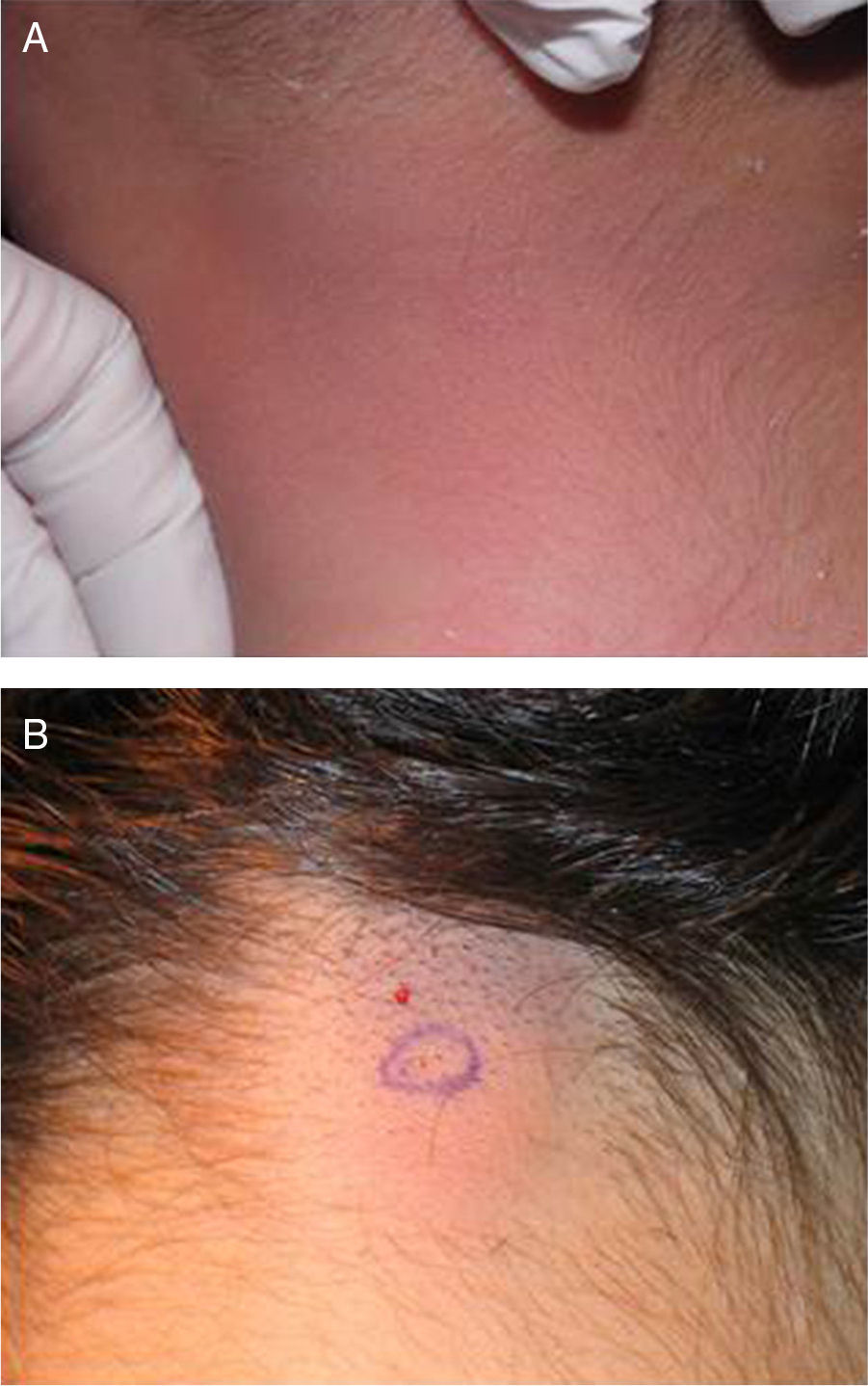
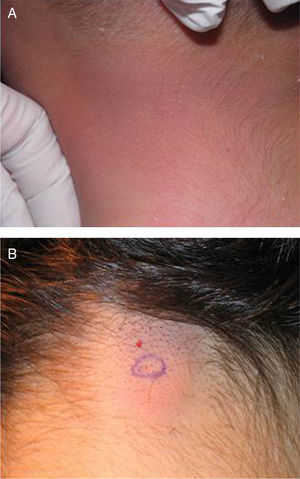
Dermatomyofibroma is a rare benign tumor of myofibroblastic origin that was initially called plaque fibromatosis in the literature.1 It is most common in young women, but has occasionally been described in pediatric patients. A recently published review gathered a total of 34 cases in children.2 We present 2 pediatric cases (Fig. 1, A and B) recently diagnosed and treated in our hospital. These cases support the benign nature of the lesion and the tendency of the tumor to arise on the neck.
