Sebaceous carcinoma is a rare, aggressive adnexal tumor of unknown etiology; 75% of these tumors arise in the periocular region while 25% arise at extraocular sites. This cutaneous tumor is a diagnostic sign of Muir-Torre syndrome, a disorder associated with visceral malignancies and gene abnormalities. Patients with sebaceous carcinoma should therefore be carefully evaluated; a detailed personal and family history of cancer, a thorough physical examination, additional tests where appropriate, and close monitoring will all be required.
We report 2 cases of extraocular sebaceous carcinoma and review the literature, focusing on the association between sebaceous carcinoma and Muir-Torre syndrome.
El carcinoma sebáceo es un tumor anexial raro y agresivo. Su etiología es desconocida. El 75% de estos tumores son de localización periocular y el 25% extraocular. Es uno de los marcadores cutáneos diagnósticos del síndrome de Muir-Torre, una enfermedad genética asociada a neoplasias viscerales. Por lo tanto, los pacientes con carcinoma sebáceo deben ser cuidadosamente valorados, realizándose una historia oncológica personal y familiar adecuada, una exploración física cuidadosa, pruebas complementarias necesarias y un seguimiento estrecho.
Se presentan 2 casos de carcinomas sebáceos extraoculares y se realiza una revisión de la literatura, destacando la asociación entre el carcinoma sebáceo y el síndrome de Muir-Torre.
Sebaceous carcinoma is a rare adnexal tumor that follows an aggressive clinical course, with a risk of local recurrence and distant metastasis. Its etiology is unknown. Three-quarters of cases occur in the periocular region, although the tumor can present on any part of the body.1,2
Sebaceous carcinoma may resemble an inflammatory disease or another tumor, leading to delays in diagnosis, inappropriate treatments, and increased morbidity and mortality. It is also one of the cutaneous diagnostic markers of Muir-Torre syndrome, a genetic disease associated with visceral neoplasms. Therefore, patients with sebaceous carcinoma should be carefully assessed by taking an extensive personal and family oncologic history, performing a detailed physical examination, and ordering any additional tests.1,3 Patients should then be closely followed-up.
Clinical Case 1We present the case of a 48-year-old woman, whose only history of interest was hypothyroidism, attended in our clinic for the appearance and rapid growth of a lesion in the left axilla. The tumor was asymptomatic. In the physical examination, a mass measuring 3cm across was found. The exophytic, papilliform lesion was pedunculated and of yellowish coloration (Fig. 1). There were no enlarged lymph nodes.
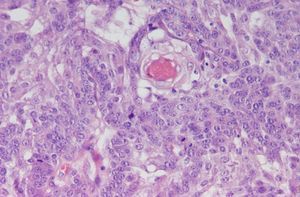
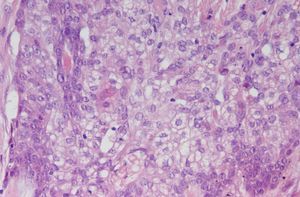
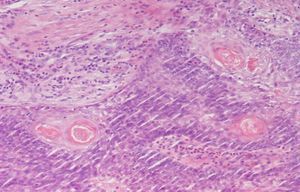
The tumor was excised and biopsied. The pathologic analysis showed a nodular lesion with surface ulceration. Areas of malignant proliferation could be seen, with tumor cells growing to form solid lobes. Under higher magnification, 2 cell populations were observed, 1 of small basaloid cells (Fig. 2) and 1 of cells with characteristic sebaceous differentiation and cytoplasmic vacuolization (Fig. 3). Sebaceous cells at different stages of maturity were seen in the specimen. Some of these formed glandular structures that contained an eosinophilic substance (Fig. 4). Immunohistochemical staining was positive in patches for epithelial membrane antigen (EMA). The histopathologic findings confirmed diagnosis of sebaceous carcinoma. A study of microsatellite instability was not possible.
The surgical margins of the lesion were then extended (1cm for the lateral margins and 2cm for the deep margins). No tumor remnants were detected.
The study of disease progression consisted of axillary ultrasonography, in which nonspecific enlarged axillary lymph nodes were observed, measuring approximately 2cm across, and computed tomography of the thorax, abdomen, and pelvis, which was normal. In order to rule out visceral neoplasms in a possible Muir-Torre syndrome, gynecologic ultrasonography, cervical cytology, and gastroscopy were also performed. Colonoscopy revealed a hyperplasic polyp, which was confirmed by histology.
After this complete study, the patient's medical history was updated with the information that her maternal grandmother had breast cancer.
Three months after excision of the sebaceous carcinoma, a new nodule had appeared on the left cheek. Biopsy of that lesion confirmed the presence of a squamous cell carcinoma on an epidermal cyst. The entire lesion was excised.
Currently, after 3 years of follow-up in the dermatology and gastroenterology departments of the hospital, the patient is asymptomatic and shows no signs of local recurrence or metastasis.
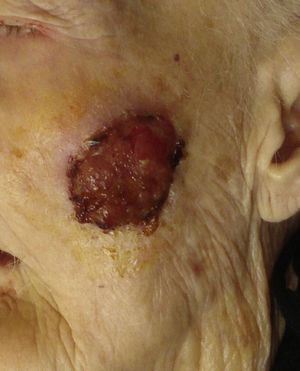
Clinical Case 2A 96-year-old woman with a personal history of hypertension, repeated transient ischemic attacks, and advanced Alzheimer disease was referred to our clinic for a lesion of several years growth on the left cheek. In the physical examination, a mass measuring 4cm was found. The lesion was exophytic and ulcerated, with a tendency to bleed (Fig. 5). No palpable regional lymph nodes were detected.
