Multinucleate cell angiohistiocytoma (MCAH) is a rare entity that takes the form of a benign dermatologic proliferation formed by small blood vessels and multinucleate mesenchymal cells. These lesions are probably underdiagnosed because of their similarity to other disorders, such as dermatofibroma, and because of their benign, asymptomatic nature.
We report the case of a 35-year-old woman in the 36th week of her 4th pregnancy. The child born as a result of her second pregnancy had died 24hours post partum. The woman had been visiting our department for many years due to multiple asymptomatic lesions on her trunk and extremities; the lesions first appeared during the first pregnancy and had increased in number over the course of the subsequent pregnancies. The physical examination revealed more than 100 round maculopapular lesions with diameters ranging between 2 and 8mm; the lesions were erythematous-violaceous with a smooth surface and were distributed unevenly across the trunk and extremities (Fig. 1). Dermoscopy showed a fine pigmented reticular pattern around the borders and a whitish central patch (Fig. 2); these findings were compatible with clinical suspicion of multiple eruptive dermatofibroma. Because this presentation of dermatofibroma has been associated with autoimmune disease, an immunological study was performed. The salient findings were the presence of anti-Ro 60 antibodies and antinuclear antibodies distributed in a speckled pattern.
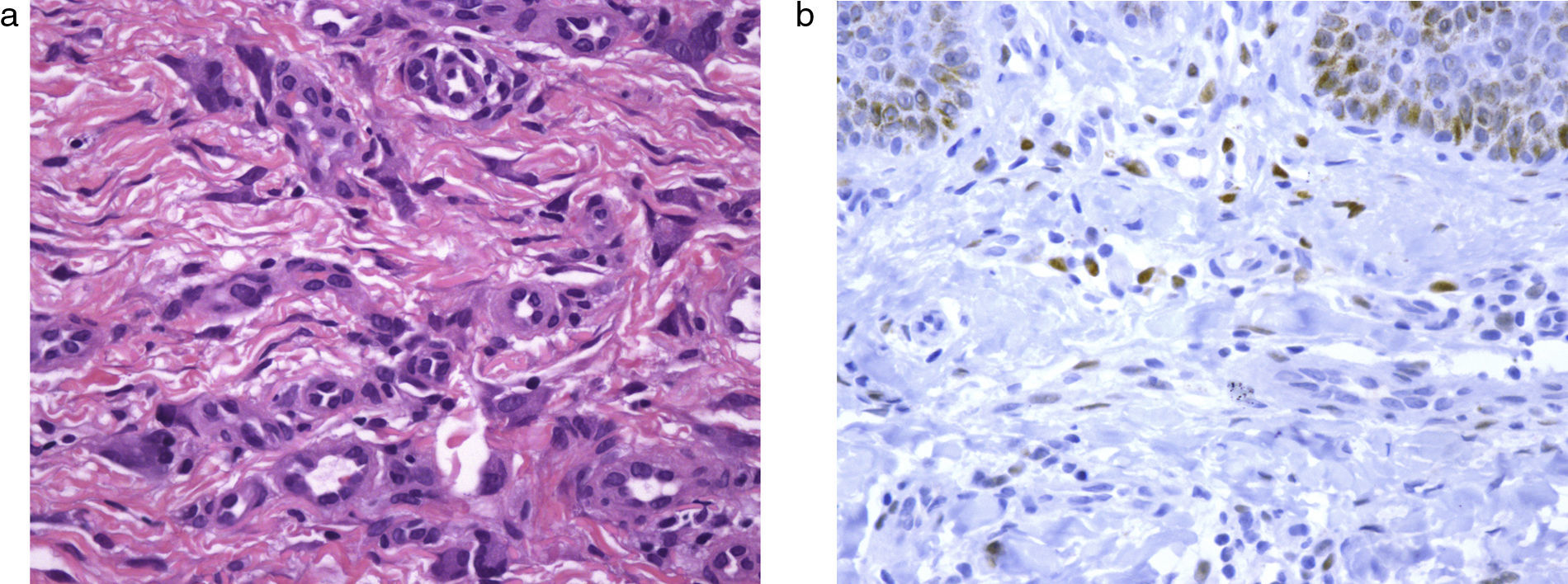
Biopsy specimens of 2 papules revealed poorly defined lesions involving the full thickness of the dermis. Histology showed that the papules consisted of numerous small blood vessels with prominent endothelia distributed with no clear pattern throughout the dermal collagen. Other findings included scant perivascular histiocytes and lymphocytes and multinucleate mesenchymal cells characterized by fewer than 10 nuclei, no abnormalities, and a large cytoplasm with angular contours (Fig. 3a). Immunohistochemical analysis showed estrogen receptor α expression in some perivascular spindle-shaped cells (Fig. 3b) and progesterone receptor expression in very few cells at the same location. Immune staining was negative for hormone receptors in the multinucleate cells. A diagnosis of generalized eruptive MCAH was reached.