The first patient was a 5-year-old boy with no past medical history of interest. He was referred to the dermatologist for evaluation of a tumor on the neck (Fig. 1A) that his parents had noticed approximately 6 months earlier. There was no reported history of trauma. This asymptomatic lesion was palpable more than visible and it had a maximum diameter of 0.6cm.
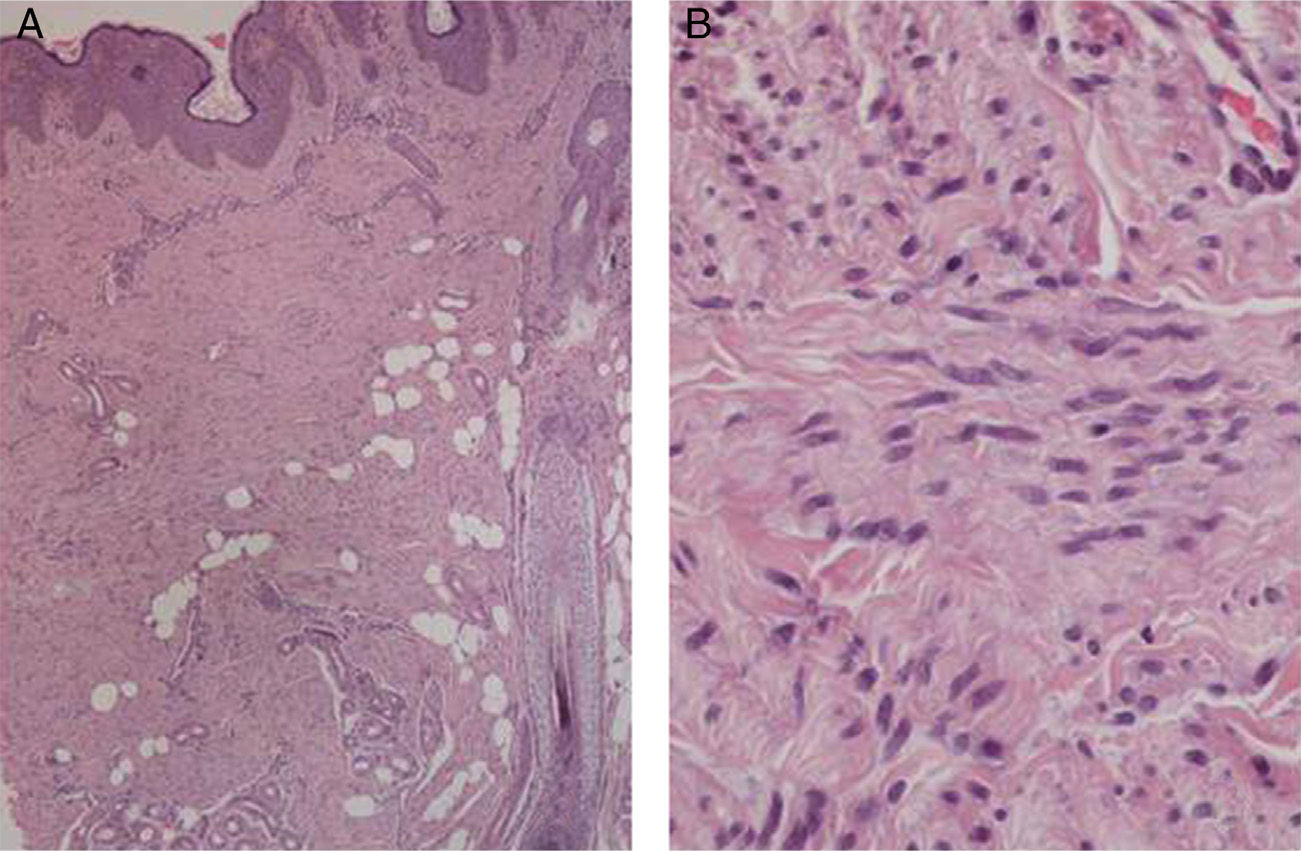
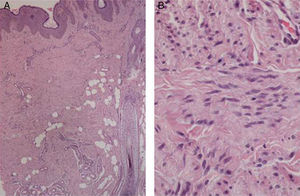
A punch biopsy taken from the center of the lesion revealed epidermal hyperplasia with mild hyperpigmentation of the basal layer. The full thickness of the dermis was affected by a proliferation of spindle-shaped cells in a fascicular arrangement, with their axes mainly oriented parallel to the epidermis; the lesion was paucicellular, and no cellular atypia or mitotic figures were observed. The spindle cells had slightly wavy nuclei (Fig. 2, A and B). No hyaline globules were observed in the cell cytoplasm. Immunohistochemistry was negative for protein s100, smooth muscle actin, muscle specific actin, desmin, Caldesmon, and CD34. Complete excision of the lesion was then performed and histology study reported identical findings.
The second patient was a 13-year-old boy with no relevant past medical history. He was referred to dermatology for investigation of an asymptomatic erythematous nodule on the neck with a maximum diameter of 1cm (Fig. 1B). The lesion had been present for at least 2 years. No history of trauma to the area was reported.
