Linear immunoglobulin (Ig) A dermatosis (LAD) is a rare autoimmune bullous disease characterized by the formation of subepidermal blisters with linear deposits of IgA along the basement membrane, visible on direct immunofluorescence.1–3 Cases of LAD mimicking other blistering diseases, such as bullous pemphigoid, pemphigus vulgaris, dermatitis herpetiformis, and impetigo, and nonbullous diseases have been reported.4,5
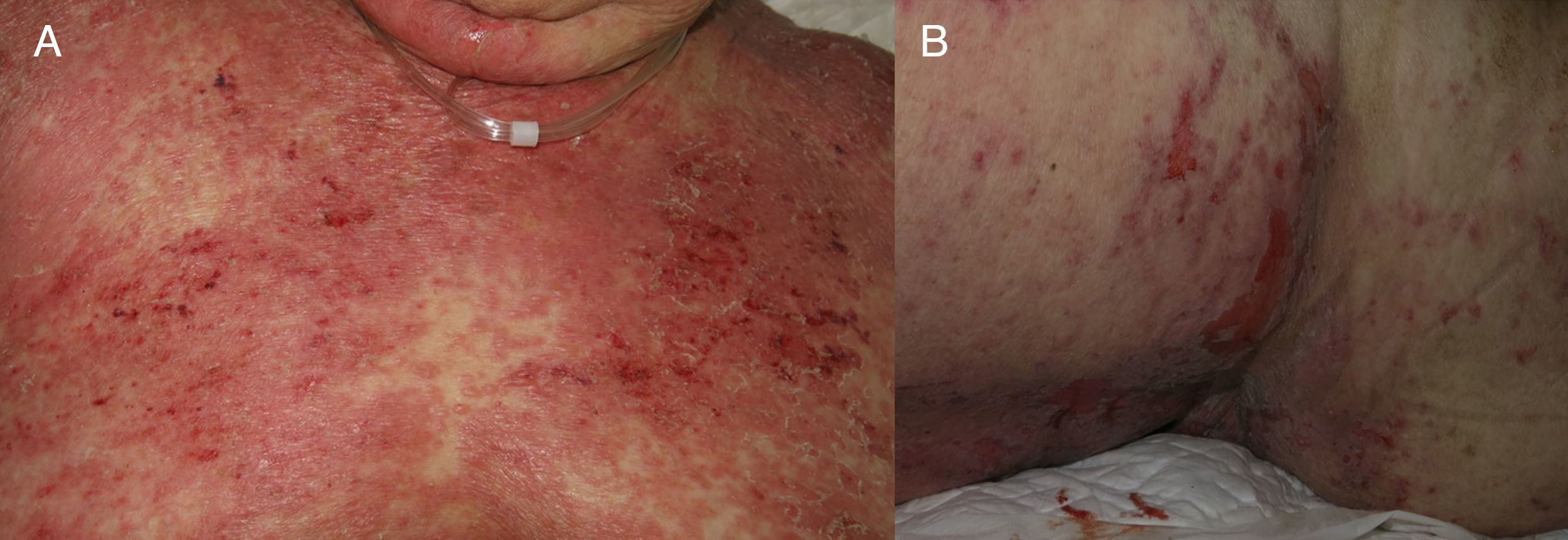
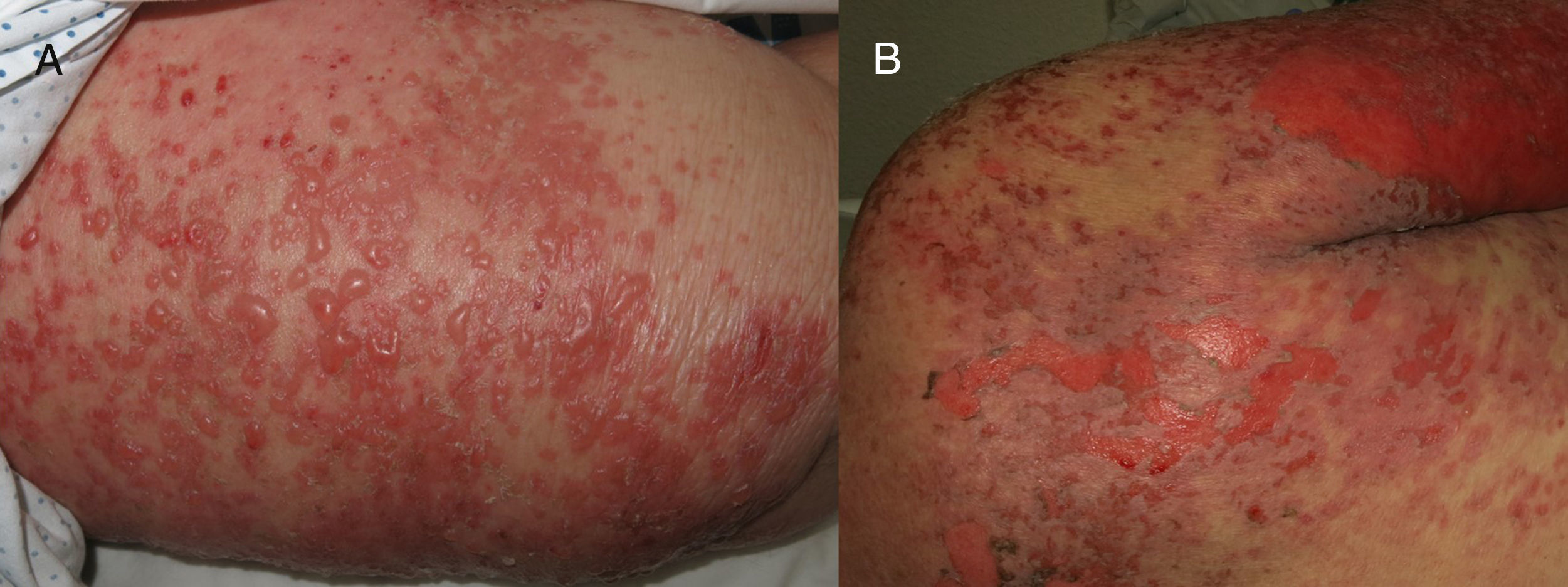
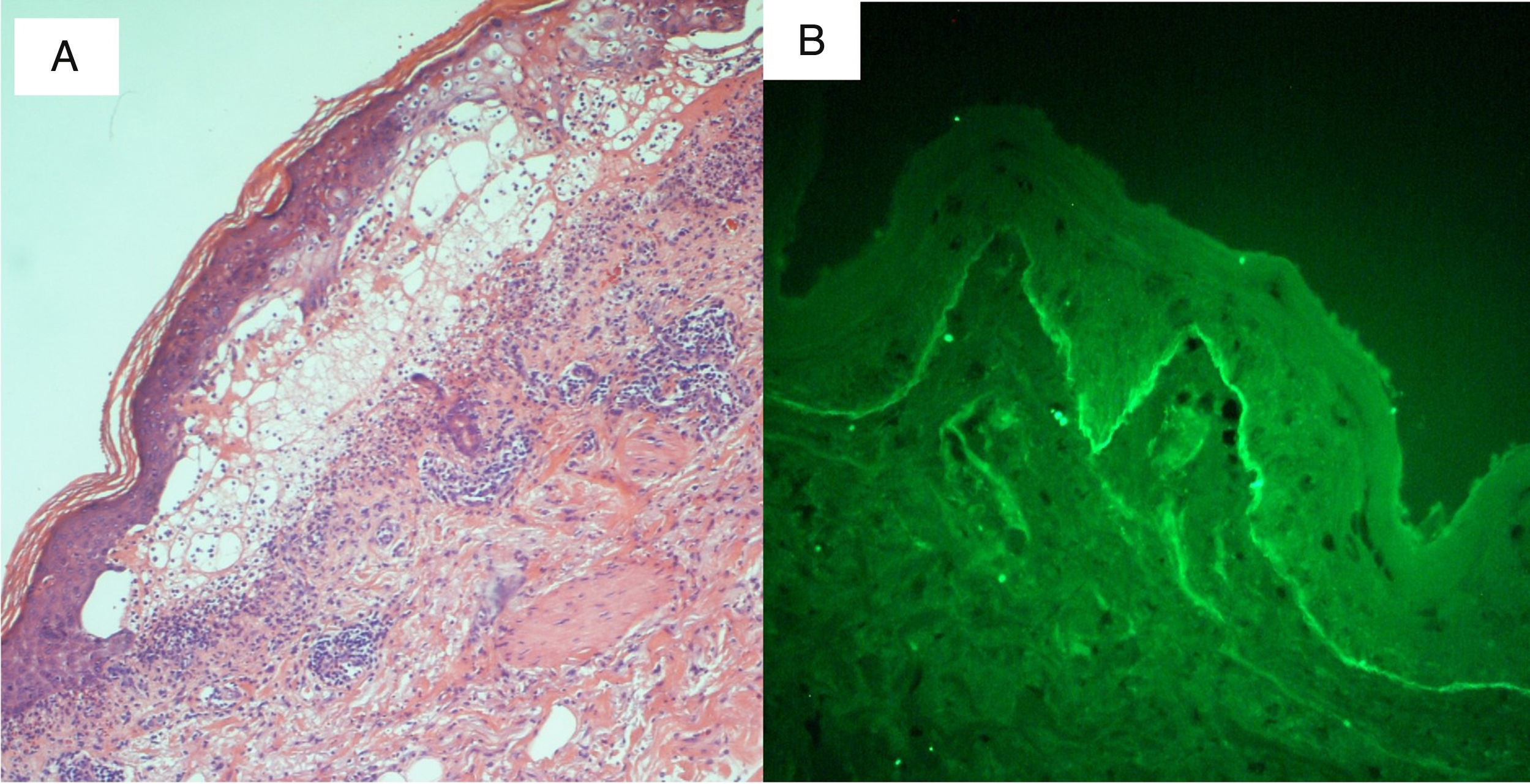
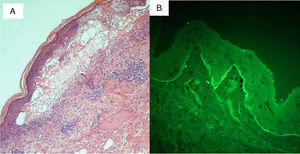
We present the case of an 88-year-old woman receiving palliative care for metastatic squamous cell carcinoma of the vulva. She was admitted to internal medicine for cellulitis of the right lower limb, for which the portal of entry was an ulcer in the right inguinal region. Computed tomography revealed a right inguinal fluid collection of 11cm in diameter, with gas, and osteomyelitis of the pubis that required urgent surgical debridement. The patient developed sepsis and treatment was started with ertapenem and vancomycin. Five days later, the dermatology department was consulted for the appearance of widespread desquamating erythematous lesions on the face, trunk, and limbs (Fig. 1A). Despite withdrawal of the vancomycin for suspected toxic epidermal necrolysis (TEN), LAD, or other drug-related hypersensitivity syndromes, the condition progressed to erythroderma in the space of 24hours, with tense blisters, erosions, and epidermal separation in pressure areas (Figs. 1B and 2A), with involvement of the oral mucosa, but not of other mucosas. In view of the patient's basal situation, she was not a candidate for transfer to a specialist burns unit. Treatment was started with systemic corticosteroids and, given the lack of response, it was decided to administer immunoglobulins at a dose of 0.4g/kg/d for 5 