Syphilis, traditionally known as the great imitator remains among us and requires maintaining a high level of diagnostic suspicion. As well as its usual forms of clinical presentation, extremely rare skin manifestations may appear that sometimes make diagnosing this entity difficult.1 Condyloma latum (CL) is a classic, though rare, cutaneous manifestation of secondary syphilis.2 The increased incidence of syphilis may lead to an increase in the number of cases with atypical presentation,1 such as those we describe below.
In this study, we collected all the cases of CL diagnosed in the STI unit of the dermatology department of Hospital General de Valencia, Valencia, Spain, between January 2015 and January 2019. In this period, a total of 95 cases were diagnosed, 49.5% of which (47 cases) were secondary syphilis. Of these, 11 cases (23.4%) showed CL in the anogenital region. We found CL with white spots on the surface in only 5 patients diagnosed with syphilis in this time. The characteristics of these patients are shown in Table 1.
Clinical and Epidemiologic Characteristics of the Study Patients.
| Patient | Age, Y/Sex | Previous Diagnosis | Sexual Orientation | Previous STIs | Associated Clinical Presentation | RPR on Diagnosis | TP PCR | HPV Genotypes | Treatment | Clinical Course |
|---|---|---|---|---|---|---|---|---|---|---|
| 1(Fig. 1A). | 27/male | CA | MSM | — | — | 1/8 | Not performed | — | Penicillin G benzathine 2.4×106IU | RPR 1/1. Clinical cure |
| 2 (Fig. 1B). | 24/male | CA | MSM | — | Evanescent maculopapular rash, depapillated tongue, swollen lymph nodes in the groin | 1/32 | Positive | HPV 6 in anal swab (after 1year of follow-up, patient developed perianal condylomata acuminata) | Penicillin G benzathine 2.4×106IU | RPR negative. Clinical cure |
| 3 (Fig. 1C). | 36/male | CA | MSM | HIV, condylomata acuminata | Perianal CA | 1/64 | Positive | HPV 6 (in condyloma acuminatum lesion) | Penicillin G benzathine 2.4×106IU/3 doses | RPR negative. Clinical cure |
| 4 (Fig. 1D). | 39/male | CA | MSM | HIV | CA, papillomatous tumor in anal canal | 1/64 | Positive | HPV 16, 62, 72, 81 (epidermoid carcinoma of anal canal) | Penicillin G benzathine 2.4×106IU/3 doses | RPR negative. Clinical cure |
| 5 | 29/male | Perianal genital herpes | MSM | HIV, condylomata acuminata | Maculopapular rash | 1/128 | Positive (also in pharyngeal exudate) | — | Penicillin G benzathine 2.4×106IU/3 doses | RPR negative. Clinical cure |
Abbreviations: CA indicates condyloma acuminatum; MSM, man who has sex with men; STIs, sexually transmitted infections; PCR, polymerase chain reaction; RPR, rapid plasma reagin test; TP, Treponema pallidum; HIV, human immunodeficiency virus; HPV, human papillomavirus.
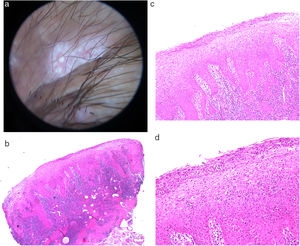
In the physical examination, the 5 patients presented a notable lesion in the perianal region (Fig. 1). This lesion was raised, with pink fleshy edges surrounding a friable erythematous center with characteristic white spots on the surface. Dermoscopy revealed a lesion with milky-red areas in the center and well-defined pearly globules in the center (Fig. 2A). In Case 1, this lesion was the patient’s only clinical sign. In Cases 3 and 4, this lesion was accompanied by perianal condylomata acuminata (CA).
A, Dermoscopy of the condyloma latum lesion of Case 5, showing 2 rounded white spots with well-defined edges, on a milky-red central area. B, Histology of a condyloma latum lesion showing a psoriasiform hyperplasia of the epidermis with marked exocytosis and formation of neutrophilic spongiform pustules, accompanied by a dense lymphoplasmacytic dermal infiltrate.
Biopsies were performed in 2 of the cases to confirm the diagnosis of CL. The characteristics of both samples are very similar, with a psoriasiform hyperplasia of the epidermis with marked exocytosis and formation of spongiform pustules, accompanied by a dense lymphoplasmacytic dermal infiltrate (Fig. 2B-D). Immune staining with anti-Treponema pallidum antibodies was positive in both patients.
In the 2 patients with suspected coinfection with the human papillomavirus (HPV), samples were taken for histopathology and genotyping of the virus. One of the patients developed epidermoid carcinoma of the anal canal. Another patient developed perianal CA after a year of follow-up.
CL is a rare pseudotumoral manifestation of secondary syphilis, with an incidence of between 5% and 22%, depending on the series.3 In our series, the incidence of CL was 23% of patients diagnosed with secondary syphilis, in relation to studies published in the literature. In other series, prevalence may reach 50%.4 These lesions are typically defined as plaques or nodules in the anogenital region, with a smooth, flat, or papillary moist surface.5 Location outside the genital region has rarely been reported.6,7 These lesions may be verrucous or pediculated, thus mimicking other diagnoses, such as CA, Bowen disease, anal epidermoid carcinoma, hemorrhoids, or lymphogranuloma venereum.8
The pathogenesis of these lesions is unknown, although their location in moist areas subject to constant friction may be responsible for the transformation of syphilitic papules to CL.9
Our series of 5 patients is characterized by flat, raised lesions with an erythematous friable center with clinically visible disperse white spots. These spots are more evident under dermoscopy and appear pearly, rounded, and with clearly defined edges. We have found no other cases of CL that present such clinically characteristic findings. Dermoscopy of CL, however, has been described and reveals multiple small, whiteish, rounded structures in the center of the lesions.6
Histopathology of 2 of these lesions showed a psoriasiform hyperplasia of the epidermis with marked exocytosis and formation of spongiform pustules, accompanied by a dense lymphoplasmacytic dermal infiltrate. This is similar to cases reported in the literature.6,10 However, we have found no reports showing spongiform pustules in CL lesions.
Furthermore, coinfection with HPV was found in 3 of the 5 patients, 2 of them with clinical lesions of CA that even masked the CP lesion. This coinfection may be a pathogenic factor in the development of these lesions.
The statement of Sir William Osler notwithstanding, we believe that syphilis is not the only disease one needs to understand in order to become an expert dermatologist.1 However, the fact that it can simulate any disease forces us to be cautious and to keep this diagnosis in mind, even when it begins with clinically rare manifestations. CL may occasionally be the only manifestation of the disease, and it is therefore important to retain a high degree of suspicion. In conclusion, we present the whiteish spots of syphilitic CL as a novel important clinical finding for being able to make an accurate diagnosis and prescribe appropriate treatment.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Magdaleno-Tapial J, Hernández-Bel P, Valenzuela-Oñate C, Alegre-de Miquel V. Puntos blanquecinos como clave diagnóstica de condilomas planos: reporte de 5 casos. Actas Dermosifiliogr. 2020;111:892–895.