Dermal melanocytosis is a group of congenital or acquired entities, characterized clinically by bluish-gray discoloration of the skin, and histologically by the presence in the dermis of pigmented spindle and dendritic melanocytes.1 The etiology and pathogenesis are unclear.2
Facial forms of dermal melanocytosis have been described, including nevus of Hori, nevus of Ota, nevus of Hidano, periorbital melanosis (as proposed by Watanabe), and nevus of Sun.1 Sun et al. reported 110 cases of nevus fusco-caeruleus zygomaticus in Chinese patients.3 This lesion consists of small speckled patches of skin ranging in color from brown to gray to blue, principally affects the zygomatic region, appears gradually between the second and third decades of life, and is 12.8 times more prevalent in women than men. Familial cases with an autosomal dominant inheritance pattern have been described.3,4 There is no known association with other dermatoses.5 Histology shows dispersed elongated melanocytes in the upper dermis, as visualized with Fontana-Masson and 3,4-dihydroxyphenylalanine (DOPA) staining or by immunohistochemistry for S100 and HMB-45.2 Here, we describe a case of acquired dermal melanocytosis corresponding to nevus of Sun.
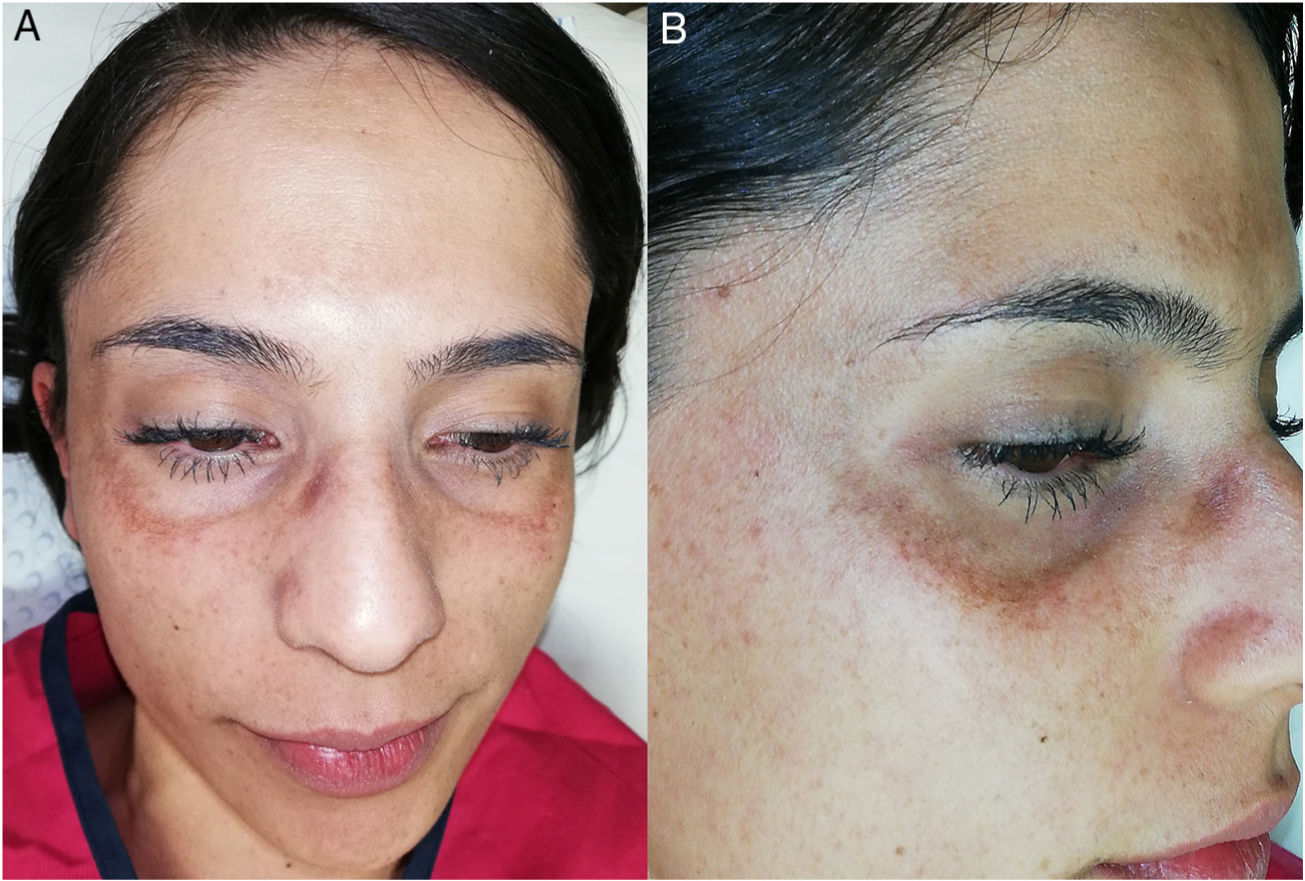
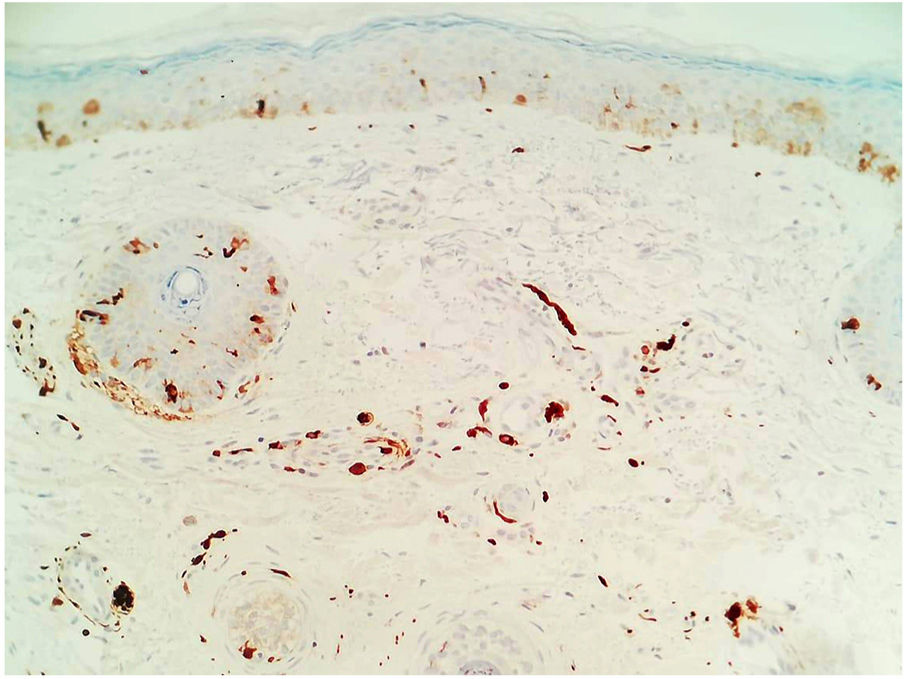
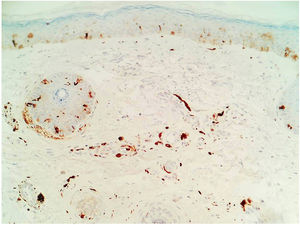
A 27-year-old woman presented with asymptomatic hyperpigmented patches in the zygomatic region that had appeared 3 years earlier. Since the appearance of the lesions, she had been evaluated by 4 dermatologists, all of whom had established a diagnosis of melasma. The patient had undergone treatment with hydroquinone, high- and medium-potency steroids, kojic acid, intralesional tranexamic acid, and chemical and physical photoprotection, without improvement. Physical examination revealed dermatosis in the bilateral zygomatic region, below the lower palpebral border, consisting of well defined, speckled, grayish-brown macules of less than 4mm diameter that showed a tendency to coalesce (Fig. 1A and B). A clinical diagnosis of acquired facial dermal melanocytosis was established, and a biopsy