days. However, the condition progressed to widespread epidermal detachment (Fig. 2B) and the patient died 7 days later. Skin biopsy (Fig. 3A) revealed an epidermis with a normal maturation gradient and subepidermal vesicles full of a fibrinoid material with polymorphonuclear cells and eosinophils; these findings were consistent with a diagnosis of LAD. The superficial dermis showed a mild perivascular lymphocytic and eosinophilic inflammatory infiltrate. On direct immunofluorescence (Fig. 3B), a linear deposit of IgA was visible along the dermoepidermal junction, with no other pathological deposits with the antisera tested (fibrinogen, IgG, IgM, and complement component C3). Indirect immunofluorescence on 1M sodium chloride-separated skin, showed the deposits to be on the epidermal side of the vesicles.
The first descriptions of LAD are attributed to Bowen in 1901, although it was not until 1979 when it was considered a separate entity from dermatitis herpetiformis.5 LAD is a clinically and histologically heterogeneous condition that includes disorders with distinct clinical courses and whose diagnostic criteria continue under discussion.6 There are 2 main forms. The infantile form of LAD is characterized by erythematous plaques with tense peripheral blisters with the string of pearls sign; this form preferentially affects the trunk, perineum, and perioral region. Although the clinical course is variable, infantile LAD tends to resolve spontaneously before puberty.1,3 The adult form is much more variable and is sometimes considered to mimic other diseases.
A number of antigens have been reported to be implicated in the etiology of LAD, most importantly BP180, BP230, LAD1, and LAD97 localized on the epidermal side on indirect immunofluorescence of separated skin, and collagen VII, localized on the dermal side2,4,7; it is this diversity of antigens that is thought to explain the clinical