A, Multinucleate mesenchymal cells with angled cytoplasmic borders and small vessels with thickened walls and prominent endothelia located in the dermal collagen (hematoxylin-eosin, original magnification x400). B, Positive immune staining for estrogen receptor α in perivascular spindle-shaped cells (original magnification x400).
The skin lesions were not treated because of the widespread nature of the outbreak. The patient was referred to obstetrics because of the positive anti-Ro 60 result and the history of the death of the newborn child after her earlier pregnancy. The neonate was monitored by the pediatrics department.
MCAH is considered to be a dermal dendrocyte proliferation. Some authors consider it to be a variant of dermatofibroma1; as with dermatofibroma, it is difficult to determine whether MCAH is a true neoplasm or a reactive process.2 MCAH presents in healthy persons and reported associations with other diseases appear to be coincidental. Several factors support the idea that this is a reactive entity: the fact that some patients present with multiple lesions, the location of lesions in sites exposed to trauma and insect bites, the absence of a familial association, and the spontaneous regression reported in some cases. A link to hormone factors has been suggested, as these lesions present more frequently in women (79% of cases) and have been associated with overexpression of estrogen receptor α.3
Including our patient, 5 cases of generalized MCAH have been reported to date: 3 men and 2 women4–7 aged between 24 and 56 years with no associated disease. Of note in our case is the coincidence of the eruptive appearance of the lesions and each pregnancy, and the finding of anti-Ro 60 antibodies with a history of the death of a newborn baby.
The dermoscopy findings concur with those reported in the literature8 and are similar to the dermoscopy pattern of dermatofibroma. Multiple eruptive dermatofibroma has been linked to an abnormal immune system. In a review of 67 cases, Zaccaria et al.9 found a link with intercurrent disease in 96% of their cases, 83% of which were immune-deficient conditions. Those authors therefore suggested that the multiple eruptive presentation of dermatofibroma might be a diagnostic marker for immunosuppressive conditions. The cases reviewed included that reported by Stainforth and Goodfield10 of a healthy woman who developed 9 dermatofibromas on the trunk during pregnancy; the authors included pregnancy as a condition involving immune-system abnormality. In light of our case, we suggest that the multiple eruptive form of MCAH may bear similarities to pregnancy-associated dermatofibroma.
In conclusion, we present the first case of generalized eruptive MCAH associated with every pregnancy in a woman who remained anti-Ro/SSA-positive and who has had no other associated symptoms to date. We suggest that this unique and rare clinical form of the disease may, in the future, be an indicator of an abnormal immune system and that it may support the association, suggested by some authors, of MCAH with hormone factors.3
Please cite this article as: Villanueva CA, et al. Angiohistiocitomas de células multinucleadas eruptivos y generalizados en una gestante. Presentación de un caso y revisión de la literatura. Actas Dermosifiliogr.2012;103:450-2.