The patient was an 82-year-old woman with a 30-year history of rheumatoid arthritis and dyslipidemia. On both lower limbs she presented painless, movable nodules along the length of the limb that had been present for 2 months. She described the nodules as “moving lentils”. There was no history of trauma, but the patient associated the condition with the use of strong compression stockings.
Physical ExaminationOn physical examination, 8 to 10 subcutaneous nodules of 0.5cm in diameter were palpable on each leg. The nodules were hard, well-defined, and could be rolled between the fingers; they could be easily moved between the skin and deeper planes and their movement was not limited to the trajectory of blood vessels (Fig. 1).
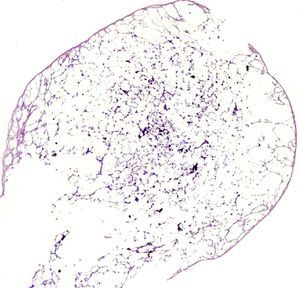
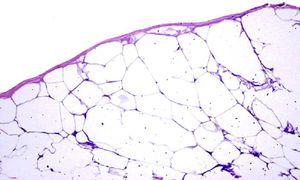
HistopathologyMacroscopic examination revealed a solid, hard, yellowish spherical nodule of 0.4cm in diameter, with a pearly appearance. Histologic examination showed fat lobules composed of necrotic adipocytes lacking nuclei and surrounded by a fibrous capsule (Figs. 2 and 3).
Additional TestsBlood analysis revealed hyperlipidemia, elevated creatinine levels, and mild leukocytosis, with no other abnormalities. Soft tissue ultrasound revealed small areas of edema in the subcutaneous cellular tissue, with no other relevant findings.
What Is Your Diagnosis?
DiagnosisEncapsulated fat necrosis.
Clinical Course and TreatmentIt was decided to maintain the patient under observation and, after 1 year of follow-up, the condition remained stable, with no new lesions detected.
CommentEncapsulated fat necrosis was first described in 1977 by Przyjemski and Schuster,1 and since then about 53 cases have been reported in the literature.2 This condition is known by many different names, including mobile encapsulated lipoma, nodular-cystic fat necrosis, and encapsulated fat necrosis.3
This dermatosis has been described in middle-aged women and in young men, particularly in athletes (skiers, etc), and predominantly affects the lower limbs.2 In some cases it has been detected on the upper limbs and hips. The condition usually presents as solitary or multiple subcutaneous nodules, ranging in size from 2 to 35mm. Cases associated with Ehlers-Danlos syndrome4 and erythema nodosum,5 among other conditions, have been described.
Histopathologically, the nodules consist of degenerated or necrotic adipose tissue surrounded by a fibrous capsule composed of several layers of connective tissue. In some cases there may be foci of calcification, fibrous septa within the lesion, and lipomembranous changes.
The most widely accepted hypothesis is that this condition is caused by trauma that decreases blood supply to a fat lobule, resulting in ischemic infarction and subsequent ischemic necrosis of the tissue. A fibrous capsule then forms around the necrotic tissue, creating a cleavage plane that separates it from the surrounding tissue and allows it to move freely throughout the subcutaneous cellular tissue. Because these lesions lack blood supply, they cannot be reabsorbed and persist as encapsulated remnants of necrotic adipose tissue.
The clinical differential diagnosis mainly includes soft tissue tumors, phleboliths, rheumatoid nodules, gout, calcinosis cutis, amyloidoma, and foreign body reaction. The histopathological differential diagnosis primarily includes traumatic panniculitis, lipomas and angiolipomas, pancreatic fat necrosis, and panniculitis due to α1-antitrypsin deficiency.
This condition is probably more common than reported. Similar lesions have been described as errant bodies in a submuscular plane, in the pericardium, and in the abdominal cavity.6
In conclusion, we present a striking case of multiple lesions of encapsulated fat necrosis, primarily characterized by their mobility.
Please cite this article as: Burgués M, et al. Nódulos desplazables en las piernas. Actas Dermosifiliogr. 2012;103:923–4.