A 62-year-old man presented with asymptomatic skin lesions that were located exclusively on the thorax and had appeared more than 15 years earlier. The patient had no relevant medical or surgical history and was not taking regular medication. Physical examination revealed erythematous-brownish plaques without scaling or infiltration (Fig. 1A). The palms of the hands, soles of the feet, and the mucous membranes were free of any lesions. Darier sign was negative and neither lymphadenopathy nor organomegaly were evident on palpation.
Although clinically the patient’s lesions could be considered compatible with mastocytosis, the duration of the lesions and the absence of Darier sign were striking. The clinical stability of the lesions over several years and the absence of palmoplantar involvement decreased the likelihood of secondary syphilis.
Results of laboratory tests revealed a normal biochemical profile and a normal complete blood count. The only findings of interest were polyclonal hypergammaglobulinemia with a slight increase in immunoglobulin (Ig) G and IgA, and an increase in acute phase reactants (erythrocyte sedimentation rate [ESR] and C-reactive protein [CRP]). Autoimmunity markers were negative and no alterations in urine sediment were observed.
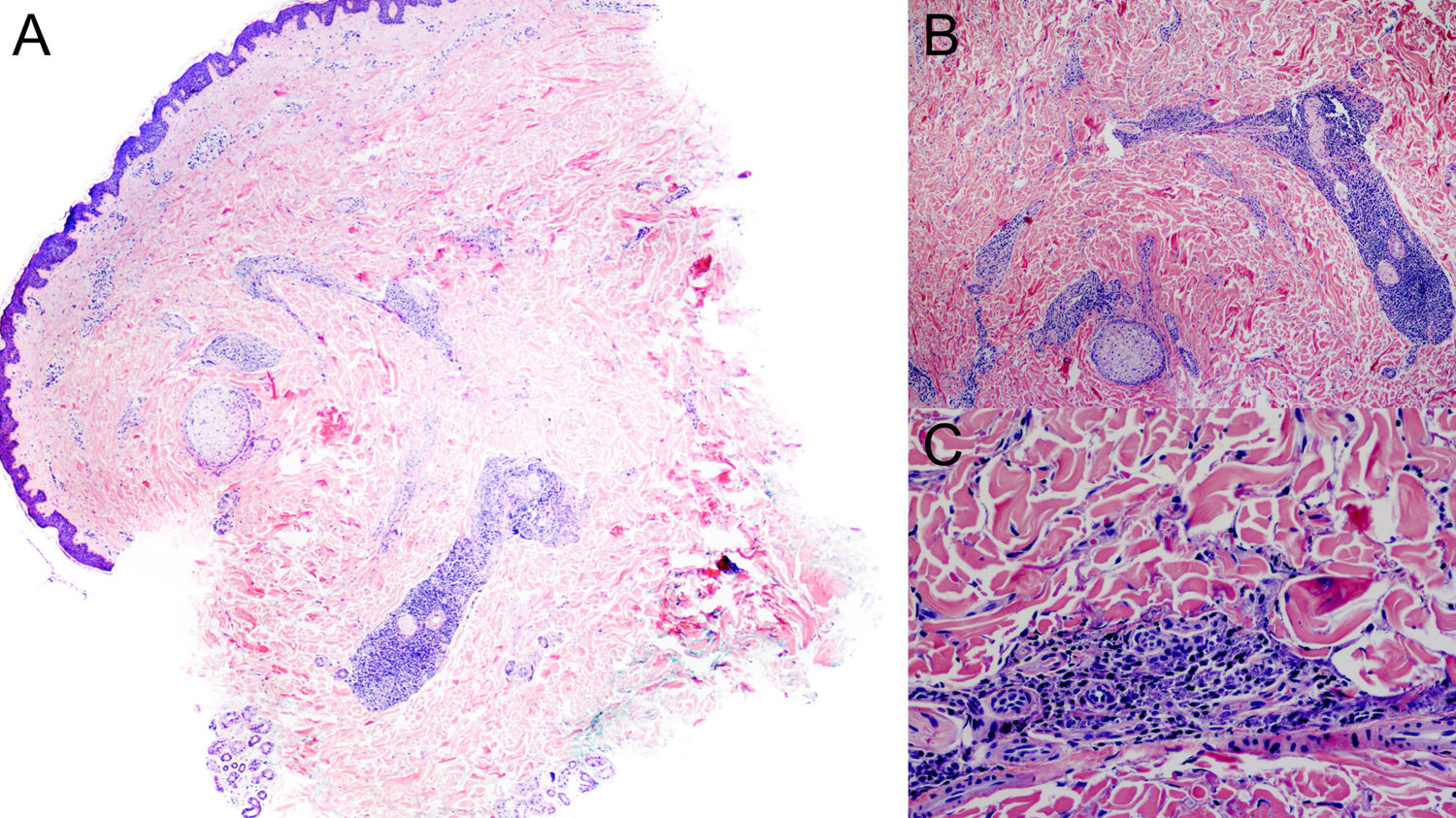
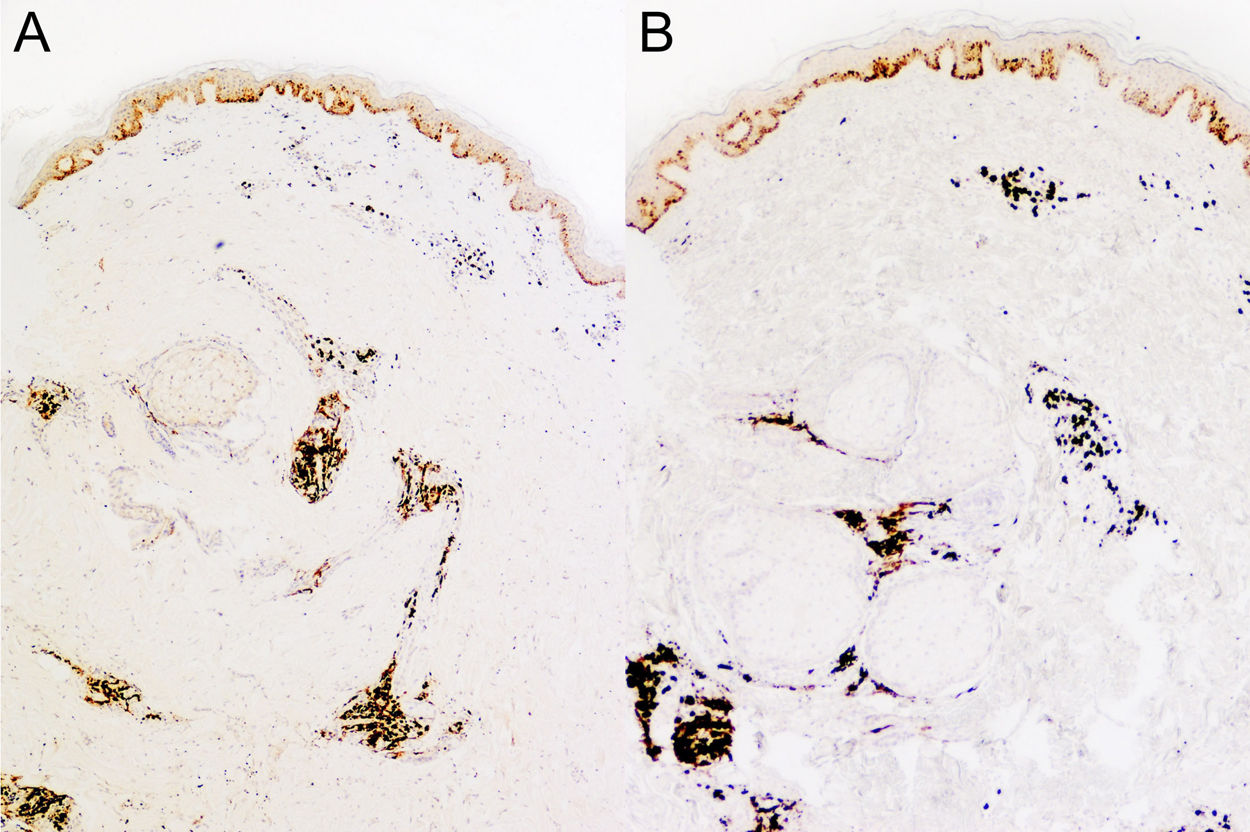
A punch biopsy of one of the chest lesions showed superficial and deep infiltrate with perivascular and periadnexal involvement (Fig. 2A), as well as perineural involvement (Fig. 2B). Observation at higher magnification revealed that the infiltrate consisted of plasma cells (Fig. 2C). Immunohistochemistry showed positive staining for κ and λ Ig light chains (Fig. 3), with no light chain restriction. Based on these observations, the differential diagnosis included other entities characterized by plasma-cell-rich infiltrate including infectious diseases (e.g. syphilis, leishmania), autoimmune diseases (e.g. lupus), and neoplastic diseases (e.g. plasmacytoma). Syphilis serology was negative. The hematology department performed peripheral blood tests, which showed no alterations in white blood cells or in the proteinogram. In the absence of any clinicopathologic correlation or signs of hematological disease, and given the negative syphilis serology and the presence of plasma-cell-rich infiltrate, a diagnosis of cutaneous plasmacytosis was established based on the pathological findings. In accordance with the recommendations of the hematology department, no extension study was carried out owing to the duration of the lesions and the absence of systemic signs, lymphadenopathy, organomegaly, or laboratory abnormalities.
