Patch tests are only indicated for hand eczema when it is diagnosed as chronic. A positive reaction of current relevance requires a change in treatment strategy. Knowing which clinical factors are associated with current relevance would allow tests to be performed sooner.
ObjectiveTo develop a model for predicting currently relevant patch test positivity in patients with hand eczema only.
Material and methodsRetrospective study of patients with hand eczema only. We collected data on age, sex, time since onset, occupation, and history of atopic dermatitis. We built a predictive logistic regression model and assessed discrimination by computing the area under the receiver operating characteristic curve.
ResultsWe included 262 patients; 66.03% had positive patch tests (28.6% of current relevance). Univariate analysis detected significant associations between positivity of current relevance and employment as a hairdresser-aesthetician, a personal history of atopy, male sex, and a time since onset of over 6 months. Multivariate analysis confirmed employment as a hairdresser-aesthetician as an independent risk factor and male sex and a personal history of atopy as protective factors. The score suggested by the predictive model was 2.316(hairdresser-aesthetician)−1.792(atopic dermatitis)−0.601(male sex).
ConclusionsOccupation, sex, and a history of atopy influence the likelihood of patch test positivity of current relevance in patients with hand eczema in Spain. Our model suggests that a diagnosis of chronic eczema is not necessarily an indication for patch testing. Future studies with larger samples are needed to determine the true usefulness of predictive models in this setting.
La única indicación para la realización de pruebas epicutáneas en eccema de manos es su cronicidad. La presencia de una relevancia presente en las mismas supone un cambio en el manejo del paciente. Sería interesante conocer qué factores clínicos se asocian a presentar relevancia presente para establecer la indicación de pruebas de forma más temprana.
ObjetivoObtener un modelo predictivo sobre relevancia presente en pruebas epicutáneas en pacientes con eccema exclusivo de manos.
Material y métodosSe realizó un estudio retrospectivo en pacientes con eccema exclusivo de manos. Las variables estudiadas fueron: edad, sexo, tiempo de evolución, profesión y antecedentes de dermatitis atópica. Se obtuvo un modelo predictivo mediante regresión logística y se valoró su poder de discriminación mediante el área bajo la curva ROC.
ResultadosSe incluyeron 262 pacientes. El 66,03% presentó pruebas positivas, con un 28,6% de relevancias presentes. Mostraron asociación en el análisis univariante profesión peluquería-esteticista, historia personal de atopia, sexo masculino y tiempo de evolución >6meses. Mantuvieron asociación independiente en el análisis multivariante profesión peluquería-esteticista (factor de riesgo), sexo masculino e historia personal de atopia (factores protectores). El modelo predictivo resultante fue Puntuación=2,316×(peluquería-esteticista)−1,792×(dermatitis atópica)−0,601×(sexo masculino).
ConclusionesEn nuestro ámbito, la profesión, el sexo y la historia de atopia han demostrado influir en la probabilidad de presentar positividades con relevancia presente en pacientes con dermatitis de manos. Según nuestro modelo, la cronicidad del cuadro no debe suponer una indicación de realización de pruebas epicutáneas. Son necesarios futuros estudios con mayor tamaño muestral para determinar la verdadera utilidad de los modelos predictivos en estos pacientes.
Hand eczema is caused by many factors. The point prevalence of hand eczema is approximately 4% in adults and the annual prevalence is around 10%.1–3 The frequency of contact allergy diagnosed on the basis of positive skin tests ranges from 23% to 62% in patients with hand eczema, while the rate of positive test results of current clinical relevance ranges from 20% to 25%.4,5 Guidelines based on expert opinion all recommend patch testing but do not specify when or under which circumstances they are indicated. The only established criterion is that the condition be chronic, defined by the presence of symptoms lasting for varying periods of time (4, 6, or 12 weeks) during which hand eczema remains poorly controlled even with appropriate treatment.1–6
Predictive models of prognosis or risk rely on a combination of factors with different degrees of association with an event, making it possible to calculate the likelihood that an individual will experience it.7 These models are useful for making clinical decisions about treatment and have been widely used in dermatology. An example is a model for scoring pigmented lesions during diagnosis.8
Because a positive patch test reaction to an allergen of current relevance indicates a need to warn a patient with hand eczema to avoid the substance implicated, these tests are extremely important for managing therapy. We have found no predictive models for hand eczema, or for contact eczema in general, that name a positive patch test reaction of current relevance as the outcome of interest.
ObjectiveWe aimed to develop a model to predict a positive patch test reaction to a substance of current clinical relevance for patients with eczema located only on the hands.
