An 11-year-old boy of Algerian origin with no pathological history of interest was referred for the presence of asymptomatic facial lesions that had appeared 12 months earlier. He reported an increase in lesion number and size, but had not undergone any treatment. Neither his parents nor his siblings had a history of similar lesions.
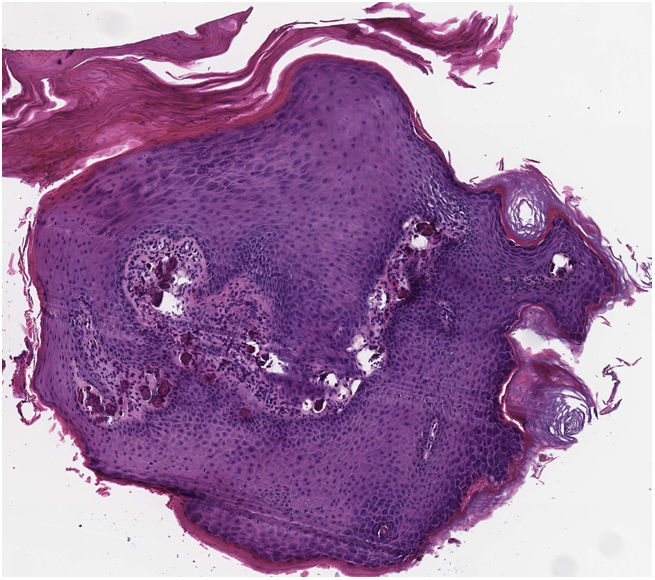
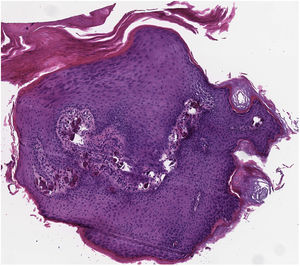
Physical examination revealed small (3–4mm in diameter), whitish, markedly indurated papules without central umbilication located on the chin and periocular area (Fig. 1). Polarized light dermoscopy showed rounded, whitish, shiny homogeneous structures, with no visible signs of vascularization (Fig. 2). Histological examination (hematoxylin–eosin) of a shave biopsy of one of the lesions confirmed the presence of extensive basophilic deposition in the mid-dermis surrounded by collagen fibers and accompanied by epidermal hyperplasia and parakeratosis (Fig. 3). Blood tests, including a metabolic and hormonal profile, revealed no abnormalities.
What Is Your Diagnosis?
DiagnosisMilia-like idiopathic calcinosis cutis
Diagnostic Process, Clinical Course, and TreatmentHistology revealed an amorphous crystalline basophilic deposit in the mid dermis, surrounded by collagen fibers. The surrounding tissue was unaffected. Calcium deposition was suspected and von Kossa staining was performed, revealing a blackish tone, which confirmed diagnosis of calcinosis cutis. Calcinosis cutis is defined as the deposition of calcium salts in the skin and subcutaneous tissue. Laboratory tests revealed normal serum levels of calcium, phosphorus, vitamin D, and parathyroid hormone. In the absence of any other underlying cutaneous or systemic disease, a definitive diagnosis of idiopathic calcinosis cutis was established. The patient underwent clinical observation and remains stable, with a similar number of lesions after 1 year of follow-up.
CommentCalcinosis cutis is classified into 5 categories according to pathophysiology: dystrophic, metastatic, idiopathic, iatrogenic and mixed.1 To confirm the idiopathic form, it is necessary to rule out underlying tissue lesions, which distinguish it from dystrophic calcification, as well as alterations in calcium and phosphorus metabolism typical of metastatic calcification.
Milia-like idiopathic calcinosis cutis is a benign and infrequent subtype (with only 32 cases reported in the literature) that was defined in 1978 and is described mainly in pediatric patients of both sexes (mean age, 12 y) with Down syndrome (62.5% of cases).2 However, isolated cases have also been described in adults3 and in patients without Down syndrome.4
The cause is unknown, although various hypotheses have been proposed, including persistent localized trauma,5 calcium precipitation in the acrosyringium secondary to increased sweat calcium levels, and calcium deposition in persistently inflamed epidermal cysts.
The clinical presentation is characterized by multiple, small, whitish, round firm papules, which usually appear on the hands and feet but can also affect other areas, and can infrequently develop on the face. Clinically, this condition can be easily confused with other entities, including molluscum contagiosum, viral warts, epidermal inclusion cysts, and syringomas. Although the definitive diagnosis is histological, a petaloid appearance on dermoscopy may be helpful,6 but this is not pathognomonic.
The condition is characterized by clustered white formations that lack vasculature, in contrast to molluscum contagiosum and viral warts.
These lesions tend to disappear spontaneously in adulthood without leaving scars, and therefore the most appropriate approach appears to be follow-up and observation. Other treatment alternatives include curettage and topical retinoids. Recognition and differentiation from other clinically similar entities is essential to avoid traumatic treatments that can exacerbate the lesions and promote their recurrence.
Conflicts of InterestThe authors declare that they have no conflicts of interest.