was taken. Histology (hematoxylin-eosin staining) revealed the presence of pigmented spindle cells distributed in the upper, perivascular, and periadnexal dermis. These cells, which were positive for S100 protein, were identified as dermal melanocytes (Fig. 2). Based on these findings, the diagnosis of nevus-of-Sun-type acquired facial dermal melanocytosis was confirmed.
The main differential diagnosis is melasma, owing to its prevalence in the Spanish population. Clinically, melasma manifests as brown or grayish patches on the face that are usually uniform in color, rarely mottled, and never affect the periorbital area.6 Histology shows hyperpigmentation of the basal layer, rupture of the basement membrane, melanophages in the dermis, an increase in the number of vessels, mast cells, and solar elastosis.7,8 By contrast, nevus of Sun affects the zygomatic area and is characterized by hyperpigmented, speckled, brown or gray-blue macules. Histology shows elongated, pigmented spindle cells in the upper dermis that correspond to dermal melanocytes positive for S100 protein.3 Other conditions that should be ruled out include ephelides, Riehl melanosis, ashy dermatosis, ochronosis,1 agminated dermal melanocytosis,9 and other forms of acquired facial dermal melanocytosis.7 Treatment consists of physical and chemical photoprotection, although some cases have been treated with Q-switched Alexandrite laser.4,10 On the American continent, a case of nevus of Hori was described in an Argentine woman of Japanese descent.1
Based on a review of the literature and the shared clinical and histopathological similarities, we propose grouping these pigmentary dermatoses within a single category; acquired facial dermal melanocytosis. It is highly likely that this type of facial hyperpigmentation is underdiagnosed due to confusion with other more common dermatoses, as occurred in the present case.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Marín Hernández E, Calderón Ponce de León Y, Bautista Piña V, Sánchez Rodríguez L. Melanocitosis dérmica facial adquirida tipo nevo de Sun. Reporte de un caso. Actas Dermosifiliogr. 2020;111:337–338.