Schnitzler syndrome is a rare entity, with around 250 cases reported to date.1 It is characterized by the presence of an urticarial rash associated with a monoclonal gammopathy, together with recurrent episodes of fever, joint pain, generalized bone pain, lymphadenopathy, hepatosplenomegaly, and bone changes.2,3 Although its etiology and pathogenesis remain unknown, an excellent response to interleukin (IL)1 inhibitors has been observed, and absence of a response should lead us to reconsider the diagnosis.4
A 63-year-old woman with no family history of interest and who reported undiagnosed bone and joint pain since 2001, was seen in 2007 for an 18-month history of fleeting, slightly pruritic skin lesions on her trunk and limbs, with no fever or other associated systemic symptoms. She had not identified any etiological or pathogenic agents.
There were no relevant findings on examination and she presented a good general state of health. Dermographism was negative. No goiter, palpable peripheral lymph nodes, or hepatosplenomegaly were detected.
Complete blood count, erythrocyte sedimentation rate, general biochemistry including electrolytes, liver and kidney function tests, antinuclear antibodies, complement (C3 and C4), thyrotropin, protein electrophoresis, immunoglobulin (Ig) levels (IgG, IgA, IgM, IgE), and tumor markers were normal or negative. No abnormal findings were detected on plain chest x-ray or abdominopelvic ultrasound. C-reactive protein was 87.5.
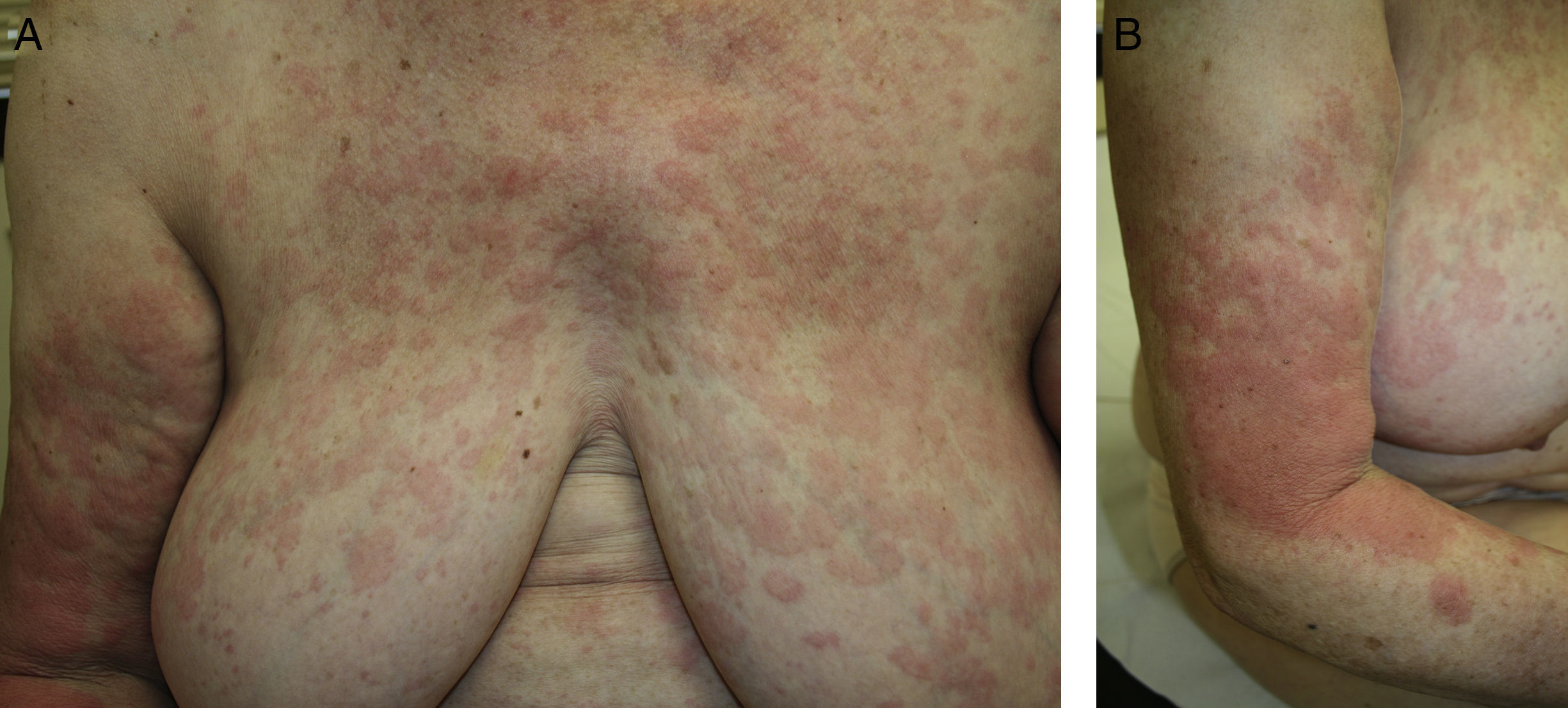
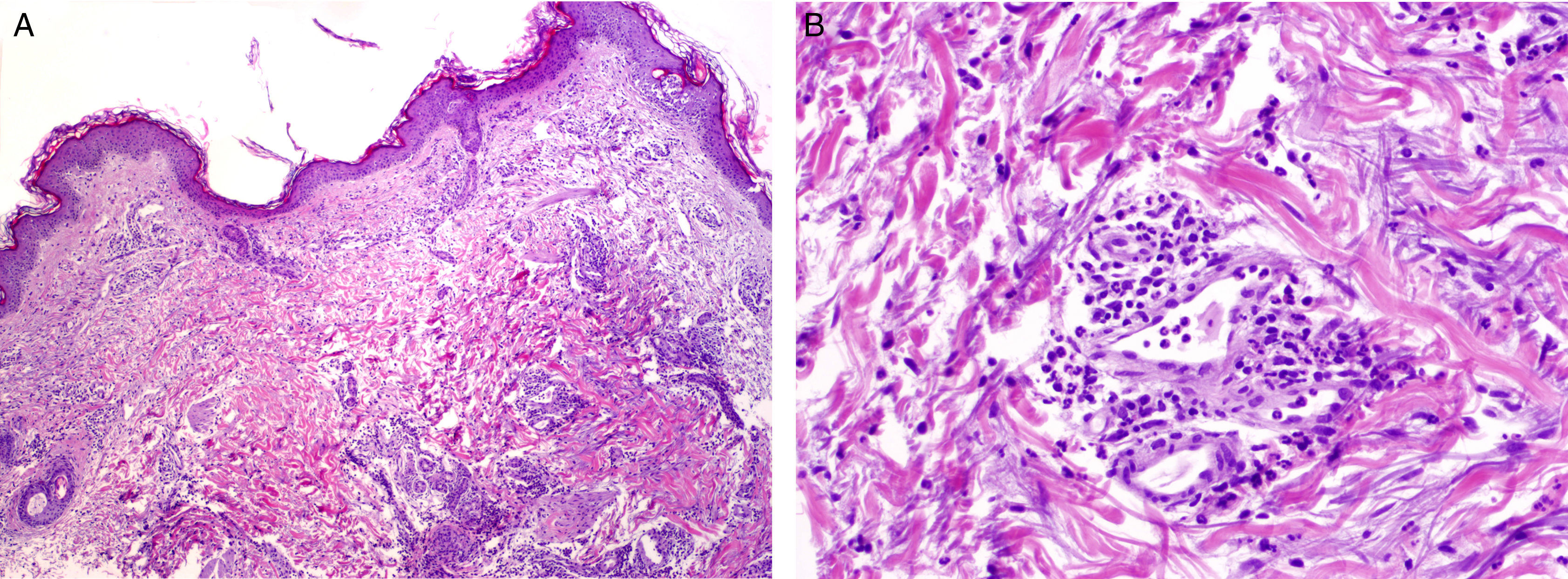
With a diagnosis of chronic idiopathic urticaria, treatment was started with oral antihistamines with a poor response. In January 2009, the patient developed recurrent spikes of fever that lasted 2 to 3 days and were associated with intense generalized bone pain and the appearance on her trunk and limbs of well-defined, edematous pink lesions that resolved in less than 24hours leaving no residual lesion (Fig. 1, A andB). Skin biopsy revealed a superficial and deep perivascular infiltrate formed of neutrophils, affecting the interstitium (Fig. 2A), with leukocytoclasia without vasculitis (Fig. 2B). In addition, a focal neutrophilic infiltrate was observed around the eccrine glands, both at the level of the epidermis and around the dermal duct.
