Dermal melanocytosis refers to the presence of dendritic melanocytes in the dermis containing abundant quantities of pigment but without melanocytic proliferation at the dermal-epidermal junction. In addition to the classic morphologic variants, which include blue nevi, Mongolian spots, and nevi of Ota and Ito, there are atypical variants. Dermal melanocytosis is common in Asians and can be present at birth or appear later in adolescence or adulthood.1 We present a case of acquired dermal melanocytosis on the back of a patient with psoriasis.
The patient was a 39-year-old Peruvian man with plaque psoriasis diagnosed in 2008. In January 2011, he presented at our department with a major psoriasis flare-up that was brought under control with oral methotrexate in addition to calcipotriol and topical betamethasone for 4 months.
The patient returned in July 2014 with a mild flare-up, which was resolved with a short cycle of calcipotriol and betamethasone ointment.
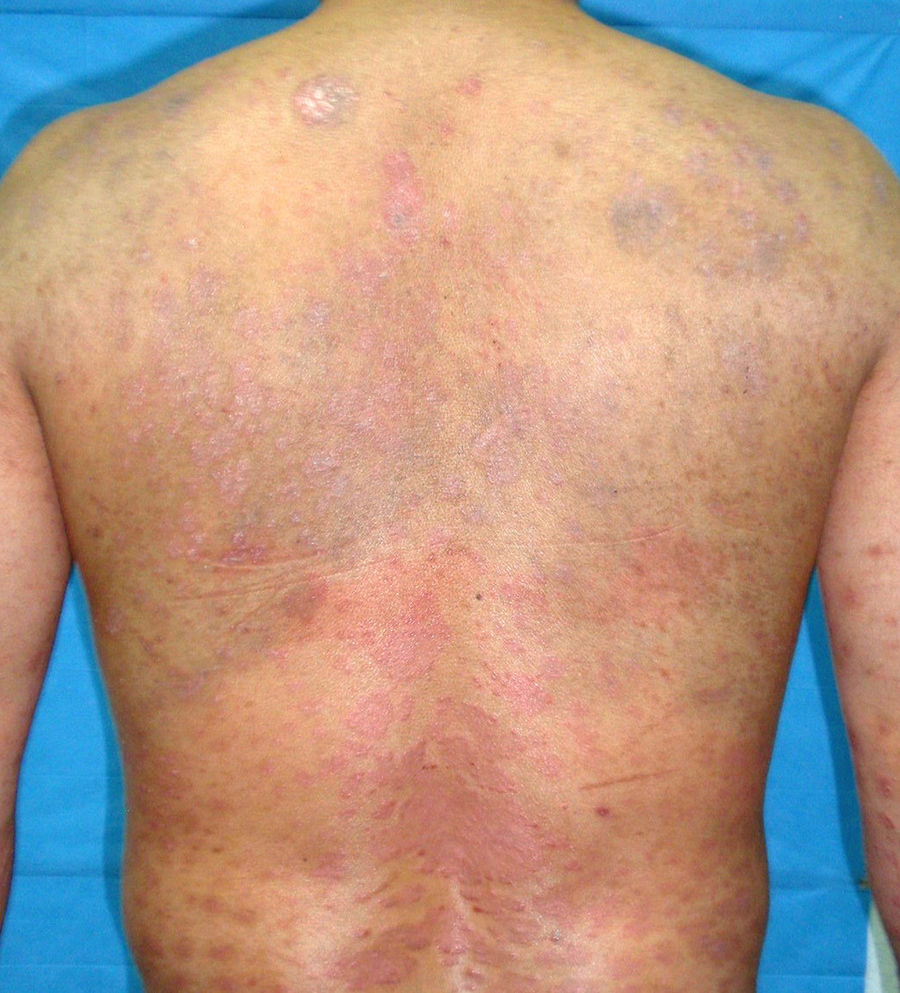
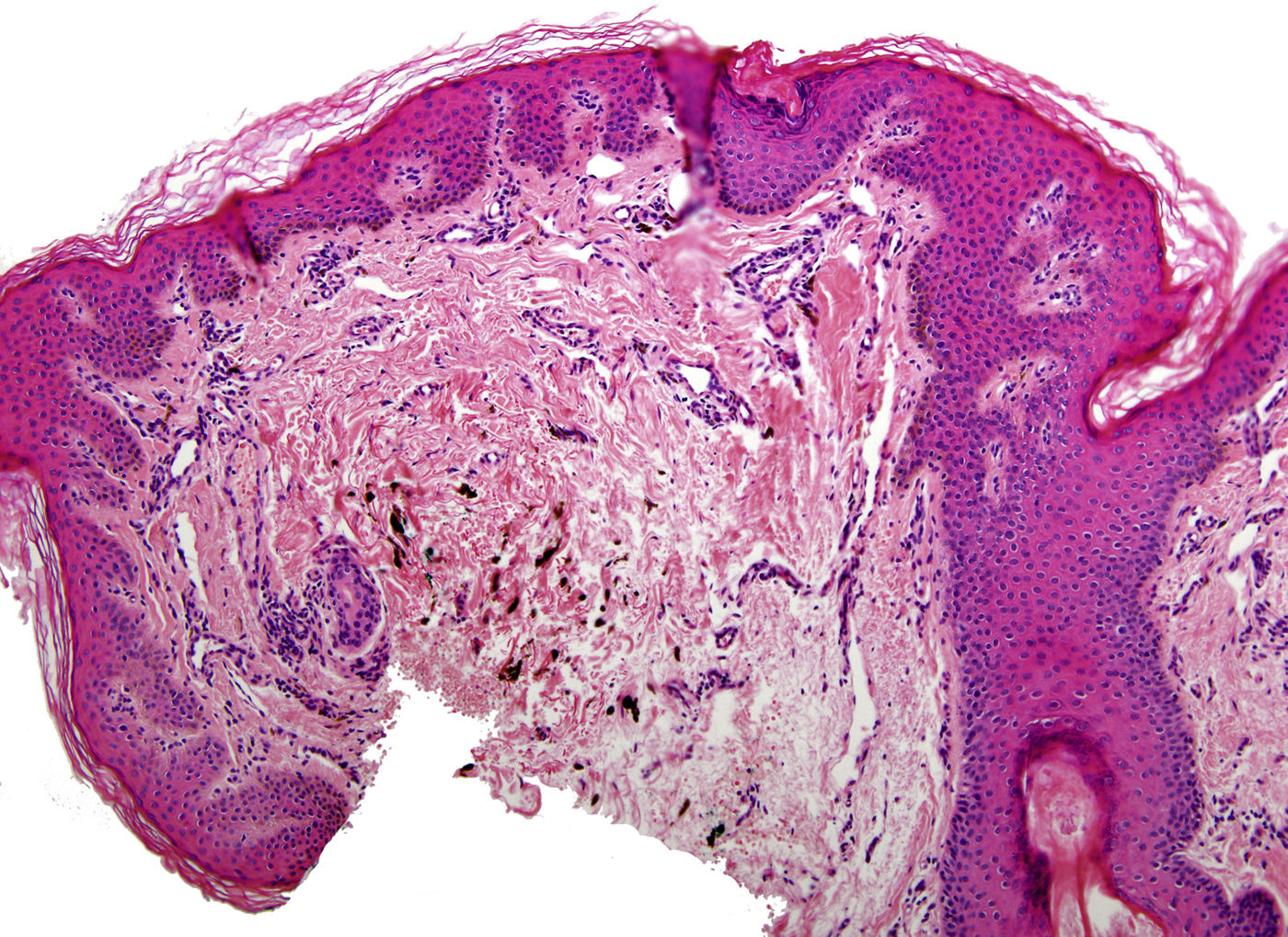
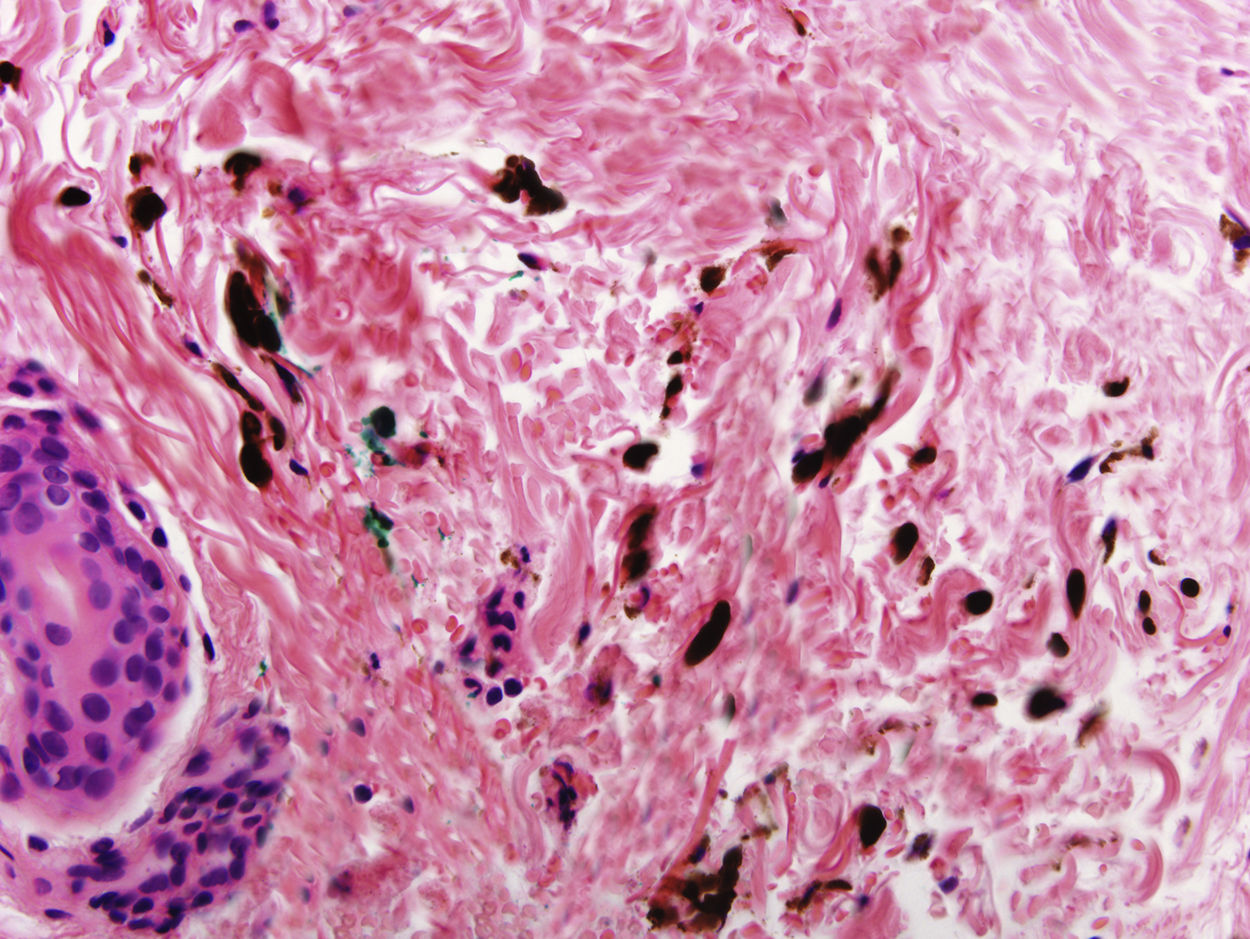
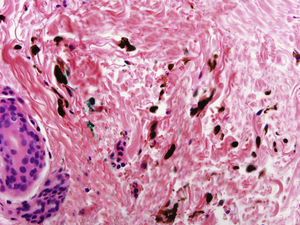
In addition to psoriasis plaques, the physical examination showed multiple grayish-blue macules with a patchy distribution in the upper and mid dorsal region that had not been present in previous clinical examinations (Fig. 1). Similar lesions in other locations were ruled out. Histopathology showed acanthosis and papillomatosis in the dermis. Spindle cells with melanin scattered among collagen bundles were observed in the mid dermis (Figs. 2 and 3). Immunohistochemical staining with SOX-10 showed nuclear positivity. HMB-45 and Melan A staining could not be performed because of the marked presence of cytoplasmic melanin. Integration of clinical, anatomopathologic, and immunohistochemical findings led to a diagnosis of dermal melanocytosis.
