Capillary malformation is a condition included in the group of vascular malformations.1 It is one of the most common vascular abnormalities and can affect up to 0.3% of newborns.2,3 It presents clinically as a homogeneous erythematous macule with well-defined borders. It is typically unilateral and is usually present at birth. However, cases of acquired capillary malformation have been reported in patients with no previous lesions of this type.
Patient 1 was a 9-year-old girl followed-up from her first year of life for mastocytosis presenting as urticaria pigmentosa and treated with sodium cromoglycate and cetirizine. When she was 7 years old, a well-defined pink macule started to become visible, affecting segmentally the area of the first branch of the trigeminal nerve, and the superior part of the area of the second branch, with a more violaceous appearance in the periocular region. She presented no other lesions and there was no family history of interest. Skin biopsy revealed a capillary proliferation, negative for GLUT-1, consistent with a diagnosis of capillary malformation.
Patient 2 was a girl aged 8 years, with no past history of interest. She was referred to our clinic for macules on the left side of her face. The macules had first been noticed by her parents when the child was 4 years old, and they had grown progressively. Her parents stated that the macules became more evident in hot environments and after physical exertion. On examination, patchy pink macules were observed in a segmental distribution along the left body of the jaw and they were seen to become more intense after the patient performed physical exercise.
Patient 3 was a 7-year-old boy with no past history of interest. He was seen for a lesion in the right jaw region. His parents had first noticed the lesion when the child was about 4 years old. They stated that it had been asymptomatic, although its intensity increased with physical activity and with heat. On examination, a patchy pink macule with superficial telangiectasias was observed. The macule became more intense after the child performed physical exercise.
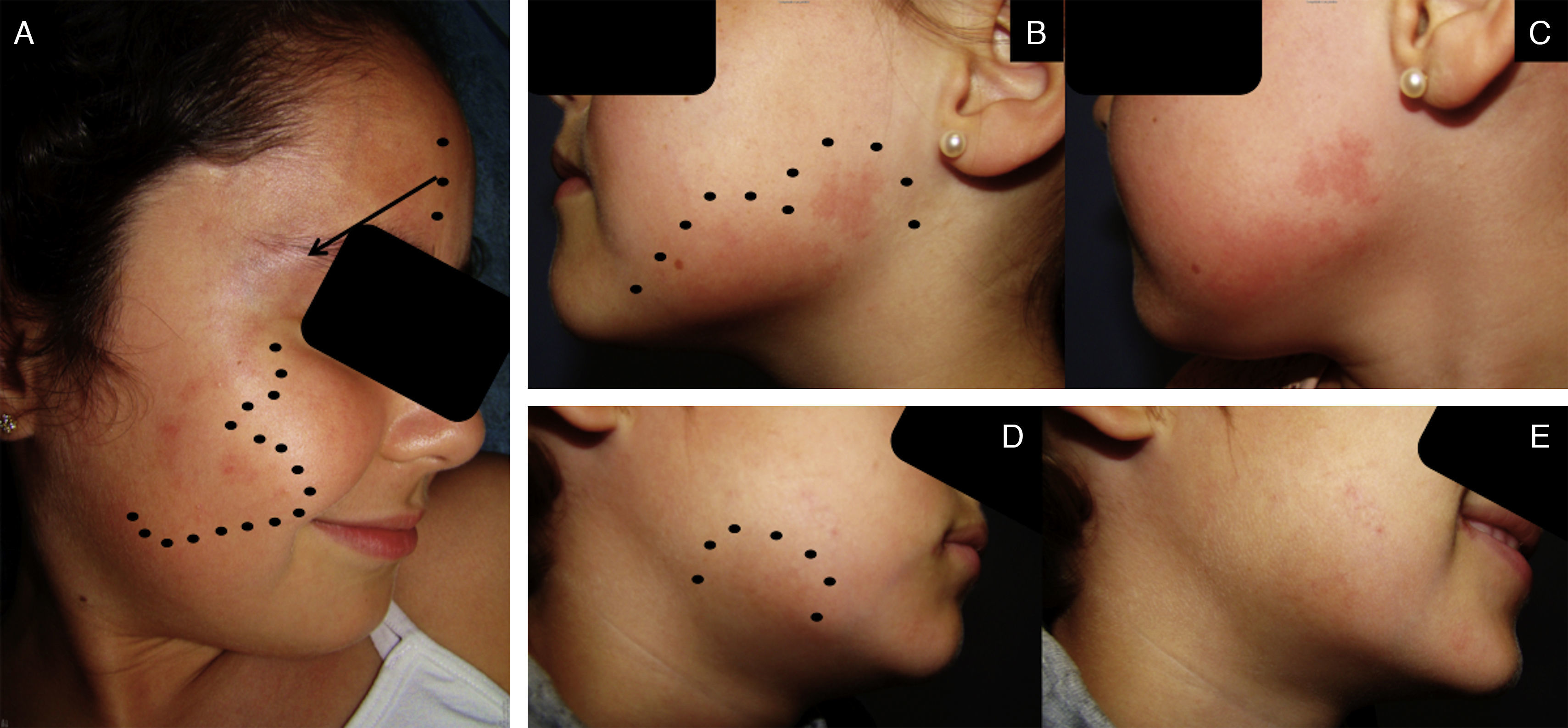
None of the 3 patients had any family history of interest or presented other lesions. Clinically there was no thrill and the lesions were not detectable on ultrasound. Photos of the children when they were younger were requested to check that the lesions had not previously escaped the parents’ attention. The children were referred to a reference center for laser treatment, which was only rejected by the third patient (Fig. 1).
A, Patient1. A reddish macule affecting the first and second branches of the trigeminal nerve (dotted line), with a more violaceous color in the periocular region (arrow). B, Patient2. Patchy pink macules (dotted line). C, More intense appearance of the lesions in B after the patient performed physical exercise. D, Patient3. Single macule of reddish color (dotted line). E, More intense appearance of the lesion in D after the patient performed physical exercise.