Blood tests revealed neutrophil leukocytosis and elevation of the acute phase reactants. Antinuclear antibodies, C3, C4, ferritin, rheumatoid factor, serology for hepatitis B and C viruses, and cryoglobulins remained normal or negative. In September 2009, a monoclonal IgM-κ band of 2.61 was detected (upper limit of normal, 2.30), enabling us to make a diagnosis of Schnitzler syndrome.
Sequential treatment was started with colchicine, 100mg/d, oral prednisone, 0.5mg/kg/d, dapsone, 50mg/d, and methotrexate, 15mg/wk, with no improvement. In 2010, the patient commenced treatment with subcutaneous anakinra, 100mg/d, leading to complete resolution of all her symptoms, including the nonspecific bone pain, within a week of starting treatment. The acute phase reactants normalized and no complications have arisen. At the time of writing, the monoclonal IgM-κ band persisted at levels between 2.40 and 2.85. Attempts to withdraw anakinra have led to immediate recurrence of the patient's symptoms, and she is currently asymptomatic on subcutaneous anakinra at a dose of 100mg every 48hours.
The first case of Schnitzler syndrome was reported in 1972 by Liliana Schnitzler. It is now considered the paradigm of acquired or late-onset autoinflammatory diseases.1 The diagnostic criteria were proposed by Lipsker et al.2 in 2001 and are still used with minor modifications made at the expert meeting in Strasbourg in 2012. It is a diagnosis of exclusion.
The presence of an urticarial rash is an obligate criterion for the diagnosis of Schnitzler syndrome.5 Histologically, the syndrome is included in the group of neutrophilic urticarial dermatoses, and leukocytoclasia is a constant finding.6,7 Involvement of the eccrine ducts by the neutrophils, as found in our patient, has been reported as an epiphenomenon, and the presence of an intraepidermal neutrophilic infiltrate has recently been proposed as a marker of the neutrophilic dermatoses.6,8 Vasculitis is observed in 20% of cases,3 but this is questioned by some authors4 who have critically reviewed biopsies and a number of literature reports and have found no clear evidence of vasculitis.
The other major diagnostic criterion is the presence of a monoclonal IgM-κ band, observed in 90% of cases,2 although an IgG variant has also been described.3 The minor diagnostic criteria include fever, joint pain and arthritis, bone pain, palpable lymphadenopathy, hepatosplenomegaly, elevation of the erythrocyte sedimentation rate, leukocytosis, and x-ray changes.2,3
The two main complications reported during the course of the disease are AA amyloidosis and lymphoproliferative disorders. These develop in approximately 10% of patients.
Although the etiology and pathogenesis of Schnitzler syndrome remain unknown, the rapid response of the majority of patients to anakinra, an IL-1 receptor inhibitor, and more recently to canakinumab, an IL-1β inhibitor, would suggest a pivotal role for this interleukin in the etiology and pathogenesis of the disease and a relationship with cryopyrine-associated periodic syndromes.8,9 A mutation in the NLRP3 gene has been detected in some cases; that study was not performed in our patient. Although patient follow-up of up to 35 years has been reported, the relatively recent introduction of anakinra to the treatment of this disease means we cannot yet determine if it will reduce the frequency of blood dyscrasias, although a reduction in the frequency of amyloidosis is assumed.3,10
We consider it important to report this case to draw attention to diagnostic difficulty of this syndrome and the need to follow-up atypical presentations, given the progressive appearance of symptoms and of alterations in the blood tests.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Hidalgo-García Y, García-Fernández E, Palacio-Aller L, Gonzalvo P. Síndrome de Schnitzler con respuesta a anakinra en monoterapia: 7 años de seguimiento. Actas Dermosifiliogr. 2017;108:956–958.