The scalp is a relatively common site for skin tumors. The lack of cutaneous elasticity and the high frequency of actinic damage can limit the choice of reconstruction techniques, particularly in medium-sized or large defects. One of the most widely used flaps is the double hatchet flap, which is a good option with excellent cosmetic results.
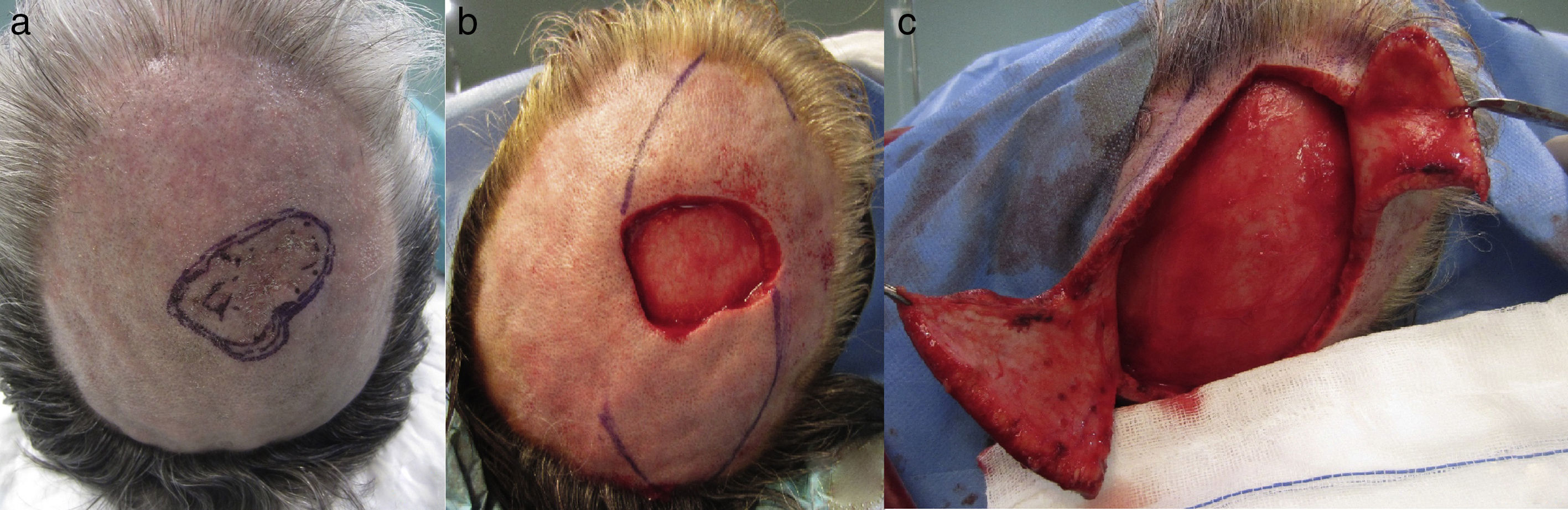
We present the case of a 62-year-old patient with a past history of hypertension and diabetes mellitus. He was referred to our outpatient clinic for a basal cell carcinoma measuring 3.4×3.5cm in the right parietal region (Fig. 1A). After histological confirmation by biopsy, surgical excision under local anesthesia and sedation was scheduled.
The resulting surgical defect measured approximately 4.2×5.7cm; the periosteum was intact. A bilateral hatchet flap was designed (Fig. 1B); the length of each flap was 1.5 times the diameter of the defect and the pedicle was a third of the length of the flap. Dissection was performed in the subgaleal plane (Fig. 1C), and the defect was closed by tissue planes, with placement of a drain posteriorly (Fig. 2A). The drain was removed the following day. The cosmetic result was excellent, with a minimal residual scar (Fig. 2B), and there were no signs of recurrence after a year of follow-up.
Tumors are not uncommon on the scalp, and can sometimes be large lesions that require laborious surgical techniques.
The options for reconstruction include closure by second-intention, which is possible when the periosteum is preserved.1,2 This is an acceptable option in small defects and in patients of advanced age or with comorbidities, although healing time is prolonged and the scar is depressed and alopecic. Another possibility is a graft, which usually achieves a poorer cosmetic result than a plasty, and leaves an area of alopecia.
Several flaps may be considered. Advancement, rotation, and transposition flaps are usually good options in defects that require special anatomical modifications. Specifically, advancement and transposition plasties are used less frequently, although they may be considered to be an option for reconstruction, depending on the size and site of the defect. The anatomical convexity makes rotation flaps and combined rotation-advancement flaps the most useful alternatives. These include the double hatchet flap and the O-Z flap, which is widely used for the reconstruction of scalp defects.
Free vascularized flaps are technically more complex and require hospital admission. Also, they are more expensive in the short and medium term.
It must be noted that when the defect includes the periosteum, leaving the cortical or even spongy bone exposed, the only reconstructive options are local plasties and free vascularized flaps, as a graft in this situation would have no vascular bed from which to draw nutrients and establish its blood supply, and would thus be lost.
The double hatchet flap, first described by Emmet in 1977, is a particularly useful option for the reconstruction of small and medium-sized scalp defects.1,3 It is a triangular plasty with a random vascular pattern that allows a double movement of rotation and advancement, facilitated by a tension-releasing design at its base, enabling closure of larger-diameter defects.3 This procedure can be performed in a single operation, on an ambulatory basis under local anesthesia, except for large defects that may require sedation and a short hospital admission.3
When designing the flap, the reference measurement after the circular excision of a lesion is the diameter of the defect; the length of the flap must be 1.5 times the diameter of the defect and the vascular pedicle must be at least a third of the length of the flap. Dissection is performed in the subgaleal plane, which will provoke less hemorrhage and preserve the supragaleal vascular bed. The disadvantage of this plane of dissection is the limited elasticity of the tissue, requiring broader release to achieve greater mobility of the plasty and thus distribute the tension across the surgical wound, avoiding complications such as dehiscence. Closure is performed by tissue planes, with a V-Y suture.
Close follow-up is required in the immediate postoperative period, with regular wound care.
The cosmetic result of the double hatchet flap can be excellent, as tissue of similar characteristics is used, with preservation of hair, texture, and thickness,3 rapid healing, and minimal scarring and comorbidity. Possible complications include flap necrosis, dehiscence, and the formation of hypertrophic scars.1,2,4,5
For all these reasons, the double hatchet flap is one of the best techniques for its simplicity of design, speed of performance, ease of postoperative care, and excellent result in the medium and long term.5
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Varela-Veiga A, Suárez-Magdalena O, Suárez-Amor Ó, Monteagudo B. Reconstrucción de defecto en cuero cabelludo mediante doble colgajo en hacha. Actas Dermosifiliogr. 2017;108:878–880.