Over 113 new cases of basal cell carcinoma (BCC) are diagnosed per 100000 inhabitants every year in Spain.1 BCC is associated with significant morbidity and health care costs. Patients who develop BCC at a younger age are more likely to have predisposing characteristics, such as a sensitive skin type or a history of sunburn.2 They are thus an ideal population for the study of risk factors and for targeted preventive measures.
In order to analyze the clinical characteristics and risk factors associated with BCC in younger adults, we reviewed all cases of BCC diagnosed in patients under 40 years of age at Hospital de Manacor in Mallorca, Spain between 2010 and 2015. Data were gathered from medical records and pathology reports.
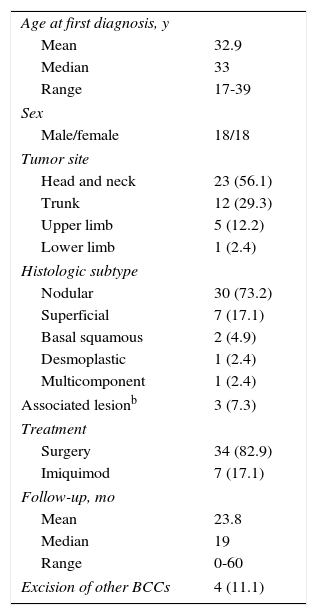
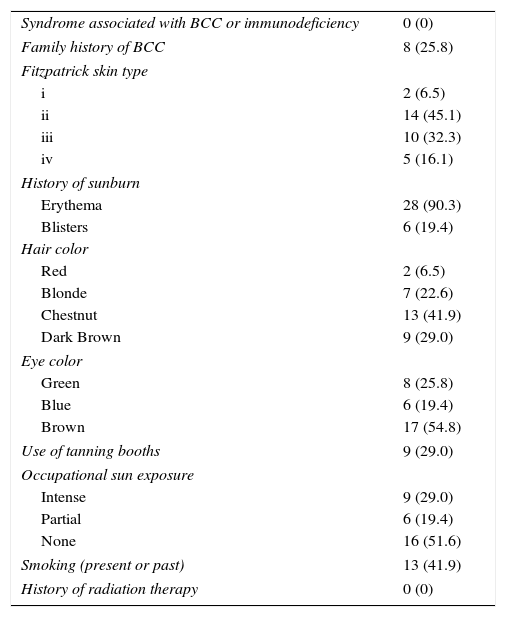
Forty-one lesions were diagnosed over the 6-year period in 36 patients (18 women and 18 men). A diagnosis of BCC had not been suspected on the grounds of clinical records or pathology reports in 6 of the tumors (14.6%) before the histologic diagnosis. Table 1 summarizes the clinical and histological characteristics of the 41 tumors, treatment received, follow-up times, and incidence of second tumors. Information on the presence of known risk factors for BCC is provided in Table 2. Information on risk factors that was not available in the medical records was obtained through telephone interviews with the patients. Five patients (4 men and 1 woman) were unlocatable and we were therefore only able to report on risk factors included in their medical records.
Clinical and Histological Characteristics, Treatment, Follow-up Time, and Incidence of Second Tumors.a
| Age at first diagnosis, y | |
| Mean | 32.9 |
| Median | 33 |
| Range | 17-39 |
| Sex | |
| Male/female | 18/18 |
| Tumor site | |
| Head and neck | 23 (56.1) |
| Trunk | 12 (29.3) |
| Upper limb | 5 (12.2) |
| Lower limb | 1 (2.4) |
| Histologic subtype | |
| Nodular | 30 (73.2) |
| Superficial | 7 (17.1) |
| Basal squamous | 2 (4.9) |
| Desmoplastic | 1 (2.4) |
| Multicomponent | 1 (2.4) |
| Associated lesionb | 3 (7.3) |
| Treatment | |
| Surgery | 34 (82.9) |
| Imiquimod | 7 (17.1) |
| Follow-up, mo | |
| Mean | 23.8 |
| Median | 19 |
| Range | 0-60 |
| Excision of other BCCs | 4 (11.1) |
Data are presented as number (%) of patients unless otherwise specified.
