Basal cell carcinoma (BCC) is the most common skin cancer in the general population. BCC is managed in a variety of ways, and available international guidelines are difficult to put into practice in Spain. This guideline aims to improve the management of BCC based on current evidence and provide a point of reference for Spanish dermatologists.
Material and methodsMembers of the Spanish Oncologic Dermatology and Surgery Group (GEDOC) with experience treating BCC were invited to participate in drafting this guideline. The drafters used the ADAPTE collaboration process to develop the new guideline based on existing ones, first summarizing the care pathway and posing relevant clinical questions. They then searched for guidelines, assessed them with the AGREE II (Appraisal of Guidelines for Research and Evaluation) tool, and searched the selected guidelines for answers to the clinical questions. Finally, the recommendations were drafted and submitted for external review.
ResultsThe highest-scoring guidelines were from the Association of Dermatologists, the National Comprehensive Cancer Network, the European Dermatology Forum, and the European Academy of Dermatology and Venereology. A total of 11 clinical questions were answered.
ConclusionsThis new guideline answers the working group's clinical questions about the routine management of BCC in Spain. It provides dermatologists with a tool they can use for decision-making while taking into consideration the resources available and patient preferences.
El carcinoma basocelular supone el cáncer de piel más frecuente en la población. Hay una gran variabilidad en su manejo y las diferentes guías extranjeras que existen son difícilmente aplicables en nuestro medio. El objetivo de la presente guía es servir de referencia a los dermatólogos españoles para mejorar el manejo de este tumor basándose en la evidencia actual.
Materiales y métodosSe escogió a miembros del Grupo Español de Dermato-Oncología y Cirugía (GEDOC) con experiencia en el tratamiento de estos tumores y con interés en participar en la elaboración de la guía. Se hizo una adaptación de las guías de práctica clínica existentes mediante el método ADAPTE, se resumió el proceso de atención, y se elaboraron las preguntas clínicas relevantes. Se seleccionaron las guías mejor puntuadas mediante el instrumento AGREE II, realizando la búsqueda de las respuestas en dichas guías y elaborando posteriormente las recomendaciones. Finalmente se sometió la guía a revisión externa.
ResultadosLas guías con mejor puntuación fueron las de la British Association of Dermatologits (BAD), del National Comprehensive Cancer Network (NCCN), del European Dermatology Forum (EDF) y de la European Academy of Dermatology and Venereology (EADV). Se obtuvieron en total 11 preguntas clínicas, contestadas a partir de estas guías.
ConclusionesEsta guía responde a preguntas habituales sobre el manejo del carcinoma basocelular en la práctica clínica diaria y sirve a los dermatólogos como referencia en la toma de decisiones, siempre teniendo en cuenta los recursos y las preferencias del paciente.
Skin cancer is a frequent disease in our setting. The incidence of basal cell carcinoma is 253.23 tumors (95% CI, 273.01–69.45) per 100 000 person-years, and this may be increasing.1 Basal cell carcinoma accounts for 80%–90% of all cases of skin cancer and is the most frequently occurring form of cancer in humans. It has major repercussions for quality of life in terms of functional and cosmetic morbidity and generates a considerable burden for dermatologists and the health system.2 Basal cell carcinoma can be treated using many approaches, some are which are new. Treatments vary in clinical practice and differ widely in terms of cost depending on the option selected. Consequently, clinical decision making becomes more complex.
While clinical practice guidelines (CPGs) for management of basal cell carcinoma are available, they apply to different settings and only partially cover the problems dermatologists consider to be the most relevant.
Therefore, the Healthy Skin Foundation of the Spanish Academy of Dermatology and Venereology (Fundación Piel Sana de la Academia Española de Dermatología y Venereología [AEDV]) has promoted the adaptation of CPGs for the main skin tumors, which now form part of the AEDV White Paper on Skin Cancer (Libro Blanco del Cáncer Cutáneo).
The objective of these guidelines is to adapt a series of recommendations to our setting. The recommendations are based on the best evidence possible for decision making in the management of patients with basal cell carcinoma.
Material and MethodsAs CPGs were already available, we decided to adapt these using the ADAPTE method. The steps followed during this process are summarized in the Supplementary Material (Supplementary Material, Section 1).3,4
The panels were selected based on the experience in treating these tumors and on interest in participating in the CPGs among the Members of the Spanish Oncologic Dermatology and Surgery Group (Grupo Español de Dermato-Oncología y Cirugía [GEDOC]) of the AEDV. All of the panelists declared their conflicts of interest before participating.
