Muscle hernia (MH), also called myofascial herniation, is caused by a defect in the fascia that envelops the muscle, giving rise to a focal protrusion of muscle tissue. It is a disease that is rarely encountered in dermatology consultations and can be diagnosed by the dermatologist by means of ultrasound.
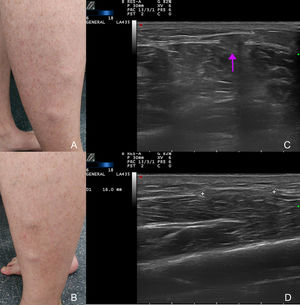
The first case is a 34-year-old man with no relevant past medical history, who presented with lumps on the sides of the legs. The lesions had appeared 7 years earlier and had increased in number and size. They were not associated with injuries. The patient reported stabbing pain after walking for long periods. Physical examination revealed several soft nodules that could be compressed on palpation; the nodules were more evident when the patient was standing or on resisted dorsiflexion of the foot in the supine decubitus position (Figs. 1A and B). The ultrasound examination was performed using a variable-frequency (8-18MHz) linear probe connected to a MyLab Class C device (Esaote) in B-mode, with the patient in the standing and supine decubitus position. When the patient was standing, B-mode ultrasound showed a partial protrusion of the tibialis anterior through a defect in the muscle fascia; the protrusion disappeared when the patient was in the supine decubitus position (Figs. 1C and D). The patient was advised to use compression measures and to return if the protrusion grew or he suffered discomfort.
A, Nodules on the side of the right leg. B, Nodules on the side of the left leg. C, B-mode ultrasonography: protrusion of the muscle during contraction, through the defect in the fascia (arrow). D, B-mode ultrasonography: discontinuity of the fascia during muscle relaxation (between markers).
The second case is a 47-year-old woman with no relevant past medical history who visited the dermatologist with a raised asymptomatic lesion on the right forearm; the lesion had appeared 4 years earlier. The lesion was not associated with injury or other triggers. The lesion grew initially and then stabilized. Physical examination revealed a soft nodule that could be compressed on palpation (Fig. 2A). Dynamic ultrasonography was performed with the same equipment used in the previous case and showed discontinuity of the fascia of the flexor carpi ulnaris; the discontinuity was more evident on flexion and adduction of the hand (Figs. 2B and C). No treatment was required.
Table 1 summarizes both cases and includes another, previously published, case.1
Clinical and Ultrasound Characteristics of the Clinical Cases of Muscle Hernia.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Sex | Male | Female | Male |
| Age, y | 34 | 47 | 14 |
| Site | Side of both legs | Right forearm | Side of right leg |
| Triggers | No | No | No |
| Time since onset, y | 7 | 4 | 2 |
| Physical examination | Soft, compressible nodules of different sizes | Soft, compressible nodule | Soft, compressible nodule |
| More evident on muscle contraction | Yes | Yes | Yes |
| Unilateral/bilateral | Bilateral | Unilateral | Unilateral |
| Solitary/multiple | Multiple | Solitary | Solitary |
| Clinical presentation | Paresthesia | Asymptomatic | Asymptomatic |
| Clinical course | Increase in number and size | Stable | Stable |
| Ultrasound B-mode | |||
| Echostructure | Isoechoic with muscle | Isoechoic with muscle | Isoechoic with muscle |
| Discontinuity of the muscle fascia | + | + | + |
| Color Doppler imaging | − | − | − |
| Muscle involved | Tibialis anterior | Flexor carpi ulnaris | Tibialis anterior |
| Treatment | Conservative management | Not required | Not required |
MH is caused by a focal defect in the muscle sheath; the defect may be congenital or acquired. Congenital causes include regions where the sheath is perforated by nerves and blood vessels, and general weakness of the fascia. Acquired causes tend to be the result of direct or indirect injury.2
The most common site for MH of the extremities is the legs. The knowledge base regarding this entity is attributed to Hugo Ihde.3 The incidence of muscle hernia in the legs is unknown, but this entity may be underdiagnosed. Those most at risk are athletic men, in whom the tibialis anterior muscle is most commonly involved.4
The few reported cases of hernias in the forearm involve symptomatic cases. They are mostly located in the proximal half of the ventral surface of the muscle.5 They occur predominantly in men and the most common cause is injury.6
MH may manifest clinically as a subcutaneous nodule or a soft-tissue tumor. The lesion may be asymptomatic or cause weakness, discomfort, and pain, which may worsen with physical activity and in certain positions. Hernias may be solitary, multiple, or bilateral.4
When presented with a soft, palpable lump under the skin, the differential diagnosis should include varicose veins, hematomas, arterial or venous malformations, muscle tearing (pseudohernia), and soft-tissue tumors.4 It is important to examine the lesion when the muscle involved is contracted, as an increase in size indicates a suspected diagnosis of MH. The diagnosis can be confirmed by means of ultrasonography or nuclear magnetic resonance (NMR). Ultrasound should be the technique of choice, as it is noninvasive, is performed in real time, and is inexpensive; NMR should be reserved for doubtful cases.7,8 When examined using ultrasound, normal muscle fascia is thin and echogenic. In mild cases of MH, the fascia is thinner than normal and the slight muscle protrusion raises the overlying fascia. When MH is evident, the fascia shows a defect with clearly defined limits through which the external herniation of the muscle occurs. Ultrasound in B-mode, using a high-frequency linear probe, may confirm the diagnosis by showing discontinuity of the muscle fascia with protrusion of the muscle; this will be more evident if the muscle is contracted and dynamic images should therefore be taken (with the involved muscle contracted and relaxed). The probe should be applied lightly to avoid reducing the hernia.8
Asymptomatic hernias do not require treatment. Conservative management is recommended in the case of mild symptoms and surgery in more severe cases, although there is no consensus regarding the most appropriate technique. Longitudinal fasciotomy appears to be the safest option in hernias in the leg because it prevents compartment syndrome.4
In conclusion, in these 2 new cases of MH, we highlight the importance of ultrasound as the technique of choice for diagnosis of the entity, thereby avoiding unnecessary biopsies and allowing for appropriate management.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sigüenza-Sanz M, Alfageme-Roldán F, Salgüero-Fernández I, Roustan-Gullón G. Hernias musculares: utilidad de la ecografía en el diagnóstico con un enfoque dermatológico. Actas Dermosifiliogr. 2018;109:842–844.