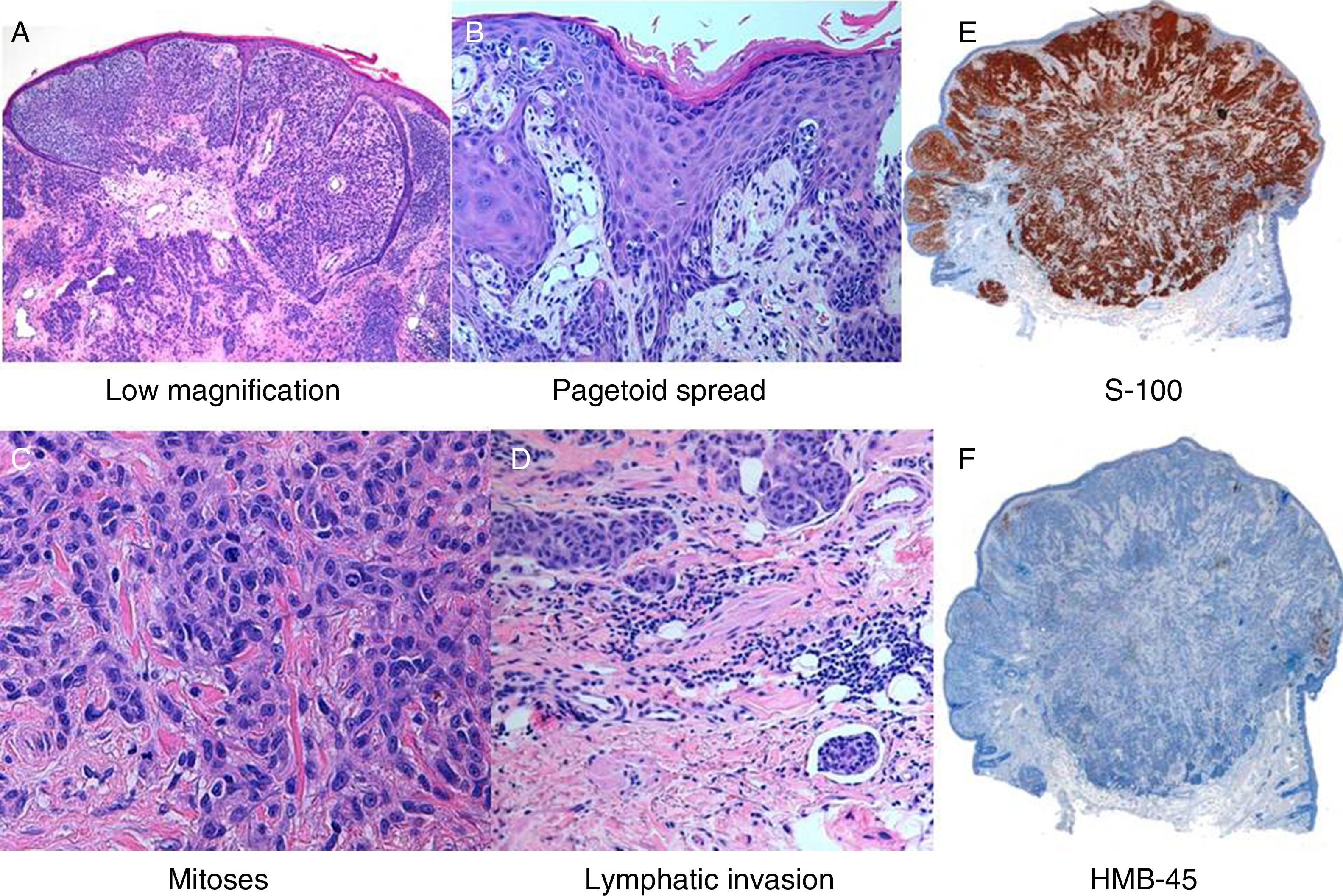
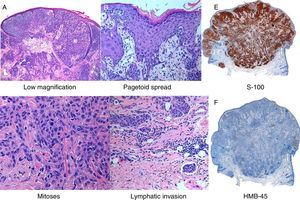
A 50-year-old man, skin phototype iii, with no past medical history of interest and with no personal or family history of melanoma, was seen in dermatology outpatients for a lesion that had arisen a year earlier on the auricle of his right ear. After treatment with salicylic acid as if it were a wart, the lesion initially disappeared, but subsequently returned. Dermatologic examination revealed an erythematous nodular lesion measuring 0.5cm in diameter on the lower third of the auricle of the right ear (Fig. 1). Dermoscopy did not suggest a melanocytic lesion, and there were no palpable regional cervical lymph nodes. The lesion was excised and histopathology reported a well-defined polypoid lesion that, at low magnification, appeared to be a benign lesion; however, at higher magnification, a melanocytic lesion with cytologic atypia and mitoses was observed, with a lack of deep maturation. Pagetoid spread and lymphatic invasion were also observed (Fig. 2). Immunohistochemistry was positive for S100 and melan A and negative for HMB45 and p16, and a high Ki-67 cell proliferation index was also observed (Fig. 2).