The scope and objectives statement established the objective of the guidelines as that of providing indications on controversial aspects of diagnosis, treatment (medical and surgical), and patient follow-up (Supplementary Material, Section 2). The care setting for the CPGs is that of dermatology departments in Spain, with dermatologists as the target users. Prevention of basal cell carcinoma and patients with multiple tumor syndromes were excluded from the scope of the CPGs.
Following the ADAPTE method, the subsequent steps involved a summary of the care process and formulation of relevant clinical questions for each step of the algorithm (Supplementary Material, Section 3). The most relevant questions were selected based on consensus at a face-to-face meeting at the head office of the AEDV in October 2016. In parallel, guidelines were sought on web pages or in specific organizations and sources, as well as in bodies that collect, prepare, or publish guidelines. We also included the main academies of dermatology or cancer (eg, National Guidelines Clearinghouse, Guidelines International Network, Guiasalud, Institute for Clinical Systems Improvement, National Institute for Health and Care Excellence, New Zealand Guidelines Group, Scottish Intercollegiate Guidelines Network, Cochrane Library, British Association of Dermatologists, American Academy of Dermatology, European Academy of Dermatology and Venereology, National Comprehensive Cancer Network). The guidelines were subsequently reviewed and evaluated for their methodological quality using the Appraisal of Guidelines for Research and Evaluation (AGREE) II tool.5 The CPGs with the most favorable results were selected for consultation.
This information was used to generate the recommendations, which maintained the reference to the original source. Retrievals, the level of evidence, and the grade of recommendation based on the levels of Oxford Centre for Evidence-Based Medicine were always established in pairs.6
Once the draft version was complete, the recommendations were published on the web page of the AEDV (https://aedv.es/revision-de-las-recomendaciones-de-la-gpc-basocelular/) and underwent external review. A review was requested from all those with an interest in the topic from the AEDV, GEDOC, and pharmaceutical industry, as well as from oncologists. The members of the panel evaluated the reviewers’ objections, and, if these were considered relevant, they were applied to the CPGs.
ResultsThe 4 highest-scoring guidelines whose objectives were consistent with the scope and objectives proposed were as follows: British Association of Dermatologists, National Comprehensive Cancer Network, European Dermatology Forum, and the European Academy of Dermatology and Venereology. Despite their high scores in terms of quality, the guidelines of the Agency for Healthcare Research and Quality and those of the National Institute for Health and Care Excellence were excluded because they were aimed at primary care and other specialists and did not address the questions proposed.
The clinical questions proposed and the recommendations of the CPGs are set out below. The complete document of the CPGs, which includes a discussion of each question, is available as supplementary material (Supplementary Material, Section 4).
Section 1. Second Intervention vs Observation in Basal Cell Carcinoma With Positive MarginsQuestion 1. In the case of patients with basal cell carcinoma with positive margins, does a second intervention reduce the probability of recurrence compared with observation?
Summary of EvidenceInvolvement of surgical margins is associated with a higher rate of recurrence after surgery, especially in tumors that affect the center of the face, high-risk histologic subtypes (morpheaform, micronodular, infiltrative), and when the positive margin is deep (Level of evidence, 2a).7–14
RecommendationsIncompletely excised basal cell carcinomas should be retreated, especially if the center of the face is involved, the deep margin is affected, local flaps or grafts have been used to close the surgical wound, or the histologic subtype is high-risk. The therapeutic approach of choice is standard surgery or Mohs micrographic surgery (especially if the abovementioned requisites are fulfilled). Similarly, clinical checkups could be considered in small nonaggressive tumors on the trunk (Grade of recommendation, B).
Section 2. Radiotherapy vs Second Intervention in Basal Cell Carcinoma With Positive MarginsQuestion 2. In patients with basal cell carcinoma and positive surgical margins, does adjuvant radiotherapy reduce the probability of recurrence compared with a second intervention?
Summary of EvidenceThere are no studies comparing second intervention with adjuvant radiotherapy in basal cell carcinoma with positive surgical margins. Guidelines recommend reintervention as the first option, with radiotherapy reserved for patients who are not candidates for surgery (contraindication, surgical problems, or patient refusal to undergo the procedure) (Level of evidence, 4).15–18
RecommendationsRadiotherapy should be reserved for patients with basal cell carcinoma and positive surgical margins who are not candidates for a second intervention (Grade of recommendation, C).