Punch biopsy and subsequent complete excision revealed an epidermis and superficial and mid dermis with no significant alterations, and a proliferation of spindle-shaped cells in the reticular dermis and most superficial part of the subcutaneous cellular tissue. This proliferation, which was paucicellular and showed no cellular atypia, formed bundles running parallel to the epidermis. The lesion presented noninfiltrative growth, surrounding but not eliminating the skin adnexa. Immunohistochemistry showed the cells to be negative for s100, smooth muscle actin, muscle specific actin, desmin, bcl-2, CD34, and CD99. The histology findings were identical to those of the previous case, shown in Fig. 2, A and B.
Both patients were followed up for 2 years after excision of the tumors and no recurrences were observed.
Dermatomiofibroma is a rare tumor in the pediatric age range. The first description of this tumor was published by Hügel1 in 1991. It was initially called plaque fibromatosis. The name dermatomyofibroma was proposed by Kamino2 in 1992. The largest global series was gathered by Mentzel et al.,3 with a total of 56 patients aged between 3 and 51 years, and there was a female predominance. The main characteristic of the tumor is a proliferation of spindle cells oriented parallel to the surface of the epidermis. Ultrastructural studies and immunophenotyping have shown these cells to be fibroblasts and myofibroblasts. The immunohistochemical profile is very variable, although vimentin is frequently expressed. CD34 expression has been reported in some cases; this can complicate the diagnosis as dermatofibrosarcoma protuberans must then be considered in the differential diagnosis. Immunohistochemistry is useful to orient the pathologist, but the diagnosis is fundamentally morphological. Treatment is surgical, and recurrence is rare after excision with an adequate margin.
