An 8-month-old boy consulted for a lesion on the right lower limb that had been present from birth. Since then, it had grown progressively, although its appearance remained unchanged. The patient’s medical history revealed no diseases of note. After a controlled pregnancy, he had been born at full term by caesarean section, without complications.
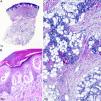
Physical ExaminationPhysical examination revealed 5 well-defined, dark red plaques, the largest of which was 1.5 cm long, that had irregular borders and were distributed between the medial malleolus and the dorsum of the right foot (Fig. 1A). Dermoscopy showed wine colored dots on a homogeneous pink background (Fig. 1B).
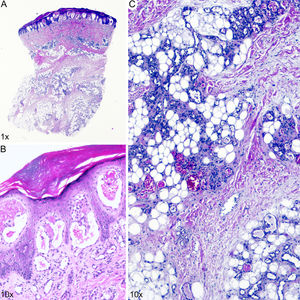
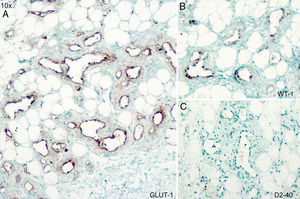
HistopathologyHistology showed an orthokeratotic epidermis with acanthosis and papillomatosis (Fig. 2A) and dilated vessels in a lobular pattern, surrounded by scant perivascular inflammatory infiltrate in the superficial and deep dermis (Fig. 2B and C). Immunohistochemical staining was positive for Wilms tumor 1 (WT1) and glucose transporter 1 (GLUT1) and negative for D2-40 (Fig. 3).
Additional TestsUltrasound showed that the lesions were superficial, and revealed a slight increase in soft tissue thickness in the medial dorsal region of the right foot, with no detectable flow. A complete laboratory work-up revealed no alterations in the hemogram, liver or kidney profile, or D-dimer levels.
What is Your Diagnosis?DiagnosisVerrucous venous malformation (VVM).
Clinical Course and TreatmentDaily topical treatment with 0.5% timolol was prescribed for 6 months, but was discontinued in the absence of any improvement.
CommentVVM is a vascular anomaly. There has been much discussion as to whether it constitutes a malformation or a tumor. The lesions, which are usually present at birth or appear in early childhood, consist of single or multiple dark red patches. These most frequently occur on the lower limbs, tend to darken, thicken, and become hyperkeratotic, and rarely undergo remission.1 VVM is characterized by compact hyperkeratosis of the epidermis and papillomatosis, irregular acanthosis, and dilated capillaries in the papillary and deep dermis and the subcutaneous cellular tissue.2 Although its clinical characteristics resemble those of a vascular malformation, it was initially considered a vascular tumor by the International Society for the Study of Vascular Anomalies due to its positive immunostaining for WT1 and GLUT1.2,3
Clinically, VVM can be confused with other vascular lesions, such as angiokeratoma, and with capillary, venous, and lymphatic vascular malformations that are negative for GLUT1 and WT1, despite displaying hyperkeratosis and acanthosis.3
Recently, Couto et al.4 described the presence in VVM tissue of a somatic missense mutation in mitogen-activated protein kinase kinase kinase 3, which is involved in the angiopoietin-1 and tunica intima endothelial cell kinase signaling cascade, and is implicated in both hereditary and sporadic venous malformations.5 Based on its clinical course and recent genetic findings, VVM is currently considered a venous malformation,6 despite its immunohistochemical characteristics.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Villegas-Romero I, Tello-Collantes K, Jiménez-Gallo D. Placas eritematovioláceas en miembro inferior. Actas Dermosifiliogr. 2020;111:861–862.