Epidermal nevi, which are benign skin growths, have been treated using a range of approaches, with varying results. Topical treatments are ineffective and, while surgical excision is a more definitive treatment, it causes scar formation. In recent decades, epidermal nevi have been treated with various types of laser therapy. We describe our experience with the use of carbon dioxide (CO2) laser therapy to treat epidermal nevi and inflammatory linear verrucous epidermal nevi (ILVEN).
Patients and methodsTwenty patients (15 with epidermal nevi and 5 with ILVEN) underwent CO2 laser treatment at our hospital between 2002 and 2010.
ResultsResponse was good (>50% reduction in lesion size) in 50% of cases and excellent (>75% reduction) in 30%. A greater resistance to treatment was observed in patients with ILVEN (only 40% had a good response). Long-term follow-up (at least 18 months) showed a recurrence rate of 30%. The side effects were hypopigmentation (25% of patients) and scarring (20%).
ConclusionsWe consider CO2 laser therapy to be the treatment of choice for epidermal nevi as it is well tolerated and has proven to be safe and effective in the long term. While the response in patients with ILVEN was limited, CO2 laser therapy might be a good option for selected cases or for palliative treatment since no other treatments have yet proven effective in this setting.
Los nevos epidérmicos son proliferaciones benignas de la epidermis para los que se han utilizado múltiples tratamientos con resultados variables. Las terapias tópicas resultan ineficaces y el tratamiento quirúrgico obtiene resultados más definitivos, pero conlleva la aparición de cicatrices. En las últimas décadas se han utilizado diversas modalidades de láser. El objetivo del trabajo es describir nuestra experiencia en el tratamiento de nevos epidérmicos y nevos epidérmicos verrugosos inflamatorios lineales (NEVIL) con láser de CO2.
Pacientes y métodosVeinte pacientes (15 con nevos epidérmicos y 5 con nevo epidérmico verrugoso inflamatorio lineal) fueron tratados con láser de CO2 entre 2002 y 2010 en nuestro centro.
ResultadosUn 50% de los pacientes presentaron buena respuesta (reducción de la lesión mayor del 50%) y un 30% respuesta excelente (reducción mayor del 75%). Los pacientes con NEVIL mostraron mayor resistencia al tratamiento (40% buena respuesta). Se realizó seguimiento a largo plazo (mínimo de 18 meses) y se observaron recurrencias en el 30% de los pacientes. Los efectos secundarios detectados fueron: hipopigmentación en el 25% de los pacientes y cicatrices en el 20%.
ConclusionesConsideramos el láser de CO2 como el tratamiento de elección para estas lesiones, ya que es bien tolerado y se ha demostrado su eficacia y seguridad a largo plazo. Aunque la respuesta es limitada en los NEVIL, no existen en la actualidad otros tratamientos eficaces, por lo que podría ser una buena opción terapéutica en casos seleccionados o como tratamiento paliativo para la mejoría de los síntomas.
Epidermal nevi are hamartomas in the epidermis. Although the reasons for their development are poorly understood, they are thought to derive from pluripotent epidermal cells and have been linked to various mosaic mutations. These nevi are estimated to be present in 1 in 1000 births, but they may also manifest during infancy, childhood or even adolescence and adulthood.1
Appearing clinically as highly keratotic and pigmented papules that coalesce to form well-defined papillomatous plaques, epidermal nevi may be found along Blaschko lines on the skin in any part of the body. Generally asymptomatic, they may be slightly hyperkeratotic or highly verrucous2 and either localized or widespread in their distribution. The lesions of nevus unius lateris are large and found on a single side of the body. Ichthyosis hystrix nevi, on the other hand, have a bilateral distribution, with lesions appearing over large areas of the trunk.