Pathology images. A, Panoramic image showing superficial and deep perivascular and periadnexal infiltrate (hematoxylin-eosin [HE], original magnification ×20). B, Higher magnification image showing perineural infiltrate (HE, original magnification ×40). C, Detail of the inflammatory infiltrate, which consists of plasma cells.
Cutaneous plasmacytosis is extremely rare and usually appears in middle-aged adults, predominantly affecting Asian (mainlyJapanese) patients and rarely white patients.1,2 This disease is rarely reported in the literature, and may be underdiagnosed due to differences in nomenclature; it was not until 19803 that the term cutaneous plasmacytosis was coined. Some authors prefer the term systemic cutaneous plasmacytosis, as lymphadenopathy and/or organomegaly have been reported in some patients, and even in patients without such alterations plasmacytic infiltrate has been detected in biopsies of apparently clinically normal lymph nodes.1–4
Laboratory analyses typically reveal polyclonal hypergammaglobulinemia, which is usually, as in the present case, due to alterations in IgG and IgA, as well as increased levels of acute phase reactants such as ESR and CRP, with no alterations in biochemical parameters or in the complete blood count.
Histology shows superficial and deep perivascular and periadnexal plasma cell infiltrate, without light chain restriction (i.e. expressing κ and λ light chains), which indicates a polyclonal process.5 Characteristic perineural involvement has also been described in some cases, including in our patient.6
As also proposed for other hematological processes, some authors have suggested a relationship between cutaneous plasmacytosis and Epstein Barr virus or Borrelia infection, although this has not been demonstrated in the few series published to date.1,5,6
There is also some controversy as to whether this process is associated with hematologic neoplasms or other reactive plasmacytic processes, such as Castleman disease, although current knowledge suggests that these processes are independent.5
Owing to the rare nature of this condition, there are neither guidelines nor consensus on the treatment of affected patients. Of the several treatments tested, most have been only partially effective, including oral and topical corticosteroids, topical calcineurin inhibitors, melphalan, immunoglobulins, rituximab and thalidomine, and phototherapy (psoralen and ultraviolet [UV] A and narrowband UVB therapy).1,6,7
In conclusion, cutaneous plasmacytosis is uncommon in white individuals, and usually has a chronic and benign long-term course. Nonetheless, follow-up of these patients is recommended owing to the scarcity of information about this pathological process.6
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Álvarez-Chinchilla PJ, Scheneller-Pavelescu L, Niveiro M, Devesa P. Plasmacitosis cutánea: una infrecuente enfermedad cutánea a tener en cuenta. Actas Dermosifiliogr. 2020;111:877–879.



![Pathology images. A, Panoramic image showing superficial and deep perivascular and periadnexal infiltrate (hematoxylin-eosin [HE], original magnification ×20). B, Higher magnification image showing perineural infiltrate (HE, original magnification ×40). C, Detail of the inflammatory infiltrate, which consists of plasma cells. Pathology images. A, Panoramic image showing superficial and deep perivascular and periadnexal infiltrate (hematoxylin-eosin [HE], original magnification ×20). B, Higher magnification image showing perineural infiltrate (HE, original magnification ×40). C, Detail of the inflammatory infiltrate, which consists of plasma cells.](https://static.elsevier.es/multimedia/15782190/0000011100000010/v1_202012160744/S1578219020303152/v1_202012160744/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)