and Carmen Coscojuela.
Please cite this article as: González-López G, García-Doval I, Molina-Leyva A, Descalzo-Gallego MA, Taberner R, Gilaberte Y, et al. Problemas de la CIE-10 para la codificación de diagnósticos dermatológicos. Estudio DIADERM. Actas Dermosifiliogr. 2018;109:893–899.