Section 3. Surgery vs Nonsurgical Treatment in Low-risk Basal Cell CarcinomaQuestion 3. In patients with low-risk basal cell carcinoma, does nonsurgical treatment affect the probability of recurrence compared with surgery?
Summary of EvidenceRecurrence rates are lower with conventional surgery than with nonsurgical approaches. Therefore, conservative treatment should be reserved for cases that are not candidates for surgery.19–21 Electrodessication and curettage may prove useful as treatment in low-risk basal cell carcinoma, with a lower percentage of persistence of the tumor in carcinomas on the trunk and extremities (Level of evidence, 4).22–26 Cryosurgery may also be a good therapeutic option in low-risk basal cell carcinoma (Level of evidence, 3b).27–33 CO2 laser ablation and curettage would be particularly indicated in low-risk basal cell carcinoma in the form of large or multiple tumors (Level of evidence, 4).34 Imiquimod is useful in low-risk basal cell carcinoma, mainly in superficial tumors, and, to a lesser extent, in nodular tumors (Level of evidence, 1b).35,36 Photodynamic therapy is also useful in superficial basal cell carcinoma, with a higher recurrence rate in nodular basal cell carcinoma (Level of evidence, 1b).37–42 5-Fluorouracil could be an option for treatment, although there is insufficient evidence to support its use (Level of evidence, 4).
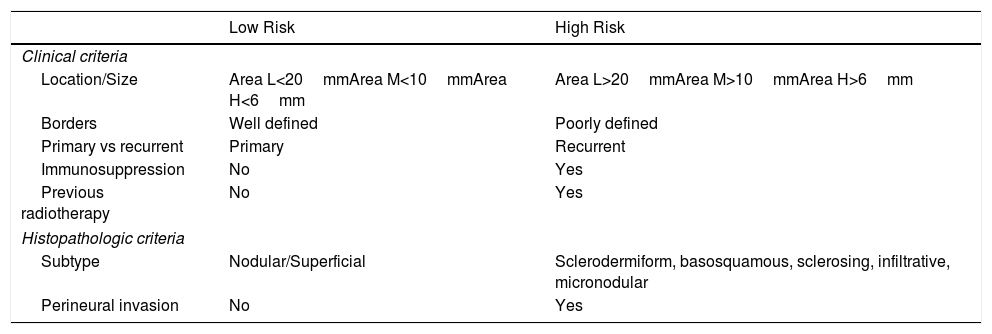
RecommendationsNonsurgical approaches are a good option for the management of low-risk basal cell carcinoma when surgery is not possible (see Table 1 for a summary of risk factors). Electrodessication and curettage is useful in low-risk tumors, especially when these are located on the trunk and extremities (Grade of recommendation, C). Cryosurgery can also be used in low-risk basal cell carcinoma (Grade of recommendation, B). Laser and curettage can be used to treat large or multiple tumors (Grade of recommendation, C). Imiquimod is a good option for superficial basal cell carcinoma (Grade of recommendation, A) and may prove useful in nodular tumors (Grade of recommendation, C). Photodynamic therapy is also useful in superficial basal cell carcinoma (Grade of recommendation, A) and, to a lesser extent, in nodular tumors (Grade of recommendation, B). 5-Fluorouracil could also prove useful in the treatment of low-risk basal cell carcinoma (Grade of recommendation, C).
Risk Factors.
| Low Risk | High Risk | |
|---|---|---|
| Clinical criteria | ||
| Location/Size | Area L<20mmArea M<10mmArea H<6mm | Area L>20mmArea M>10mmArea H>6mm |
| Borders | Well defined | Poorly defined |
| Primary vs recurrent | Primary | Recurrent |
| Immunosuppression | No | Yes |
| Previous radiotherapy | No | Yes |
| Histopathologic criteria | ||
| Subtype | Nodular/Superficial | Sclerodermiform, basosquamous, sclerosing, infiltrative, micronodular |
| Perineural invasion | No | Yes |
Area H: center of the face, eyelids, eyebrows, periorbital skin, nose, lips, chin, mandible, preauricular area, retroauricular area, pinna, temple, genitals, hands, and feet. Area L: trunk and extremities. Area M: cheeks, forehead, neck, scalp, and neck.
Question 4. In patients with high-risk basal cell carcinoma, does Mohs surgery reduce the probability of recurrence compared with conventional surgery?