In epidermal nevus syndrome, also known as Solomon syndrome, nevus formation is associated with neurologic, ocular, musculoskeletal, or organ (cardiac and genitourinary) abnormalities. Before coming to a diagnosis of epidermal nevus, particularly if lesions are generalized, the physician should rule out the presence of such associated conditions.1,2
Inflammatory linear verrucous epidermal nevus (ILVEN) is another type. The lesions in this condition have a more inflammatory, psoriasiform appearance. They usually form in childhood and are more common in females. Linear plaques are typically unilateral and located on the lower limbs. Pruritus may be intense, and an alternative diagnosis of linear psoriasis is sometimes investigated.3
Epidermal nevi are asymptomatic and their course is benign, but as patients seek treatment for cosmetic reasons, many therapeutic modalities have been tried with varying degrees of success. Topical or intralesional corticosteroids and other topical agents (calcipotriol, 5-fluorouracil, podophyllin, retinoids, the combination of 5% 5-fluorouracil and 1% tretinoin, and chemical peelings4–6) have usually been ineffective. Surgery achieves more definitive results but as unsightly scars may form, this option can only be used for small lesions.7 Cryotherapy, dermabrasion, electrosurgery, and various types of laser therapy have also been tried.8,9 Photodynamic therapy has recently been reported to give good results in single cases of verrucous epidermal nevus (VEN)10 and ILVEN.11
These modalities have not been compared in clinical trials to date. Carbon dioxide (CO2) laser treatment of epidermal nevi has been studied in case series and found to be effective and safe.7
We describe our experience using CO2 laser therapy for epidermal nevi in a series of 20 patients. Our aim is to evaluate treatment effectiveness and patient satisfaction after long-term follow-up.
Patients and MethodsWe conducted a retrospective study of a series of 20 patients treated in the laser therapy unit of our hospital. Fifteen patients with VEN and 5 patients with ILVEN underwent CO2 laser therapy between January 2002 and May 2010. To rule out the associated conditions of epidermal nevus syndrome, patients underwent age- and symptom-appropriate complementary studies. Tests done included neurologic examination, including electroencephalography; eye examination, including inspection of the ocular fundus; musculoskeletal examinations (chest radiography, bone series); and visceral organ examination (abdominal ultrasound). The diagnosis of ILVEN was based on histologic findings in all cases. After a description of the treatment, including its possible side effects, the patients gave their written consent.
A test dose was first applied to an area measuring approximately 2 to 3cm2 to estimate how effective the treatment would be; if the test was satisfactory, therapy was scheduled. Treatments were given in an operating room, and all patients wore protective glasses. The skin was pretreated with chlorhexidine, and a local anesthetic (mepivacaine 1%) was applied to the targeted area.
A continuous wave CO2 laser device (Sharplan 1060, Laser Industries Ltd, Tel Aviv, Israel) was set to deliver light at a wavelength of 10 600nm in unfocused mode with a beam diameter of 2mm. Laser power ranged from 4W to 15W, depending mainly on the thickness, or degree of keratosis, of the lesions. Complete nevus tissue destruction was undertaken for the area assigned for treatment at a single session. Depending on nevus characteristics, the operator made 1 to 4 passes with the beam until destruction seemed complete according to visual inspection. Between passes, necrotic tissue was wiped away with gauze soaked in normal saline. Pressure could also be applied to the gauze to control bleeding. Treatment aimed to destroy the nevus. Destruction included the underlying papillary dermal component as well as the epidermal component to avoid recurrence, which could be expected if a more superficial approach were taken. If the laser reached the reticular dermis, however, the risk of scarring would increase. Thus, the safety margin is narrow in this procedure. Once the hyperkeratotic superficial component had been removed, the smooth, pinkish surface of the papillary dermis became visible. At this point, after necrotic tissue had been wiped away, the operator made a final pass to coagulate the surface vessels. As some patients had lesions that extended over a large area, it was sometimes necessary to schedule multiple sessions in order to treat all affected areas. Between 1 and 10 sessions were required in the series (mean, 2.8 sessions). Wound care after the treatments consisted of daily application of an antibiotic cream (fusidic acid) and occlusion with a nonadherent dressing (Tulgrasum). Any ulceration of the area that developed after treatment was seen to heal in 10 to 15 days without complications. All patients had residual erythema that resolved gradually during the month following treatment.
Nevi were classified by extension of the affected area into 3 groups reflecting divisions used in previously published series7,12: less than 20cm2, between 20 and 100cm2, and more than 100cm2.
The degree of hyperkeratosis, or thickness, of a lesion was measured using vernier calipers and also classified in 3 groups: less than 1mm, between 1 and 3mm, and more than 3mm.
As in previously published series,7,12 clinical response was assessed subjectively. The percentage of remission or disappearance of the nevus in the treated area in comparison with baseline was assessed, with response defined as nil or poor if remission was 25% or less, moderate if between 25% and 50%, good if between 50% and 75%, and excellent if greater than 75%.
To evaluate the results of therapy, 2 months after sessions ended 2 independent dermatologists compared the nevus area with pre-treatment photographs. The evaluation was repeated yearly thereafter for the duration of follow-up.