Presence of Known Risk Factors for Basal Cell Carcinoma (BCC).a
| Syndrome associated with BCC or immunodeficiency | 0 (0) |
| Family history of BCC | 8 (25.8) |
| Fitzpatrick skin type | |
| i | 2 (6.5) |
| ii | 14 (45.1) |
| iii | 10 (32.3) |
| iv | 5 (16.1) |
| History of sunburn | |
| Erythema | 28 (90.3) |
| Blisters | 6 (19.4) |
| Hair color | |
| Red | 2 (6.5) |
| Blonde | 7 (22.6) |
| Chestnut | 13 (41.9) |
| Dark Brown | 9 (29.0) |
| Eye color | |
| Green | 8 (25.8) |
| Blue | 6 (19.4) |
| Brown | 17 (54.8) |
| Use of tanning booths | 9 (29.0) |
| Occupational sun exposure | |
| Intense | 9 (29.0) |
| Partial | 6 (19.4) |
| None | 16 (51.6) |
| Smoking (present or past) | 13 (41.9) |
| History of radiation therapy | 0 (0) |
Data are presented as number (%).
BCC is a common disease in our setting. The pathology laboratory at Hospital de Manacor, which serves a population of approximately 150 000 inhabitants in the eastern part of Mallorca, diagnosed 1841 cases of BCC based on biopsy and surgical specimens in the 6 years analyzed (306.8 cases a year). Just 2.5% of the cases corresponded to patients younger than 40 years. This proportion is similar to that reported in a previous study in Catalonia, Spain.3 The low incidence of BCC in young patients could cause diagnostic delays due to a low index of suspicion. In our series, 6 of the 41 tumors (14.6%) had not been suspected clinically.
As is usual with tumors of this type, the most common location was the top of the head. The most common subtype was nodular BCC (73.2%), contrasting with a recent report that early-onset BCC was associated with an aggressive histologic subtype.4 Three of the BCCs in our series (7.3%) were associated with a sebaceous or epidermal nevus.
Four patients (11.1%) developed a second BCC during follow-up, and 1 of these developed a third tumor. Length of follow-up was highly variable, and ranged from no follow-up in some cases to 5 years in others. In a recent study, 34% of patients diagnosed with BCC before the age of 40 years had a second BCC at the 5-year follow-up.5
None of the patients had immunodeficiency or syndromes that predispose to BCC. In relation to risk factors associated with pigmentary traits, a majority of patients had Fitzpatrick skin type ii or iii, which based on indirect data, are the most common skin types seen in routine clinical practice in our setting.6 Almost all the patients in the series had a history of sunburn and almost 20% recalled blisters. Intense and intermittent sun exposure in the early years of life is a well-known risk factor for BCC.7,8 Occupational sun exposure, whether intense (builders, agricultural workers) or intermittent (waiters, couriers, tourist guides) was reported by 48% of the patients. This type of sun exposure tends to be more sustained over time.
Nine of the 31 patients we were able to locate by telephone (7 women and 2 men) had used tanning booths. A clear association has been established between tanning booth use and early onset of skin cancer, and adults under 40 years of age who have used a tanning booth at some point during their life have been found to have twice the risk of BCC as those who have never used one.9,10 Unlike elsewhere in Europe, frequency of tanning booth use has not been studied in Spain. Apart from detecting a tendency towards a greater use of tanning booths among the women in our series, we were unable to establish correlations between any of the other risk factors due to our small sample.
In conclusion, BCC is a significant source of morbidity and health care costs in Spain. Understanding the risk factors associated with BCC is essential for designing prevention strategies and favoring early diagnosis. BCC is rare in patients under 40 years of age. Nonetheless, these patients have a higher prevalence of risk factors for this cancer, some of which are avoidable. Tanning booth use could be a major risk factor for BCC but there are no accurate data on its prevalence in Spain.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Garcias-Ladaria J, Morales-Morato FJ, Rosón MC, Rocamora V. Carcinoma basocelular en pacientes jóvenes. Actas Dermosifiliogr. 2017;108:376–377.