Erosive palmoplantar lichen planus (LP), also known as ulcerative or bullous LP, was first described by Cram et al.1 in 1966 as a rare variant of LP that can affect mucous membranes, palms, and soles. It presents clinically as erythematous, ulcerated plaques that run an extremely chronic course and are resistant to all types of treatment.
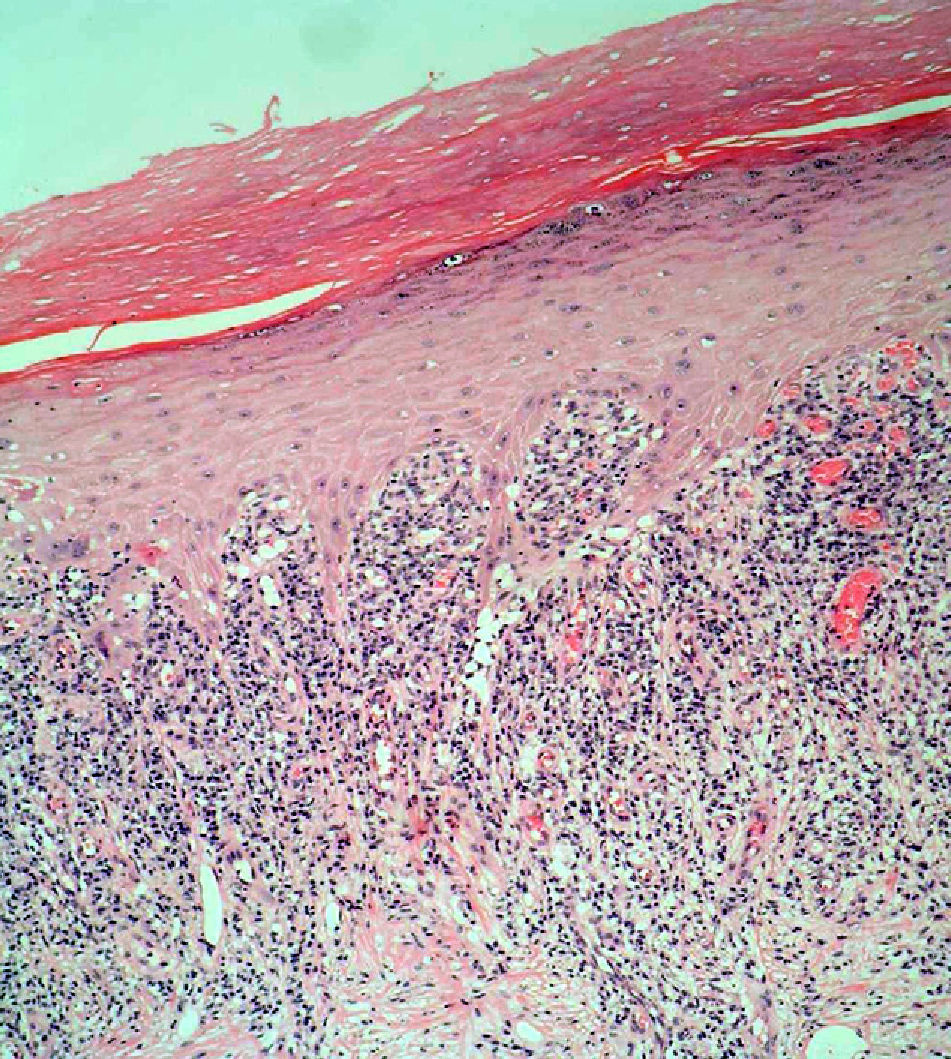
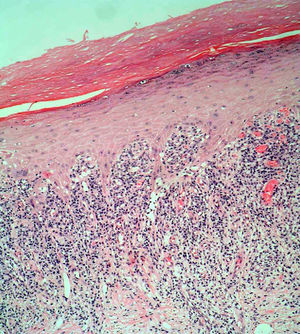
The patient was an 84-year-old woman with a personal history of hypertension, aortic valve fibrosclerosis, and polyarthritis who had been receiving treatment with paracetamol, acetylsalicylic acid, atorvastatin, and candesartan-hydrochlorothiazide for several years. She presented with a very painful ulcerated lesion on her right foot that had appeared 6 months earlier and made walking difficult. Physical examination revealed an ulcerated plaque, measuring 4×5cm, on the medial aspect of the right heel. The base of the lesion was filled with granulation tissue, which in some areas was covered with whitish, macerated epithelium. Another ulcer with the same characteristics was present on the dorsal aspect of the first toe (Figs. 1 and 2). The dermatological examination also revealed the presence of whitish reticulated areas on the buccal mucosa and pterygium on several fingernails. In addition, the patient had total scalp alopecia, having lost her hair, as well as all 10 toenails, 6 years earlier. She did not have alopecia of the eyebrows, eyelashes, axilla, or pubic area, or any other cutaneous abnormalities. Blood tests, including liver function tests, hepatitis B serology, and hepatitis C serology, were normal or negative. Skin biopsy revealed marked orthokeratotic hyperkeratosis, acanthosis, and a band-like lymphocytic infiltrate in the upper dermis, without melanophages. Also present were spiculated dermal papillae and vacuolar degeneration at the dermal-epidermal junction. The findings were consistent with LP (Fig. 3).