The patient's level of satisfaction was also recorded as not very satisfied, moderately satisfied, satisfied, or very satisfied.
All patients were followed long-term. Mean (SD) follow-up was 42(25.5) months (range, 18–96 months). Adverse events or recurrences after treatment were also recorded.
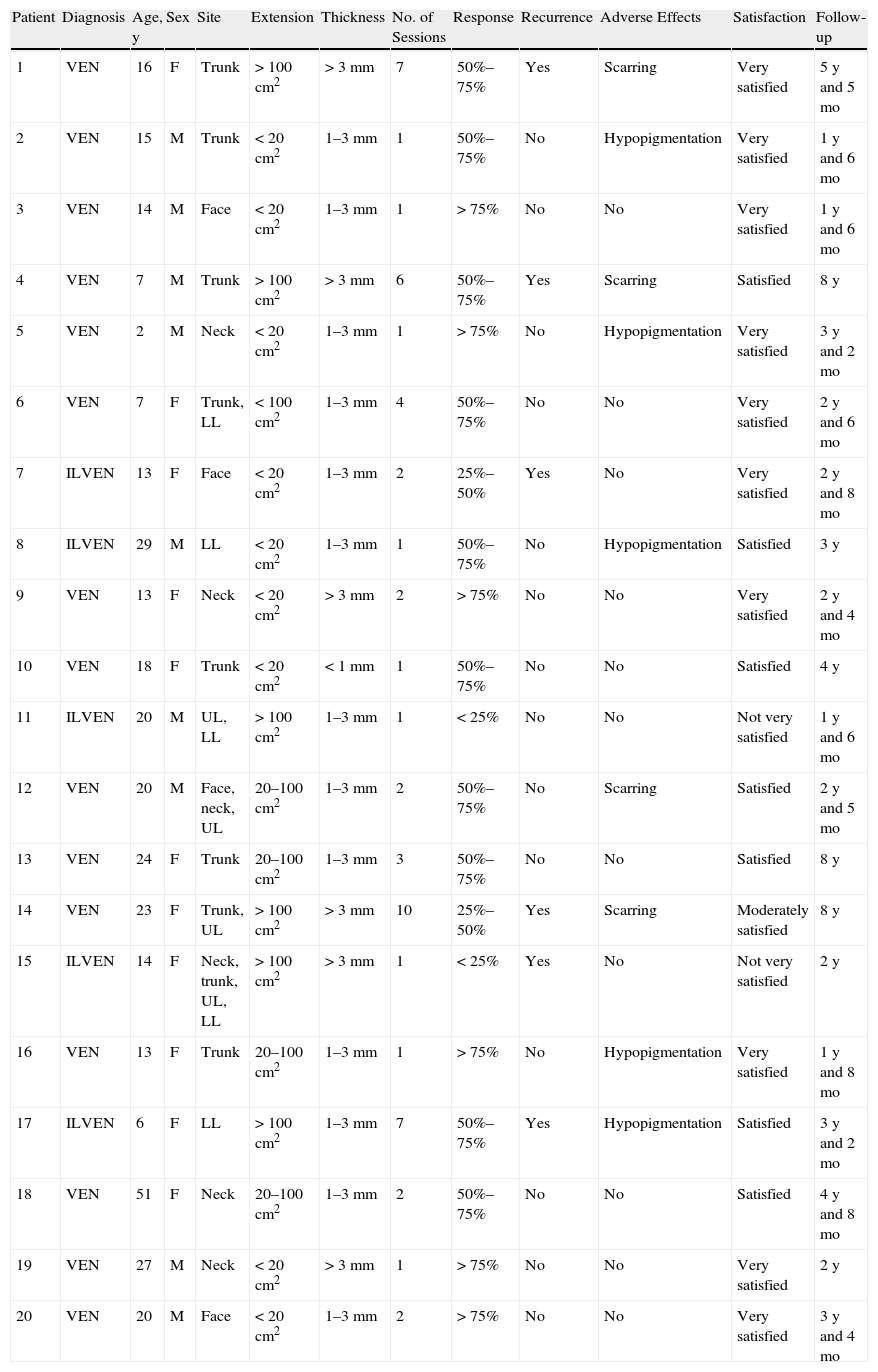
ResultsPatient characteristics and treatment responses are summarized in Table 1. The ages of the 20 patients (13 women, 7 men) ranged from 2 to 51 years (mean, 33.5 years). The lesions were located on the trunk in 6 patients, on the face in 3, on the neck in 4, and on the lower limbs in 2. Five patients had lesions on 2 or more areas. Nine patients (45%) had lesions affecting less than 20cm2, 4 (20%) had lesions extending between 20 and 100cm2, and 7 (35%) had lesions over areas larger than 100cm2. The thickness of the lesion was less than 1mm in 1 case (0.5%), between 1 and 3mm in 13 cases (65%), and more than 3mm in 6 cases (30%). Thirteen patients (65%) had been treated previously. Among the treatment approaches used were surgery (5 patients), cryotherapy (3 patients), topical retinoids (2 patients), and electrocoagulation (1 patient). Three patients with ILVEN had previously undergone pulsed dye laser treatments.
