Bullous morphea is a rare form of localized scleroderma. Since the description of the first case, numerous theories have been put forward on the origin of the blisters, but the actual mechanism by which they develop remains unclear.
Our patient, a 63-year-old woman, presented 2 lesions that had arisen some months earlier, localized symmetrically in the pretibial regions (Fig. 1). The lesions had an atrophic appearance, an erythematous base, and a central blister that contained a blood-stained fluid. The patient described no history of trauma.
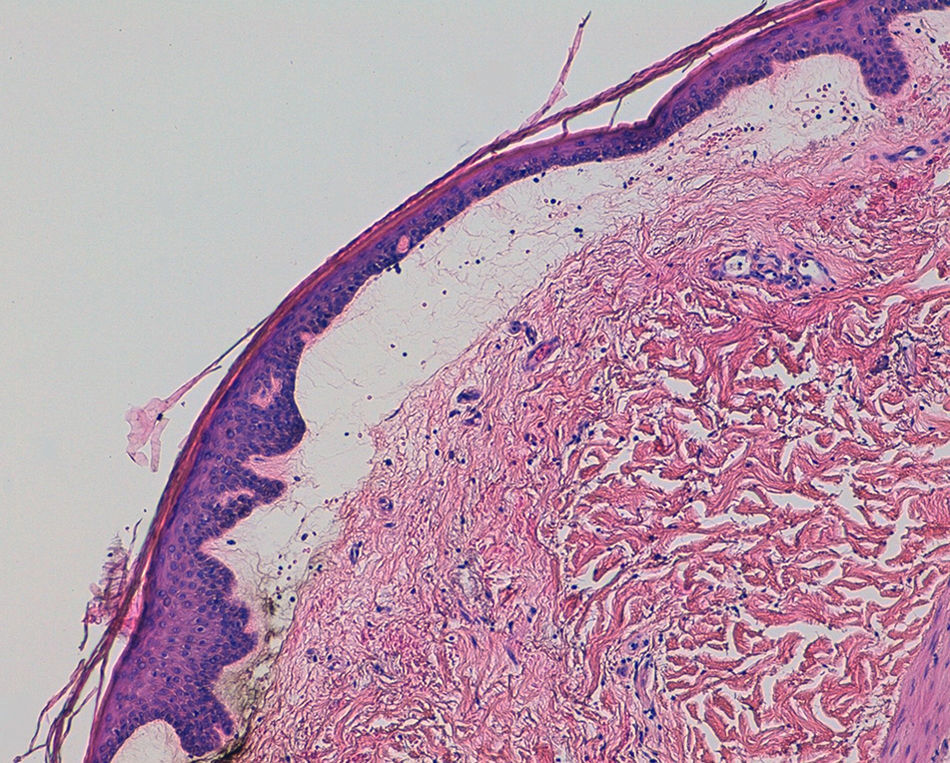
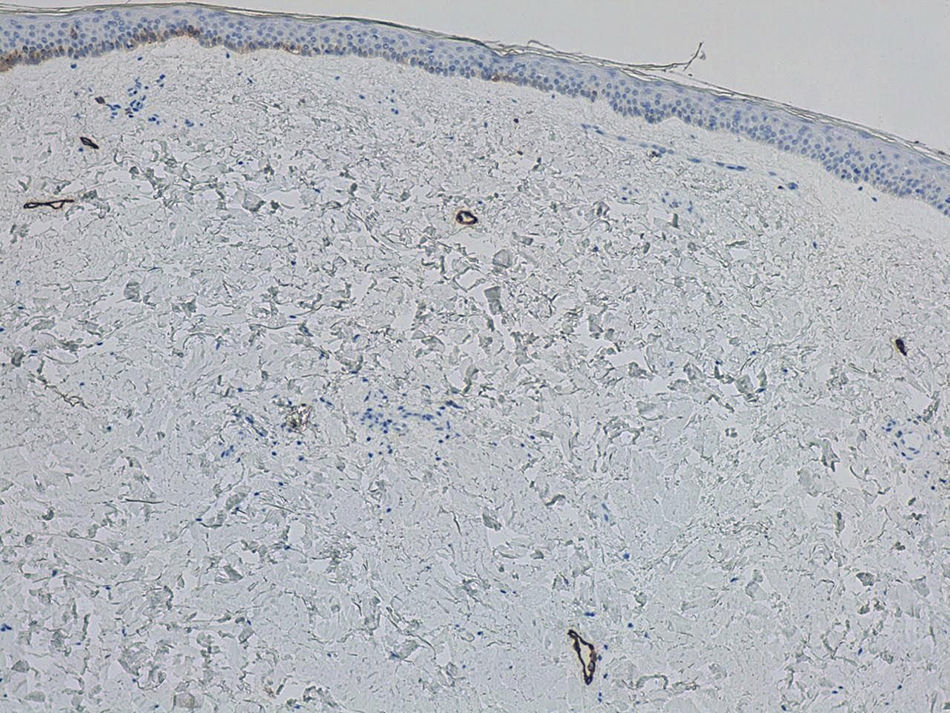
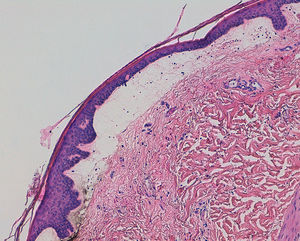
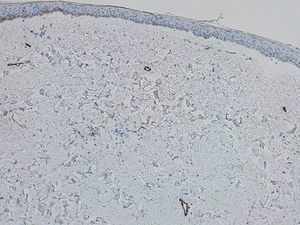
Biopsy showed subepidermal separation with preservation of the basal layer. A mild inflammatory component and collagen fibrils were observed in the superficial dermis, but extensive sclerosis with a dense lymphocytic infiltrate was found in the reticular dermis and subcutaneous cellular tissue, though with no vasculitis or significant presence of eosinophils (Fig. 2). No lymphangiectasia was observed after staining with hematoxylin-eosin or D2-40 (Fig. 3). The findings were compatible with a diagnosis of bullous morphea. Blood tests were within normal limits and Borrelia serology was negative. Topical therapy with betamethasone and fusidic acid was started, leading to resolution of the blisters, but the sclerotic plaques deteriorated and systemic treatment was therefore commenced with oral methotrexate, achieving a good response.
