A 9-year-old boy with a past history of atopic dermatitis and attention deficit and hyperactivity disorder, who was undergoing treatment with methylphenidate and risperidone, visited our department with asymptomatic lesions in the oral cavity that had appeared 7 months earlier; the lesions had been treated with topical antifungal agents (ketoconazole and nystatin), with no improvement.
Physical ExaminationThick, rough, white plaques that did not detach on scraping were found in the oral cavity, involving the mucosa of both cheeks, the floor of the mouth, and the lateral edges and ventral region of the tongue (Fig. 1). The rest of the physical examination was normal.
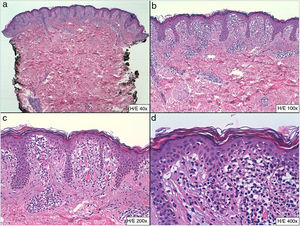
HistopathologyAn incisional biopsy of the buccal mucosa was taken. Staining with hematoxylin–eosin revealed a squamous mucosa with acanthosis and clear cells corresponding to keratinocytes with abundant clear cytoplasm and a small nucleus and foci of a perinuclear cytoplasmic eosinophilic material. The cell wall showed no inflammatory infiltrate (Fig. 2). PAS staining revealed no mycotic structures.
Other TestsMycology culture was negative. Blood tests revealed elevated urea (356 mg/dL), and other biochemistry parameters, blood count, complement, and immunoglobulin levels were normal. The serologic study (EBV, Mycoplasma pneumoniae, parvovirus B19, CMV) showed findings compatible with past infection (IgG positive) by EBV and Parvovirus B19.
[[?]]What is your diagnosis?
DiagnosisWhite sponge nevus.
Clinical Course and TreatmentA wait-and-see approach was adopted due to the benign nature of this entity. The patient is currently being studied for high urea levels at a metabolic diseases department.
CommentWhite sponge nevus is a rare, autosomal dominant hereditary genodermatosis with variable penetrance, although sporadic cases have been reported. It was described by Hyde in 1909 with the name leukokeratosis and in 1935, Cannon coined the term white sponge nevus.
The pathophysiology is not fully understood. Mutations have been identified in the genes that code for keratins 3 and 14, located on chromosomes 12q13 and 17q21‐q22, respectively. These keratins are expressed specifically in the buccal, anogenital, nasal, esophageal, and laryngeal mucosa, and in other nonkeratinized stratified squamous epithelia.1–4
Lesions are asymptomatic in most cases and tend to involve the buccal mucosa bilaterally and symmetrically, in the form of white plaques with a rough, spongy appearance, which do not detach on scraping. Rare cases of isolated involvement of the extraoral mucosa have been reported.5 They may be congenital or appear during childhood, as in the case of our patient. They sometimes appear during adolescence and show no preference for sex.1,3,5,6
Histopathology is nonspecific. Of note is the epithelial thickening with parakeratotic hyperkeratosis, acanthosis, and spongiosis, with vacuolization of supra-epidermal keratinocytes and with perinuclear eosinophilic aggregates that correspond to anomalous groupings of keratin tonofilaments.1
Diagnosis is based on clinical signs and symptoms and on histopathology findings. A genetic study may also be performed.
Prognosis is good. Cases have been reported in the literature with subsequent development of dysplasia and even epidermoid carcinoma, although the link has not been clearly established.3,5
Treatment is not required, as the lesions are asymptomatic. Isolated cases of response to chlorhexidine, topical retinoids and topical tetracycline, and oral penicillin have been published.1,2,6
The differential diagnosis must be carried out with other diseases that involve white lesions in the buccal mucosa, such as genodermatosis (congenital pachyonychia, hereditary benign intraepithelial dyskeratosis, and congenital dyskeratosis), infections (oral candidiasis in its pseudomembranous form, focal epithelial hyperplasia, and syphilis), inflammatory diseases (lichen planus), premalignant and malignant lesions (leukoplasia, epidermoid carcinoma), and other entities such as leukoedema and friction hyperkeratosis.
We report a rare, extensive case of pediatric-onset white sponge nevus. Of note in our patient is the casual finding of high levels of urea and suspected underlying metabolic disease, a finding not reported to date. The link between the 2 entities has yet to be defined.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rojas Mora E, Kheadaoui R, Hernández-Núñez A, Placas blancas en cavidad oral. Actas Dermosifiliogr. 2020;111:255–256.