Patient and Clinical Characteristics in Epidermal Nevus Cases Treated With Carbon Dioxide Laser Therapy.
| Patient | Diagnosis | Age, y | Sex | Site | Extension | Thickness | No. of Sessions | Response | Recurrence | Adverse Effects | Satisfaction | Follow-up |
| 1 | VEN | 16 | F | Trunk | > 100cm2 | >3mm | 7 | 50%–75% | Yes | Scarring | Very satisfied | 5 y and 5 mo |
| 2 | VEN | 15 | M | Trunk | <20cm2 | 1–3mm | 1 | 50%–75% | No | Hypopigmentation | Very satisfied | 1 y and 6 mo |
| 3 | VEN | 14 | M | Face | <20cm2 | 1–3mm | 1 | >75% | No | No | Very satisfied | 1 y and 6 mo |
| 4 | VEN | 7 | M | Trunk | >100cm2 | >3mm | 6 | 50%–75% | Yes | Scarring | Satisfied | 8 y |
| 5 | VEN | 2 | M | Neck | <20cm2 | 1–3mm | 1 | >75% | No | Hypopigmentation | Very satisfied | 3 y and 2 mo |
| 6 | VEN | 7 | F | Trunk, LL | <100cm2 | 1–3mm | 4 | 50%–75% | No | No | Very satisfied | 2 y and 6 mo |
| 7 | ILVEN | 13 | F | Face | <20cm2 | 1–3mm | 2 | 25%–50% | Yes | No | Very satisfied | 2 y and 8 mo |
| 8 | ILVEN | 29 | M | LL | <20cm2 | 1–3mm | 1 | 50%–75% | No | Hypopigmentation | Satisfied | 3 y |
| 9 | VEN | 13 | F | Neck | <20cm2 | >3mm | 2 | >75% | No | No | Very satisfied | 2 y and 4 mo |
| 10 | VEN | 18 | F | Trunk | <20cm2 | <1mm | 1 | 50%–75% | No | No | Satisfied | 4 y |
| 11 | ILVEN | 20 | M | UL, LL | >100cm2 | 1–3mm | 1 | <25% | No | No | Not very satisfied | 1 y and 6 mo |
| 12 | VEN | 20 | M | Face, neck, UL | 20–100cm2 | 1–3mm | 2 | 50%–75% | No | Scarring | Satisfied | 2 y and 5 mo |
| 13 | VEN | 24 | F | Trunk | 20–100cm2 | 1–3mm | 3 | 50%–75% | No | No | Satisfied | 8 y |
| 14 | VEN | 23 | F | Trunk, UL | >100cm2 | >3mm | 10 | 25%–50% | Yes | Scarring | Moderately satisfied | 8 y |
| 15 | ILVEN | 14 | F | Neck, trunk, UL, LL | >100cm2 | >3mm | 1 | <25% | Yes | No | Not very satisfied | 2 y |
| 16 | VEN | 13 | F | Trunk | 20–100cm2 | 1–3mm | 1 | >75% | No | Hypopigmentation | Very satisfied | 1 y and 8 mo |
| 17 | ILVEN | 6 | F | LL | >100cm2 | 1–3mm | 7 | 50%–75% | Yes | Hypopigmentation | Satisfied | 3 y and 2 mo |
| 18 | VEN | 51 | F | Neck | 20–100cm2 | 1–3mm | 2 | 50%–75% | No | No | Satisfied | 4 y and 8 mo |
| 19 | VEN | 27 | M | Neck | <20cm2 | >3mm | 1 | >75% | No | No | Very satisfied | 2 y |
| 20 | VEN | 20 | M | Face | <20cm2 | 1–3mm | 2 | >75% | No | No | Very satisfied | 3 y and 4 mo |
Abbreviations: F, female; ILVEN, inflammatory linear verrucous epidermal nevus; LL, lower limbs; M, male; UL, upper limbs; VEN, verrucous epidermal nevus.