Material and methodsStudy designThis retrospective observational study included 262 patients with eczema only on the hands. Cases came from the database of the contact dermatitis unit of our hospital. Patients were treated and tested between February 2005 and November 2017. All underwent patch testing (True Test) using the Spanish standard series and complementary allergens9 along with additional batteries as needed according to clinical suspicion. We followed the guidelines of the European Society of Contact Dermatitis and read results at 48 and 96hours.10 Patients were classified according to presence or absence of positive test results of current clinical relevance, which was determined by medical history. The following variables were analyzed: age (years), sex (man or woman), patient history of atopic dermatitis (yes or no), current occupation, and time since onset of lesions (6 months or less or longer than 6 months). We recorded the patient's occupation at the time of testing, regardless of when employment had started, because it was the current relevance of positivity that was of interest. The cut-point of 6months (less than and more than) was chosen based on statistical criteria.
To test the model's predictive ability, cases were randomly assigned to 2 subgroups, a development sample consisting of two thirds of the patients and a validation sample consisting of the remaining one third.
To develop the model, variables were entered into the database as present (1) or absent (0).
All patient information was managed in accordance with current Spanish legislation on data protection (Law 41/2002 of November 14 and Law 15/1999 of December 15). The study was approved by the research ethics committee of our center (Complejo Hospitalario Universitario Insular – Materno Infantil) in Las Palmas de Gran Canaria, Spain.
Statistical analysisNormal distribution of data was checked with the Kolmogorov–Smirnov test. Categorical variables were reported as frequency and percentage and continuous ones as the mean (SD) or the median and interquartile range if not normally distributed. We compared percentages with the Pearson χ2 test or the Fisher exact test. Means were compared with the t test. The model to predict a positive patch test finding of current clinical relevance (the event) was developed with the data for a subgroup of 175 patients (training data set) and validated in another subgroup of 87 patients. The likelihood of the event was estimated using linear logistic regression analysis. Variables were previously selected by an algorithm that took into consideration all variables11 and the Akaike information criterion (AIC). This approach assumes that the optimal model is the one with the lowest AIC. The model thereby obtained was summarized by coefficients and their standard errors, AIC values resulting from eliminating variables, and odds ratios (OR) and their 95% CIs. The ability of the model to predict the event was assessed with the area under the receiver operating characteristic curve (AUC-ROC) in the validation data set. This curve and its 95% CI estimated the model's ability to discriminate between cases in which the event was present or absent. The optimum cut-point for prediction was the one that minimized the function, as follows: (1−sensitivity)2+(1−specificity)2. Finally, we calculated the sensitivity, specificity, and positive and negative predictive values and their 95% CIs for the resulting prediction rule. The null hypothesis was assessed at a level of statistical significance of P<.05. Data were analyzed using the R software package, version 3.3.1.12
ResultsTable 1 summarizes the main patient characteristics. We observed 467 patch test reactions in 262 patients. At least 1 positive result was observed in 66.03% of the patients. The allergens that provoked the largest numbers of reactions were nickel (89), combined methychlorolisothiazolinone/isothiazolinone (27), methylisothiazolinone (18), ethylene glycol dimethacrylate (18), and hydroxyethyl methacrylate (17). Positive reactions of current clinical relevance were found in 28.6%. The most common ones are summarized in Table 2, which shows that acrylates were clearly the most frequent culprits. Patient occupations are shown in Table 3.