Based on these findings, the patient was diagnosed with nevoid melanoma of 0.7cm diameter, Clark level v and a Breslow thickness of 6.11mm, with up to 3 mitoses per mm.2 No ulceration, lymphocytic response, signs of regression, or perineural invasion were present.
Positron emission tomography-computed tomography was performed, showing no viable tumor tissue with affinity for 18F-FDG. Widening of the surgical margins to 2cm and selective sentinel lymph node biopsy (SLNB) were performed. After widening, the margins were free of tumor and the SLNB was negative. The patient was therefore diagnosed with melanoma stage T4b, N0, M0.
Nevoid melanoma, described by Schmoeckel et al.1 in 1985, is a lesion with characteristics similar to a benign nevus (symmetrical, dome-shaped lesion with cells that apparently mature). The main differential diagnosis is with intradermal melanocytic nevus (IDMN), and up to 50% of cases are referred for a suspected benign lesion.2 Histologically, nevoid melanoma is differentiated from IDMN because IDMN does not present cytologic atypia, mitoses, pagetoid spread, lymphovascular invasion, or lack of deep maturation. Immunohistochemistry is very similar and cannot be used to differentiate between these 2 diseases. HMB-45 is positive in 80% to 86% of melanomas, but was negative in our patient. Loss of p16, as was found in our patient, correlates with aggressiveness and metastases.3
Regarding malignant lesions, nodular melanoma is a densely cellular, nodular tumor, with intense cytologic atypia, mitoses, and an absence of the radial growth phase. Signs of IDMN are almost always present in melanoma on nevus, and immunohistochemistry can help in such cases, as the expression of HMB-45 and Ki-67, which characterize the superficial region of IDMN, is lost in nevoid melanoma.
In minimal deviation melanoma, cell organization in the dermis facilitates differentiation, as the growth pattern is expansive and displaces adjacent structures, and remnants of the preexisting nevus, whether a Spitz nevus, congenital nevus, or blue nevus, almost always persist.3,4
Nevoid melanoma is very rare, accounting for between 0.5%5 and 2.3% of cases. It is more common in men, with a mean age at presentation of 57 years, and tends to arise on the back and limbs.6 The largest series, with 43 patients, was published in 2015 by Idriss et al.7 Those authors described 2 architectural patterns (plaque and polypoid) and stated that 81% of cases of nevoid melanoma presented nests arranged in a parallel theque pattern in the basal layer of the tumor, which could aid diagnosis. Genetic techniques including fluorescent in situ hybridization and comparative genomic hybridization (CGH) have been shown to be useful in the differentiation between melanoma and melanocytic nevus. In that study, CGH detected genetic changes in 7 of the 8 cases in which the test was performed.
Nevoid melanomas appear to carry a poorer prognosis than other types described in the different series, with metastasis rates of 15% to 37.5% and a mortality of between 25% and 37.5% (series by Schmoeckel et al.1 and series by Idriss et al.7). In our patient, SLNB was performed despite the site being on the head and neck, which can make the technique more difficult, and, in accordance with the melanoma committee, local radiotherapy was administered.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernándezirenebsf@hotmail.com IS, Sanz MMS, Botello LN, Gullón GR. No es bueno todo lo que lo parece. Actas Dermosifiliogr. 2017;108:876–878.