Tardío et al.4 gathered a total of 34 cases in children and 56% of those tumors were found on the neck, as in the 2 patients we describe. A primary characteristic of pediatric dermatomyofibroma therefore appears to be its tendency to arise in the cervical region. In adults, on the other hand, the tumor arises most frequently on the shoulders or proximal region of the limbs and is less common on the neck. The second characteristic is that the tumor predominantly affects boys. In adults, 90% of cases are in women.5–8 It has been speculated that the tumor may spontaneously regress in male children at puberty and persist in girls, leading to a higher prevalence in adult women.
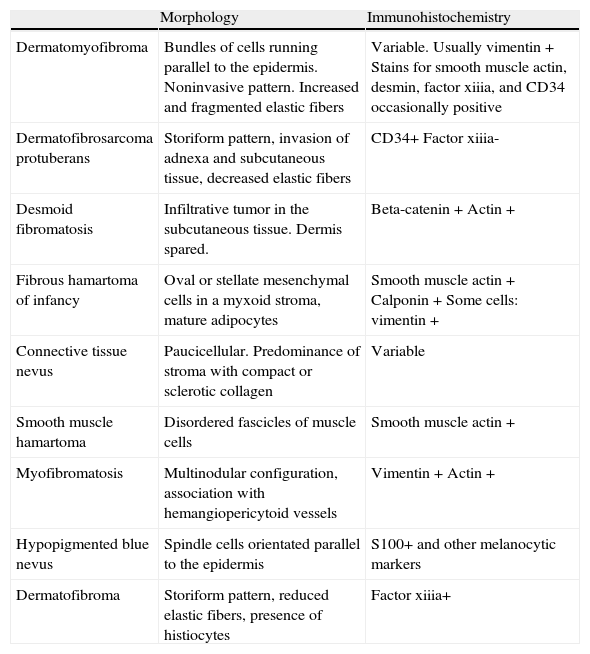
The importance of this disease is its differentiation from other tumors formed of spindle cells, such as desmoid tumor and dermatofibrosarcoma protuberans. In addition, other mesenchymal lesions more typical of the pediatric age range, such as fibrous hamartoma of infancy, myofibromatosis, connective tissue nevus, and smooth muscle hamartoma, must be excluded. A guide to the differential diagnosis of these tumors is presented in Table 1.
Key to the Differential Diagnosis of Mesenchymal Tumors in the Children.
| Morphology | Immunohistochemistry | |
| Dermatomyofibroma | Bundles of cells running parallel to the epidermis. Noninvasive pattern. Increased and fragmented elastic fibers | Variable. Usually vimentin+ Stains for smooth muscle actin, desmin, factor xiiia, and CD34 occasionally positive |
| Dermatofibrosarcoma protuberans | Storiform pattern, invasion of adnexa and subcutaneous tissue, decreased elastic fibers | CD34+ Factor xiiia- |
| Desmoid fibromatosis | Infiltrative tumor in the subcutaneous tissue. Dermis spared. | Beta-catenin+ Actin+ |
| Fibrous hamartoma of infancy | Oval or stellate mesenchymal cells in a myxoid stroma, mature adipocytes | Smooth muscle actin+ Calponin+ Some cells: vimentin+ |
| Connective tissue nevus | Paucicellular. Predominance of stroma with compact or sclerotic collagen | Variable |
| Smooth muscle hamartoma | Disordered fascicles of muscle cells | Smooth muscle actin+ |
| Myofibromatosis | Multinodular configuration, association with hemangiopericytoid vessels | Vimentin+ Actin+ |
| Hypopigmented blue nevus | Spindle cells orientated parallel to the epidermis | S100+ and other melanocytic markers |
| Dermatofibroma | Storiform pattern, reduced elastic fibers, presence of histiocytes | Factor xiiia+ |
Please cite this article as: Romaní J, Leal L, Sáez A, Luelmo J. Dermatomiofibroma en la nuca: descripción de 2 casos en la edad pediátrica. Actas Dermosifiliogr. 2014 105:315–317.