Patient Characteristicsa
| With or Without a Reaction of Current Relevance | P | |||
|---|---|---|---|---|
| Total (%) | No (%) | Yes (%) | ||
| n=262 | n=187 | n=75 | ||
| Age, y, mean (SD)b | 41.8(13.1) | 42.3(13.2) | 40.6(12.9) | .330 |
| Male sex | 110 (42.0) | 88 (47.1) | 22 (29.3) | .009 |
| Atopic dermatitis | 33 (12.6) | 30 (16.0) | 3 (4.0) | .008 |
| Hairdresser–aesthetician | 34 (13.0) | 7 (3.7) | 27 (36.0) | <.001 |
| Clinical course >6mo | 210 (80.5) | 156 (83.9) | 54 (72.0) | .029 |
Allergens Most Often Provoking Reactions of Current Relevance
| Allergen | No. of Positive Patch Tests With a Currently Relevant Reaction |
|---|---|
| Ethylene glycol dimethacrylate | 18 |
| Hydroxypropyl methacrylate | 16 |
| Nickel | 15 |
| 2-Hydroxyethyl methacrylate | 10 |
| Potassium dichromate | 9 |
| Methylisothiazolinone | 9 |
| Triethylene glycol dimethacrylate | 9 |
| Hydroxyethyl methacrylate | 8 |
| Chloromethylisothiazolinone/isothiazolinone | 7 |
| Urethane dimethacrylate | 7 |
Reactions of Current Relevance According to Occupation.a
| Occupation | No. of Patients | Reactions of Current Relevance |
|---|---|---|
| Food handler | 35 | 6 (17.1) |
| Hairdresser–aesthetician | 34 | 27 (79.4) |
| Housekeeper | 29 | 8 (27.6) |
| Construction worker | 27 | 9 (33.3) |
| Cleaner | 24 | 5 (20.8) |
| Sanitation worker | 21 | 4 (19.1) |
| Office worker | 13 | 2 (15.4) |
| Agriculture–animal husbandry | 13 | 3 (23.1) |
| Sales | 9 | 3 (33.3) |
| Chauffeur | 5 | 1 (20.0) |
| Automobile industry | 5 | 1 (20.0) |
| Mechanic | 4 | – |
| Student | 4 | – |
| Retired person | 4 | – |
| Metallurgy industry | 3 | – |
| Industrial chemistry, pharmaceuticals | 2 | – |
| Textile industry | 1 | – |
| Unemployed | 1 | – |
| Other | 25 | 4 (16.00) |
| Not specified | 3 | 1 (33.33) |
Employment as a hairdresser–aesthetician (OR,14.46; 95% CI,5.94–35.23) was strongly and positively associated with a finding of currently relevant reactions, whereas male sex (OR,=0.467; 95% CI,0.263–0.829), patient history of atopic dermatitis (OR,0.218; 95%CI,0.064–0.738), and time since symptom onset of more than 6months (OR,0.495; 95%CI,0.261–0.936) were inversely associated.
Predictive ModelThe variables confirmed to be predictors on multivariate analysis were employment as a hairdresser–aesthetician, male sex, and patient history of atopic dermatitis. These variables were entered as present (1) or absent (0). The model deduced by logistic regression (Table 4) was as follows: 2.316×(hairdresser–aesthetician)−1.792×(atopic dermatitis)−0.601×(male sex). A patient's score was positive (presence of a currently relevant reaction) if it was higher than the cut-point K.
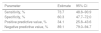
Factors in the Linear Logistic Regression Model.a
| Coefficient (SE) | AICb | Odds Ratio (95% CI) | |
|---|---|---|---|
| Independent term | −0.708 (0.248) | – | – |
| Atopic dermatitis | −1.792 (0.846) | 199.1 | 0.167 (0.032; 0.874) |
| Male sex | −0.601 (0.374) | 195.4 | 0.548 (0.264; 1.140) |
| Hairdresser–aesthetician | 2.316 (0.568) | 213.7 | 10.1 (3.333; 30.8) |
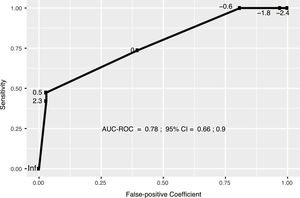
The model displayed moderate discrimination, with an AUC-ROC of 0.78 (95% CI, 0.66–0.90 (Fig. 1). The optimum cut-point according to the criterion of proximity to the upper right corner was K=−0.3. The properties supporting the model's ability to identify cases (discrimination) are shown in Table 5.
Properties of the Model at the Cut-point K=−0.3.a
| Parameter | Estimate | 95% CI |
|---|---|---|
| Sensitivity, % | 73.7 | 48.8–90.9 |
| Specificity, % | 60.3 | 47.7–72.0 |
| Positive predictive value, % | 34.1 | 25.8–43.6 |
| Negative predictive value, % | 89.1 | 79.0–94.7 |
Predictive models are highly useful for clinical decision-making. Patch tests are done to detect sensitization to a product that is causing contact dermatitis. It would therefore be useful to have a predictive model that identifies patients who are most likely to have a positive patch test reaction of current clinical relevance. Our model relies on the presence or absence of 3 predictors: employment as a hairdresser–aesthetician, male sex, and a history of atopic dermatitis. These 3 factors were assigned optimal weights by logistic regression. The proposed predictive model, validated in a second data set different from the one used to develop the model, had an AUC of 0.78. For the selected cut-point (K=−0.3), the negative predictive value was 89.1%. Thus, when a patient has a score under −0.3, there is only a 10.9% chance of positive patch test findings of current relevance.