Summary of EvidenceRecurrence rates for Mohs micrographic surgery are lower than for conventional surgery in recurrent tumors (Level of evidence, 1b). Data for primary tumors are not as clear. Mohs surgery is particularly indicated in high-risk tumors, especially those located on the face (Level of evidence, 1b).43–49
RecommendationsMohs micrographic surgery is the most appropriate treatment in high-risk basal cell carcinoma, especially those located on the face, and in recurrent tumors (Grade of recommendation, A).
Section 5. Risk Associated With ImmunosuppressionQuestion 5. In immunodepressed patients with low-risk basal cell carcinoma, does surgical treatment affect the probability of recurrence compared with nonsurgical treatment?
Summary of EvidenceThere are no conclusive data that allow us to state that basal cell carcinoma in immunodepressed patients is riskier than in immunocompetent patients. Similarly, there are no studies comparing surgical treatment with conservative treatment in these patients. However, in the guidelines of the British Association of Dermatology and the National Comprehensive Cancer Network, immunosuppression per se is considered an indicator of poor prognosis (Level of evidence, 5).50–52
RecommendationsBasal cell carcinoma may be more aggressive in immunodepressed patients. Therefore, surgery should always be the first option, and conservative treatments should be reserved for cases that are not candidates for surgery (Grade of recommendation, D).
Section 6. Vismodegib vs Radiotherapy in Locally Advanced Basal Cell CarcinomaQuestion 6. In patients with locally advanced basal cell carcinoma, does treatment with vismodegib improve overall survival or disease-free survival compared with radiotherapy?
Summary of EvidenceThere are no studies comparing vismodegib with radiotherapy for the treatment of locally advanced basal cell carcinoma with respect to survival outcomes (overall and disease-free). Clinical trials with vismodegib include patients with basal cell carcinoma who have already received radiotherapy or for whom radiotherapy was considered contraindicated or inappropriate (hypersensitivity to radiotherapy [eg, Gorlin syndrome], limitations arising from the location of the tumor, or cumulative doses of previous radiotherapy) (Level of evidence, 5).53–57
RecommendationsVismodegib is effective for the treatment of locally advanced or metastatic basal cell carcinoma. Its use is limited to those cases where the patient is not a candidate for surgery, whether because of inoperability, multiple recurrences, or expected surgical morbidity (severe disfigurement, functional defect, and/or cosmetic defect not tolerated by the patient) (Grade of recommendation, D).
Section 7. Vismodegib in Neoadjuvant TherapyQuestion 7. In patients with locally advanced basal cell carcinoma that is inoperable owing to the complexity of surgery, does neoadjuvant vismodegib enable surgical rescue or reduce the complexity of surgery sufficiently to enable a second intervention compared with radiotherapy?
Summary of EvidenceThere are no studies comparing vismodegib with radiotherapy in terms of reducing the complexity of surgery. Some studies suggest that vismodegib could be useful in neoadjuvant therapy by reducing the size of the tumor and enabling surgical rescue (Level of evidence, 4).58–60
RecommendationsIn cases of locally advanced basal cell carcinoma where it is difficult to treat the tumor with surgery, treatment with vismodegib for some months could reduce the size of the tumor and thus enable surgery (Grade of recommendation, C).
Section 8. Follow-up by Protocol or as Needed for Early Diagnosis of RecurrenceQuestion 8. In patients with high-risk basal cell carcinoma, does follow-up by protocol facilitate early diagnosis in cases of recurrence compared with follow-up as needed?
Summary of EvidenceThere are no studies comparing follow-up by protocol with follow-up as needed in patients with high-grade basal cell carcinoma. Similarly, no consensus has been reached on the frequency, periodicity, or total duration of follow-up. However, the different guidelines recommend long-term surveillance of these patients (especially in patients with recurrent, multiple, and high-risk lesions), with checkups every 6–12 months during the first 3–5 years. Checkups can subsequently be scheduled further apart if no other skin tumors appear during this period. Some guidelines recommend lifelong annual checkups as the ideal approach (Level of evidence, 5).61,62
RecommendationsIn patients with high-risk basal cell carcinoma or recurrent or multiple lesions, follow-up should be every 6–12 months for the first 3–5 years. Follow-up visits can subsequently be scheduled further apart (Grade of recommendation, D).
Section 9. Follow-up by Protocol vs Discharge and Follow-up as Needed in Low-risk Basal Cell CarcinomaQuestion 9. In patients with low-risk basal cell carcinoma, does follow-up by protocol facilitate early diagnosis in the case of recurrence compared with discharge and follow-up as needed?