Bullous morphea is a rare form of localized scleroderma.1 The first case was described by Morrow in 1896.2 Since that time, numerous theories on its origin have been proposed.3–5
The most widely accepted theory on the origin of the blisters has been lymphatic obstruction due to lymphangiectasia caused by the underlying sclerotic changes.1,3,5,6 However, not all lesions of bullous morphea present lymphangiectasia on histology, nor do all cases of scleroderma with lymphangiectasia present blisters.1,4,7
Local trauma may be another etiologic and pathogenic factor, given the hemorrhagic content of some blisters and their frequent localization in areas of friction such as the legs and intertriginous areas.1,7,8 No history of trauma was detected in our patient, but some findings, such as the localization of the blisters in the pretibial region, the blood-stained content, and the absence of other etiologic and pathogenic factors, could suggest that unperceived trauma may have played a role in the formation of the lesions.
Cases have been reported in which blisters developed as an isotopic or isomorphic response on residual lesions of herpes zoster or on the scars of previous surgery, trauma, injections, or radiation.1,6,8 Some authors have suggested that eosinophils may play a role in this disease,5 while other postulate reactive oxygen species as a possible causative factor.9
We have also found cases with 2 or more coexisting bullous diseases, such as pemphigus vulgaris, epidermolysis bullosa, and porphyria cutanea tarda; these diseases were ruled out in our patient.3,10 Likewise, scleroderma-like changes are recognized in patients with graft-versus-host disease, and the appearance of blisters on these lesions has also been reported.8
The diagnosis of bullous morphea requires a detailed medical history, full physical examination, skin biopsy with direct immunofluorescence, and blood tests including serology for Borrelia (typically negative) and autoimmunity.3–5
Histology reveals a greater or lesser degree of epidermal atrophy with flattening of the crests. The blisters are subepidermal, have a blood-stained content, and may be associated with edema of the papillary dermis.1,4,5 In the reticular dermis there are prominent thick bundles of hyalinized collagen that destroy the adnexal structures.5
The main differential diagnosis of morphea is with lichen sclerosus et atrophicus, and the 2 diseases can coexist in some patients. In contrast to lichen sclerosus et atrophicus, the basal layer and the elastic fibers of the reticular dermis are unaffected in bullous morphea, which also does not show follicular plugs.4,7
Numerous therapeutic strategies have been used, including phototherapy, topical and systemic corticosteroids, topical vitamin D analogs, antimalarials, various immunosuppressant agents, systemic retinoids, certain antibiotics, colchicine, and phenytoin. Also, isolated cases have been treated with extracorporeal photophoresis, N-acetylcysteine, imiquimod, sulfasalazine, or skin grafts, with varying results.3–5,9
In conclusion, we have presented a case of bullous morphea in which lymphangiectasia was not detected on histology; this, together with the pretibial site of the lesions and their blood-stained content, leads us to speculate that unperceived trauma may have been the cause of the blisters in this case. Regarding treatment, it would appear reasonable to adopt an approach similar to that for nonbullous forms of morphea, starting with topical agents (corticosteroids, vitamin D analogs) or phototherapy, and advancing to systemic treatments such as methotrexate if no response is observed.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sánchez-Pérez S, Escandell-González I, Pinazo-Canales MI, Jordá-Cuevas E. Un nuevo caso de morfea ampollosa y discusión de los factores etiopatogénicos en la formación de las ampollas. Actas Dermosifiliogr. 2017;108:75–76.