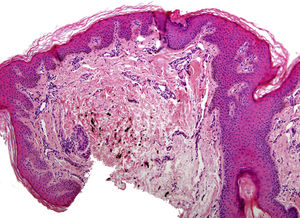
In October 2014, the patient experienced a new, more serious, psoriasis flare-up that showed excellent response to 2 months of treatment with oral ciclosporin. Examination of the dorsal region showed progression of the dermal melanocytosis, with more extensive skin involvement and greater pigmentation (Fig. 4).
Dermal melanocytosis was described by Mevorah et al.2 in 1977. The term refers to a group of entities that are characterized histologically by dendritic melanocytes in the dermis and clinically by grayish-blue macules.3 Theories for their origin include the descent of melanocytes from the epidermis or hair bulb to the dermis and reactivation of latent melanocytes in the dermis due to improper migration from the neural crest to the epidermis.1,4,5 The higher incidence observed in the Japanese population and observation of familial cases suggest a role for genetic factors in the etiology and pathogenesis of dermal melanocytosis.6,7 Several reactivation triggers have been proposed, namely, solar radiation, local inflammation, trauma, medication, and hormonal therapy with estrogens and/or progesterone, among others.3 In addition, a recent report described the appearance—and progression—of dermal melanocytosis lesions in patients with chronic myeloid leukemia and gastrointestinal stromal tumors treated with imatinib.8
A possible association between latent melanocytes and certain triggers is supported by the observation of dermal melanocytes in areas of normal skin adjacent to the pigmented area in melanocytosis.6
Dermal melanocytosis has also been described in patients without reactivation triggers. Ríos-Martín et al.,3 for example, described the case of a 49-year-old woman who developed a bluish-gray macule in the right dorsal region without any clear triggers.3
Interaction between melanocytes and collagen and elastic fibers has also been highlighted as an important etiologic and pathogenic factor in dermal melanocytosis. Ultrastructural studies have shown an extracellular sheath containing these fibres around dermal melanocytes.7 The sheaths have been found to fade in involuted Mongolian spots but to persist in acquired dermal melanocytosis.7
The anatomic distribution of atypical dermal melanocytosis is variable, with reports of cases involving the dorsal region,7,9 extremities,10 hands,4,5 and nose,10 among others.
Two authors have reported similar cases to ours in which the patients developed dermal melanocytosis. One of the patients had been treated with psoralen plus UV-A therapy while the other had received infliximab.11 In our patient, dermal melanocytosis was first observed in July 2014, although it could have developed earlier, as there was no follow-up after the 2011 flare-up treated with oral methotrexate and calcipotriol with topical betamethasone.
Postinflammatory hyperpigmentation was an important consideration in the differential diagnosis in the current case given the patient's history of plaque psoriasis in the area of the melanocytosis. Histologic examination of the plaque, however, showed hyperpigmentation in the basal layers and melanophages in the dermis, while examination of the acquired dermal melanocytosis lesions showed a predominance of scattered melanocytes with a characteristic morphology in the reticular dermis that may sometimes be accompanied by melanophages.1,12
Our patient may have been genetically predisposed to dermal melanocytosis and there may already have been dermal melanocytes in this area. However, the presence of accentuated melanocytes after the psoriasis flare-ups and the patchy distribution on the back, with sparing of mucous membranes, suggest a pathogenic role for inflammation in this uncommon entity.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank the patient for providing written consent for the publication of the images in this study.
Please cite this article as: Flores L, Burillo-Martínez S, Rodríguez Peralto JL, Rivera-Díaz R. Melanocitosis dérmica adquirida de la espalda en un paciente con psoriasis. Actas Dermosifiliogr. 2018;109:839–841.