Summary of EvidenceThere are no studies comparing follow-up by protocol with checkups as needed or annual checkups in patients with low-grade basal cell carcinoma. The risk of recurrence in patients with appropriately treated low-risk disease is reduced. However, patients with basal cell carcinoma have a greater risk of developing new skin tumors, and this risk is increased in the short term (Level of evidence: 2a). Therefore, the ideal situation would involve regular follow-up of all patients with basal cell carcinoma at least once per year (Level of evidence, 5).61–63,9
RecommendationsIt is recommended to arrange at least 1 follow-up visit in order to advise the patient on photoprotective measures, the nature of the tumor, and the risk of new lesions. If possible, patients with low-risk basal cell carcinoma should be followed up yearly (Grade of recommendation, D).
Section 10. Follow-up After Nonsurgical Techniques in Low-risk Basal Cell CarcinomaQuestion 10. In patients with low-risk basal cell carcinoma treated with nonsurgical techniques (electrodessication and curettage, cryosurgery, CO2 laser, imiquimod, photodynamic therapy, and 5-fluorouracil), does follow-up by protocol facilitate early diagnosis in the case of recurrence compared with consultation as needed by the patient?
Summary of EvidenceThere are no studies comparing follow-up by protocol with consultation as needed by the patient with respect to early diagnosis in the case of recurrence. It is important to remember that nonsurgical approaches are to be used mainly in low-risk basal cell carcinomas, although these therapeutic modalities are associated with greater recurrence rates than standard surgery (Level of evidence, 5).64,65
RecommendationsGiven the lack of sufficient evidence to support a follow-up protocol in these cases, we would extrapolate the follow-up recommendations for low-risk basal cell carcinoma (Grade of recommendation, D).
Section 11. Patient Follow-up for Detection of New CarcinomasQuestion 11. In patients previously diagnosed with basal cell carcinoma, does follow-up by protocol facilitate early diagnosis of new basal cell carcinomas compared with consultation requested by the patient?
Summary of EvidenceAll patients with basal cell carcinoma have a greater risk of developing new basal cell carcinomas, squamous cell carcinoma, and melanoma, and this risk is greater during the first 3–5 years (Level of evidence, 2a). The number of previous basal cell carcinomas is the best predictor of new basal cell carcinomas (Level of evidence, 1b). Therefore, some experts recommend periodic follow-up of all patients with basal cell carcinoma at least once per year (Level of evidence, 5).63,66–79
RecommendationsAt least 1 follow-up visit should be scheduled in order to advise the patient on photoprotective measures, explain the risk of developing new lesions, and highlight the importance of self-monitoring. If the health system allows, patients with basal cell carcinoma should be followed-up at least annually (Grade of recommendation, D).
DiscussionThe CPG we adapted based on other recent guidelines can aid decision making in the field of dermatology-oncology.
The main advantages of the present study were its rigorous and reproducible methodology, the fact that the findings were applied to our setting, and the external review by professionals from various disciplines before publication.
A limitation to the approach adopted here could be the fact that the panelists were all dermatologists. We followed this approach because the scope and objectives statement limited the CPGs to dermatology, the original CPGs are multidisciplinary, and the draft versions of the CPGs underwent multidisciplinary external review.
The recommendations will remain in force but must be reviewed during the next 3 years.
As with any guidelines, these recommendations are not mandatory but should be applied with some flexibility depending on local availability of resources, the physician's experience, and the patient's preferences.
FundingThe AEDV White Paper on Skin Cancer was fully funded by Fundación Piel Sana AEDV. Neither external companies nor the pharmaceutical industry played a role in its drafting (except for possible external review [Roche Pharma], as with other interested parties).
Conflicts of InterestA. Ruiz-de-Casas and P. Redondo-Bellón have given paid talks for Roche. I. Palacios-Álvarez has given paid talks for Roche and IFC. The remaining authors declare that they have no conflicts of interest.
The present guidelines form part of the White Paper on Skin Cancer of Fundación Piel Sana of the AEDV.
Please cite this article as: Vílchez-Márquez F, Borregón-Nofuentes P, Barchino-Ortiz L, Ruíz-de-Casas A, Palacios-Álvarez I, Soria-Rivas A, et al. Carcinoma basocelular cutáneo: diagnóstico y tratamiento en atención especializada dermatológica. Guía de Práctica Clínica de la AEDV. Actas Dermosifiliogr. 2020;111:291–299.