For example, if a non-atopic woman who works as a hairdresser–aesthetician is the patient, her score would be calculated as follows: 2.316×1−1.792×0−0.601×0=2.316. Since the resulting score is greater than −0.3, patch testing would be indicated with no need to wait to see her response to standard treatment with topical corticosteroids and emollients. The score for a man with atopic dermatitis who did not work as a hairdresser, on the other hand, would be calculated as follows: 2.316×0−1.792×1−0.601×1=−2.393. Given this score, a more conservative approach of prescribing hand care and waiting to see the response before testing would be advisable. There are certain constraints on applying predictive models, and the criteria for including patients when developing one must be made clear. We excluded patients who had eczema in other parts of the body in addition to the hands in order to attenuate an effect of clinical variability. A predictive model is valid for use in the study population or one of similar characteristics, so our model is not applicable to other dissimilar populations. The small size of our patient sample, the limited number of clinical variables analyzed, and the preponderance of patients who worked as hairdresser–aestheticians and who were sensitized to acrylates are limitations of our study. The lack of other clinical data stored in our database prevented us from including other variables, such as clinical type,5,13,14 which would have to be taken into account in more exhaustive multicenter studies.
The only model developed to predict hand eczema, to our knowledge, was published by Meding and Swanbeck15 in 1990. Their model was based on a set of clinical variables. We have found no study attempting to predict currently relevant positive patch test results, nor any other predictive model specifically for hand eczema. Most studies on hand eczema describe clinical variables that are associated with greater or lesser risk for allergic contact dermatitis and positive patch test findings. However, most of them do not take into consideration whether or not the positive findings are of current relevance in the patient's life.4,5,13,16–19
The rate of positive reactions was 66.03% in our data set, and the 28.6% that were of current relevance were mainly in women, consistent with previous studies.4,5,13,14,16,20
The association between hand eczema and occupational risk factors is well established and can be seen in over half of patient cohorts in Europe.5 However, only a limited number of studies link the frequency of positive patch test reactions to specific occupations.17–19 In addition, the occupation that predominates in studies differs according to population. Employment as a hairdresser–aesthetician was the main risk factor for contact dermatitis evidenced by a currently relevant positive test result in our study. This association was largely the result of the nature of the study population itself. The association between hand eczema and occupational exposure to acrylates in hairdressers has been described with ever increasing frequency in the last decade.21–23
The prevalence of atopic dermatitis in our study was 12.6%, and the presence of this factor was inversely associated with having a positive reaction of current relevance. Although studies are not comparable, we note that a multicenter study enrolling 416 patients with hand eczema recorded fewer positive patch test results in patients with a history of atopic dermatitis than in patients with no such history (55% vs 66%, respectively; P=.052).4 Other authors have found that the differences are not significant.13,16 Publications on contact eczema at any location, on the other hand, report a clear relation between atopic dermatitis and higher or lower frequencies of positive patch test results.14,20 These discrepancies may be attributable more to selection bias at the moment of deciding to order patch tests or not in atopic patients rather than to an influence of atopic dermatitis on sensitization in these patients.
Allergic contact dermatitis is seen largely in women, who also have significantly more positive patch test results than men both in contact eczema and hand eczema,4,13,20 consistent with our findings. Patch test positivity of current relevance was inversely associated with male sex in our study.
Although a diagnosis of chronic eczema is often the main indication for doing patch tests,1–6 we found no studies analyzing this aspect. In our study, lesion onset more than 6months earlier was inversely associated with finding a positive reaction to a currently relevant allergen, although the association was not confirmed in the multivariate analysis. The small size of our patient sample prevented us from dividing it into 2 groups according to time since lesion onset. A larger patient cohort that could be subdivided might suggest a cut-point for an association between time since onset and test positivity. Even considering the limitations of our study, however, we have shown that there are other clinical factors that are better indicators than chronicity for ordering patch tests.
ConclusionsIn spite of limitations, our study offers a mathematical approach to prediction that may be very useful for decision-making in our clinical management of contact dermatitis. In our setting, all hairdresser–aestheticians who consult us for hand dermatitis should have patch tests performed regardless of how long lesions have been present. Our model suggests that a diagnosis of chronic eczema is not a necessary indication for patch testing. Rather, the dermatologist should consider the possibility that a patient might have been exposed to specific allergens, such as would be the case for hairdressers–aestheticians in contact with acrylates.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ponce S, Borrego L, Saavedra P. Modelo predictivo de dermatitis alérgica de contacto en pacientes con eccema de manos. Actas Dermosifiliogr. 2020;111:300–305.