Patient number 4 (diagnosis, VEN) had multiple lesions on a large area of the trunk. The entire nevus was not treated in this case. Rather, the laser was applied to areas the patient and the dermatologists identified as most important for cosmetic purposes.
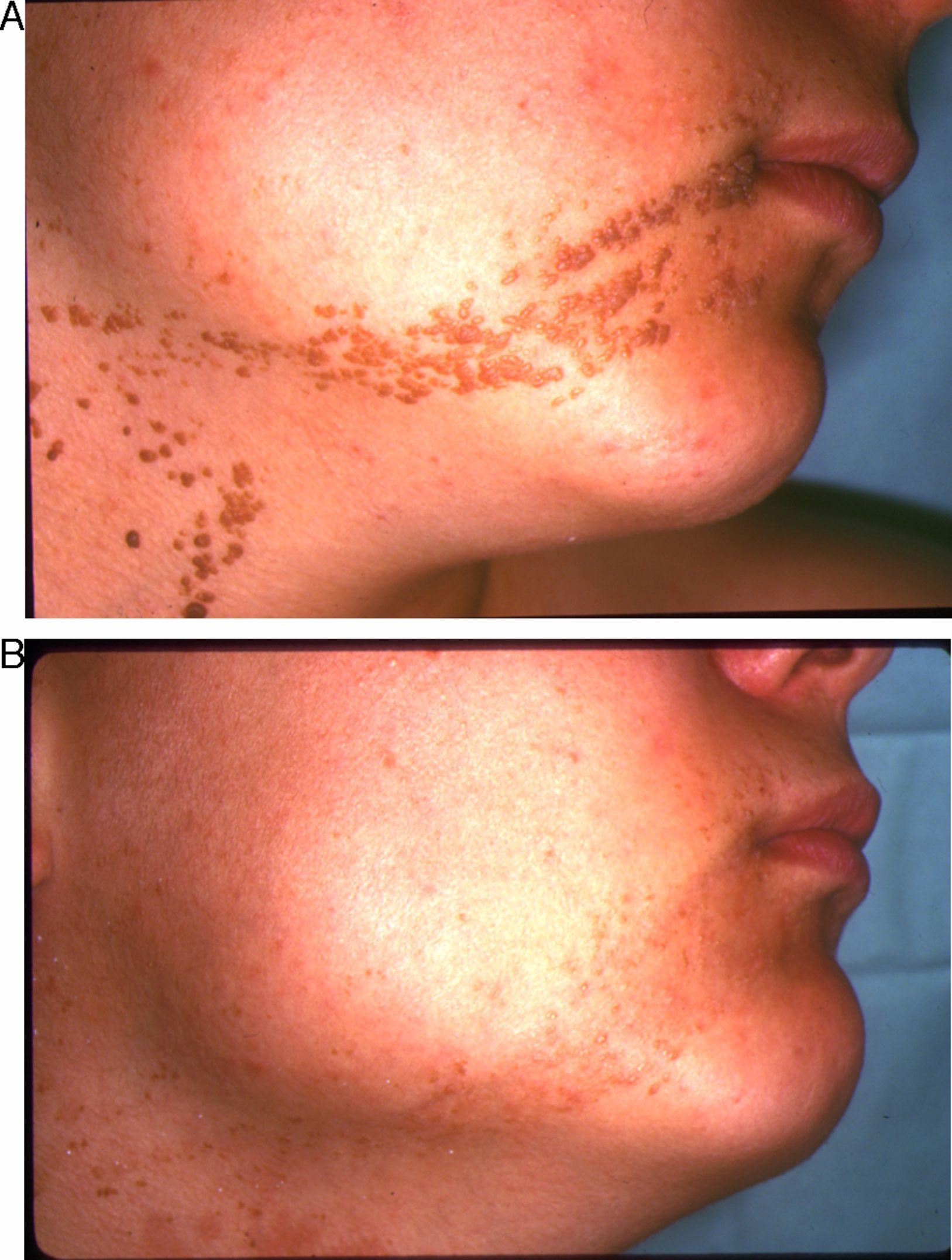
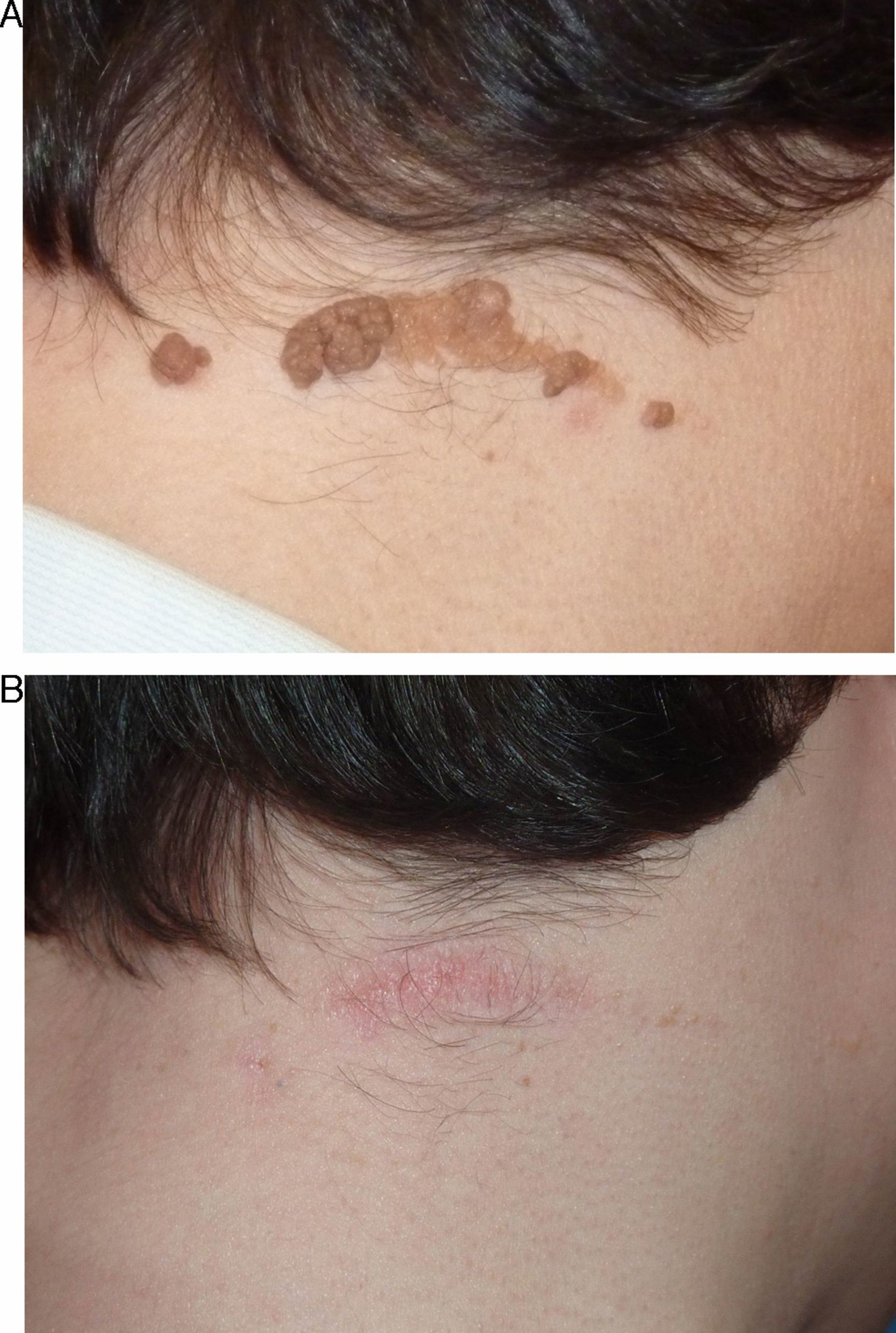
In the short term, response was nil or poor in 2 patients (10%), moderate in 2 (10%), good in 10 (50%), and excellent in 6 (30%) (Figs. 1–3). Of the 5 patients with ILVEN, 2 (40%) had no response or poor response, 1 (20%) had a moderate response, and 2 (40%) had a good response (Fig. 4). Given the lack of effect of laser therapy in the 2 ILVEN cases with no or poor response (patients 11 and 15), only a single laser session was performed even though the patients’ lesions affected large areas.
The symptoms of patients with ILVEN—mainly pruritus—did improve in the treated area, however, in spite of the poor overall response in these cases.