heterogeneity of the disease.7 Drug-induced and idiopathic forms are traditionally recognized. The drug-related form, occurring most commonly with vancomycin, followed by phenytoin,4,8,9 develops between 1 and 30 days after starting treatment. The possibility of a tumor-related form (particularly with hematologic tumors) has also been suggested. The form similar to TEN is perhaps the most striking mode of clinical presentation of LAD, as it is most commonly associated with erythroderma, a positive Nikolsky sign, and palmoplantar and mucosal involvement; vancomycin also the most frequently implicated drug.7
The treatment of choice is dapsone, though corticosteroids, azathioprine, methotrexate, ciclosporin, and immunoglobulins are occasionally used.2,3,10 The treatment of LAD that presents as TEN is no different from that of other forms of LAD, although the greater extension and severity of the skin lesions requires greater attention to physical measures. Withdrawal of the suspected drug, when there is one, is the first and sometimes only step. On other occasions it is necessary to resort to systemic corticosteroids. The prognosis will also depend on the patient's basal situation and comorbid conditions.2,3,7 The use of immunoglobulins in LAD, as in other blistering diseases,10 is reserved for severe and refractory cases.
In summary, LAD is a heterogeneous entity that, among its numerous forms of presentation, can mimic TEN.4,5,7,9 It is important to include LAD in the differential diagnosis of vesiculobullous dermatoses and of TEN, making it advisable routinely to perform not only histological study in these cases but also immunofluorescence.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ruiz-Rivero J, Hernández-Aragüés I, Pulido-Pérez A, Suárez-Fernández R. Dermatosis ampollosa IgA lineal con presentación clínica de necrólisis epidérmica tóxica. Actas Dermosifiliogr. 2017;108:880–882.