On the basis of the clinical and histopathologic findings, the patient was diagnosed with erosive palmoplantar LP and was prescribed treatment with oral prednisone (1mg/kg/d). Two months later, the ulcerated lesions had healed. Systemic treatment was continued with a tapering dose for a further 6 months and finally withdrawn. The patient then started a 1-month regimen of topical clobetasol propionate (500 mcg/g). She has remained asymptomatic since treatment was completed 24 months ago.
Erosive palmoplantar LP is a rare form of LP that mainly affects elderly people. The lesions initially present as erythema and blisters on the feet and evolve into intensely painful, disabling erosions and ulcers. They usually occur on the heels but can affect the entire sole and even the dorsal surface of the toes.2 The disease can lead to the total loss of all toenails.
Erosive palmoplantar LP can occur in isolation or in association with cicatricial alopecia of the scalp and diffuse alopecia of the axilla and pubic area. In many cases, it is accompanied by typical LP lesions.1 It is important to monitor this condition, as squamous cell carcinoma3 and eccrine syringofibroadenoma4 have been known to arise in erosive palmoplantar LP lesions.
There have been numerous anecdotal reports of associations between erosive palmoplantar LP and autoimmune diseases such as primary biliary cirrhosis, autoimmune thyroiditis,5 diabetes mellitus, Sjögren syndrome, and rheumatoid arthritis, as well as other abnormalities, such as hypergammaglobulinemia, hypocomplementemia, and chronic liver diseases of infectious origin. Although it is accepted that the cellular immune response plays a key role in the pathogenesis of LP, the etiology and pathogenesis of erosive palmoplantar LP remain unknown.
Because erosive palmoplantar LP is chronic and resistant to both topical and systemic treatments, numerous treatment options have been proposed. Local treatments used to date, with variable results, include high-potency corticosteroids, retinoids, intralesional triamcinolone acetonide, topical ciclosporin,6 and psoralen–UV-A bath therapy.7 Topical tacrolimus 0.1% cream applied twice daily was recently shown to be effective in the treatment of ulcerative LP affecting mucous membranes.8
Oral treatments used to date include systemic corticosteroids, dapsone, etretinate, ciclosporin, mycophenolate mofetil, platelet-derived growth factor, griseofulvin, and thalidomide. Good response has been seen after 4 to 13 weeks of subcutaneous low-molecular-weight heparin (LMWH) administered at low doses (3mg/wk); LMWH inhibits the type iv hypersensitivity response that appears to be involved in the pathogenesis of LP.9,10
UV-A1 radiation (380-400nm), which induces apoptosis of CD4+ T cells, has proved to be an effective treatment in some cases. Extracorporeal phototherapy has also been effective in isolated cases.
Surgery, with or without immunosuppressive therapy with ciclosporin, has occasionally been effective against chronic, stable, localized cases of erosive palmoplantar LP.11
This case is remarkable for the patient's excellent response to conventional treatment with systemic corticosteroids and the absence of recurrence after 2 years, despite the fact that erosive palmoplantar LP is refractory to most available treatments. Nevertheless, because of the high recurrence rate associated with this disease, we consider that the patient should be monitored closely.
Please cite this article as: Jiménez-Sánchez MD, et al. Liquen plano erosivo plantar. Actas Dermosifiliogr.2012;103:448-50.