Long-term follow-up revealed that 6 of the 20 patients (30%) had recurrences. Lesions recurred within 3 months in 2 patients, between 3 and 6 months in 1 patient, between 6 and 12 months in 2 patients, and after more than 18 months in 1 patient. Recurrence was more common in patients with ILVEN (3 out of 5 cases) and in patients whose epidermal nevi affected an area exceeding 100cm2 (3 out of 4 cases).
On analysis of the relationships between therapeutic response and certain nevus characteristics, we saw that the response was less satisfactory in patients with a diagnosis of ILVEN (3 had a rate of response of less than 50%). Extension, location, and thickness were also considered. Response was better when lesions affected an area measuring less than 20cm2 (excellent response in 5 of the 7 patients with small VEN) and when lesions were on the face and neck (excellent response in 5 of 6 patients with VEN in these locations) (Figs. 1–3). No clear link between thickness and response was observed.
Adverse effects were noted in 9 of the 20 patients (45%). Hypopigmentation was observed in 5 patients and atrophic scarring in 4, although none developed hypertrophic scars or keloids. No occurrences of postinflammatory hyperpigmentation were seen after treatments.
Two patients (10%) said their degree of satisfaction was low. One (5%) was moderately satisfied, 7 (35%) were satisfied, and 10 (50%) were very satisfied.
DiscussionEpidermal nevi are benign but they can cause significant problems for patients if they are unsightly. Although a large variety of treatment modalities have been tried, these nevi continue to be a source of frustration because it is difficult to eliminate them definitively and yet avoid scarring.
Laser therapy destroys a nevus and leaves minimal residual scarring. Various types of lasers have been used for this purpose with varying degrees of success. Argon laser therapy12 and pulsed ruby laser therapy13 have been applied to treat the epidermal and highly pigmented components of lesions, respectively, with limited success. Ablative lasers applied have included erbium:YAG and CO2 lasers. In series showing excellent cosmetic results of erbium: YAG laser treatments, authors have also reported absence of recurrence in long-term follow-up (24 months).8,14 The patients in these studies had superficial or small lesions, however. Thicker (more hyperkeratotic) nevi, on the other hand, may not respond or treatment may cause hypertrophic scars.7
CO2 laser treatment has been applied to epidermal nevi in many studies. CO2 laser devices emit light in the infrared spectrum at a wavelength of 10 600nm. Water vaporized from tissue is the main chromophore in this modality, in a process that succeeds in destroying tissue and coagulating surface vessels. Several CO2 laser modalities are currently available.15 The main problem in using a continuous beam is the nonspecific tissue damage that heat causes. Such damage can reach 0.5 to 1mm below the surface, causing adverse effects such as color changes and, more rarely, scarring.16 Risk can be minimized, however, by expert management.
In 1986 Ratz and coworkers17 used a continuous CO2 laser to treat 15 patients with epidermal nevi, obtaining good results in half the series. In a later series of 43 patients (2 with ILVEN) CO2 laser treatments achieved better results than argon laser therapy for highly verrucous or keratotic lesions.12 The same group successfully used this modality (with power up to 25W) to treat an extensive epidermal nevus without causing scarring or seeing recurrence over a period of 4 years.18 More recently, Thual and coworkers19 achieved excellent results (86% cured or greatly improved) with CO2 laser therapy in 21 patients with VEN. The rate of recurrence was moderate at 38% in long-term follow-up in that study, in which patient satisfaction was very high.
With superpulsed and ultrapulsed lasers, there is greater control over thermal damage and the depth of tissue destruction; thus, scarring is less likely.7,20 Michel and coworkers21 achieved excellent results when treating 5 patients with linear epidermal nevi. Those authors proposed repeated passes with low-power beams to reduce the risk of scarring. Boyce and Alster22 also reported good long-term results of using a short-pulse CO2 laser and a similar technique. A 2007 report of a series of 25 patients with epidermal nevi treated with a superpulsed CO2 laser modality found that outcome was influenced most by the degree of hyperkeratosis.7 The authors reported good results in 92% of flat nevi and only 33% of highly keratotic nevi. The recurrence rate was 60%.