The immense majority of capillary malformations are present at birth or appear in the first years of life. Cases of acquired capillary malformations are rare and were first described in 1939 in a patient who had suffered spinal cord injury.4 Ten years later, Fegeler5 reported a new case of postraumatic capillary malformation, which has been named Fegeler syndrome since that time. The etiological factors that can trigger their de novo appearance have not been identified, though a history of trauma is present in up to a third of cases. Previously it has been proposed that the appearance of congenital capillary malformations could be due to a deficit of sympathetic innervation (responsible for vasoconstriction), leading to vascular ectasia that presents as this vascular malformation.6 Acquired cases associated with spinal trauma conform to this hypothesis. Other possible etiologies have also been proposed, such as estrogenic impregnation, either during pregnancy or in the pubertal-adult period.7,8 In some isolated cases, capillary malformations have been related with drugs, herpes zoster, sun damage, cluster headaches, and acoustic neuroma.7,8 In a capillary malformation of the port wine stain type, the possibility of a postnatal mutation of the GNAQ gene might also be considered.9 Despite these proposals, no triggering event has been discovered in many cases. The age at onset reported in the literature varies between 3 and 69 years, with a mean age of 25 years. Lesions most often arise on the face and upper limbs, and they have not been associated with other malformations or skin lesions. Typical and acquired capillary malformations are histologically and morphologically indistinguishable.
The differential diagnosis based on the type of vascular lesion is extensive. But perhaps it is most important to rule out this lesion as part of a syndromic diagnosis associated with more serious repercussions than the purely cosmetic. These include capillary malformation-arteriovenous malformation syndrome (a family history of similar lesions or of arteriovenous malformation is usually detected, the capillary malformations are multiple, with a browner color, increased local temperature, a whitish peripheral halo, and possibly with arterial flow visible on ultrasound) and Sturge-Weber syndrome (lesions that affect one side of the face, but that are usually present at birth).3,10
In summary, acquired capillary malformation may be considered simply to be a late-onset capillary malformation with a variable latency period.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Millán-Cayetano JF, del Boz J, García-Montero P, de Troya-Martín M. Malformación capilar adquirida (síndrome de Fegeler): 3 casos. Actas Dermosifiliogr. 2017;108:954–955.