The lesion was diagnosed as sebaceous carcinoma in the histologic study. A study of microsatellite instability could not be performed.
Computed tomography showed that only the skin was involved, with no invasion of subcutaneous tissue or deep structures. After excision, the surgical defect was closed with a local flap technique.
No family history of visceral neoplastic disease or skin tumors of the sebaceous type was found on further investigation. Given the advanced age of the patient and her comorbidities, no further tests were performed to rule out internal tumors. After 8 months of follow-up, there were no signs of local recurrence or metastasis.
DiscussionSebaceous carcinoma is a rare adnexal tumor characterized by its aggressive course. Local recurrence is reported in more than one-third of cases, while lymph node metastasis and distant metastasis occur in 25%.1,2 The etiology is not known. One hypothesis is that the tumor originates in the epithelium of sebaceous glands,2 but recent studies suggest that it may be derived from a pluripotent cell able to differentiate into any cell line, including sebaceous cells.1
Sebaceous carcinoma can present in any part of the body where sebaceous glands are present.2 Three-quarters of cases occur in the periocular region, particularly on the eyelids. There are up to 5 types of sebaceous glands in this region, although the meibomian glands are the ones most frequently affected.1,2 The most common extraocular site is the head and neck (20%),2 as in our second case, followed by other hairy regions of the body (as in our first case) including the genitals (5%).1For years, the extraocular tumors were thought to have a worse prognosis.2 At present though, the biological behavior and prognosis of sebaceous carcinoma are not considered to depend on the site of presentation.1,3–5
Clinically, sebaceous carcinoma presents as an occasionally pedunculated subcutaneous nodule or mass of firm consistency whose coloration varies between pinkish and red, although it sometimes has a yellowish tone. In one-third of the cases, there is a tendency for ulceration and spontaneous bleeding. Generally, these tumors are not painful1–3 or symptomatic, as was the case in our 2 patients. The clinical and histologic findings for this carcinoma may resemble an inflammatory disease (chalazion, blepharitis) or other tumors (sebaceous adenoma, basal cell carcinoma, and squamous cell carcinoma). The lack of strong clinical pathologic correlation in sebaceous carcinoma can cause a delay in diagnosis, inappropriate treatment, and an increase in morbidity and mortality.1,2
Sebaceous carcinoma is most common in elderly individuals and in women, as shown in a recent study in which the mean age of patients was 72 years and 73% were women.6 Most sebaceous carcinomas are de novo lesions,1 although cases have been reported of such tumors arising on a preexisting sebaceous nevus.7,8
Sebaceous carcinoma has been associated with Muir-Torre syndrome, a hereditary disease of autosomal dominant transmission. Muir-Torre syndrome is characterized by the association of at least a skin tumor of sebaceous lineage (sebaceous adenoma, sebaceoma, sebaceous epithelioma, sebaceous carcinoma, or basal cell carcinoma with sebaceous differentiation), with or without a keratoacanthoma associated with 1 or more visceral neoplasms. The most frequently associated visceral tumors are gastrointestinal, located mainly in the proximal colon, followed by tumors of the genitourinary tract.9–12 Approximately 23% of the patients with Muir-Torre syndrome have sebaceous carcinoma.1,10 Thus, when patients present with a sebaceous carcinoma, they should be carefully screened by taking a personal and family history of cancer and performing a full physical examination and baseline laboratory tests.1,10 Patients should then be referred to internal medicine for a preliminary study and appropriate follow-up. Lesions associated with Muir-Torre syndrome often have unstable microsatellites, in which there is DNA repair defect after replication due to a mutation in the MutS homolog (MSH)-2, the MutL homolog (MLH)-1, and more recently and less often the MSH-6 genes. The proteins coded by these genes can be used in screening to enable early identification of this syndrome.9,10,12,13
Histologically, sebaceous carcinoma can be well, moderately, or poorly differentiated. Tumor cells have hyperchromatic nuclei of variable shapes and sizes, with high mitotic activity and basaloid characteristics. Less well differentiated cells contain a lipid-rich eosinophilic cytoplasm, giving a foamy appearance.1,2 The presence of sebaceous differentiation can be shown by staining with Oil Red O or Sudan IV, or with immunohistochemical markers such as EMA and Leu-M1.1
The treatment of choice for the sebaceous carcinoma is excision with margins of 5 to 6mm.1,2 Local recurrence occurs in 32% of the cases.1,13 Use of Mohs micrographic surgery has been reported, with lower local recurrence rates (approximately 12%).13,14 Sentinel node biopsy has been used to identify subclinical metastasis in both ocular and extraocular sebaceous carcinomas, but it is not a standard technique and its clinical utility has not been established.15 Radiotherapy has been used in the treatment of metastatic sebaceous carcinoma, in patients with orbital involvement who refuse excision, and in elderly patients with local recurrence.1
With the exception of sebaceous hyperplasia, diagnosis of any sebaceous neoplasm such as sebaceous carcinoma can be important for the diagnosis of Muir-Torre syndrome. The role of the dermatologist is essential for the diagnosis, assessment, and follow-up of these patients.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Cieza-Díaz DE, et al. Carcinoma sebáceo extraocular: presentación de 2 casos. Actas Dermosifiliogr. 2012;103:919–22.