ILVEN is a much less common condition than noninflammatory forms of epidermal nevus, but the intense pruritus that accompanies ILVEN is highly debilitating. Clinically and histologically, ILVEN shares characteristics with psoriasis.3 Lesions extend deeper in ILVEN (reaching as far as the middle dermis) than in epidermal nevus and inflammatory changes are prominent findings. Histologically, epidermal nevi display acanthosis, papillomatosis with elongated epidermal crests, and hyperkeratosis alternating with areas of orthokeratosis and parakeratosis. Other features such as epidermolytic hyperkeratosis and focal acantholytic dyskeratosis can sometimes be observed in epidermal nevus. ILVEN lesions, on the other hand, have an inflammatory infiltrate deposited in a band in the papillary dermis. Exocytosis of lymphocytes and neutrophils toward the spongiotic and papillomatous epidermis can also be observed.
Unlike epidermal nevi, ILVEN lesions are thought to originate in mechanisms that regulate inflammation; such pathogenesis would condition their response to therapy. Various treatments have been tried, generally with disappointing results. Topical or intralesional corticosteroids, topical calcipotriol, cryotherapy, dermabrasion, electrocoagulation, surgery, and laser therapies are the main approaches used.3,23 Pulsed dye laser therapy has been reported to lead to improvement in pruritus in single cases24,25; this outcome is probably attributable to the anti-inflammatory effect of that laser modality. CO2 laser treatments have been used to treat ILVEN lesions in several series.26,27 Michel and coworkers21 achieved good results with this modality in 3 of 5 patients with ILVEN, although the effects were less satisfactory than outcomes in noninflammatory nevi.
The response in our series overall was good or excellent in 80% of the cases, but 93% of patients with VEN had good or excellent results. That rate is somewhat higher than the rates reported for earlier series.7,12,17
We found that ILVEN cases were clearly more resistant to treatment: the outcome was good for only 2 of the 5 patients with this diagnosis. This observation is consistent with previous reports.12,21 A constraint on laser treatment of these nevi is their depth. We treated all patients similarly in our series, making passes with the beam until the lesions were seen to have vaporized and eliminating tissue only to the level of the superficial dermis so as to avoid scarring. Ablation was generally inadequate in ILVEN cases and thus results were poor. The patients nonetheless reported great improvement in pruritus.
We did not see a clear relationship between therapeutic response and the thickness of epidermal nevi (hyperkeratosis), as results were excellent in some highly verrucous nevi. This finding contrasts with earlier reports that the degree of hyperkeratosis is a limiting factor.7,18 Differences in success may be attributable to the lack of fixed parameters in this type of treatment, in which the operator makes real-time procedural decisions about the optimal depth at which to destroy a lesion. Consistent with other published reports,19 we did observe that response was better when nevi were located on the face or neck. We can also report that response was better when the nevi covered an area less than 20cm2.
All patients were followed long-term (for periods ranging from 18 to 96 months) in order to detect recurrences, as these nevi have been known to reappear months or years after treatment. The overall rate of recurrence was 30% in our series, although if ILVEN cases are excluded the rate was 20%.
Patients expressed high satisfaction with treatment: 17 of the 20 patients were satisfied or very satisfied. Overall satisfaction was high with regard to improved appearance, and the treatments were well tolerated. This finding for satisfaction must be understood in the context of the lack of other clearly effective modalities that achieve good cosmetic results.
The inclusion of patients with ILVEN might have biased the results in this series. The pathogenesis of ILVEN and the histologic features of these nevi are different from those of other epidermal nevi, and these differences affect both treatment choice and degree of response.
We think that CO2 laser therapy is the treatment of choice for cases of epidermal nevus, as it is safe, well tolerated and effective over the long-term. Outcomes are superior for CO2 laser therapy in comparison with other laser modalities, although the risk of scarring is higher. The operator must decide when to end a CO2 laser procedure, as no fixed criteria have been established. Thus, operator experience is a highly relevant variable. The safety margin for treating ILVEN lesions is narrow. If treatment is inadequate, they will recur. If the operator goes too deep, unsightly scarring will develop. The principle limitation of this modality is that treating very extensive lesions will require scheduling several sessions. No safe, noninvasive alternatives are currently available for ILVEN, however, even though firm proof of the efficacy of laser therapy for these lesions is limited at this time. CO2 laser therapy, therefore, might be a good option to consider in certain cases or it might be useful as a palliative treatment to attenuate symptoms. We believe it is essential to have information about the experiences of various centers with large series of patients in order to perfect the way the procedure is carried out and to optimize our treatment of these nevi.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Alonso-Castro L, et al. Nevos epidérmicos tratados con láser de CO2: respuesta y seguimiento a largo plazo. Actas Dermosifiliogr. 2012;103:910–8.