A 43-year-old man with androgenetic alopecia consulted for blistering lesions and erosions of 6 months’ duration on the scalp. The lesions were asymptomatic or slightly pruritic and tended to recur, although they never disappeared completely. The only trauma to the area reported by the patient was the use of a safety helmet at work for the previous 5 years.
Physical ExaminationPhysical examination revealed vesiculobullous lesions, erosions, and crusting, located mainly in the parietal areas of the scalp. Some of the lesions had left shiny atrophic skin with a scar-like appearance (Fig. 1). No other skin or mucosal lesions were observed.
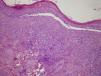
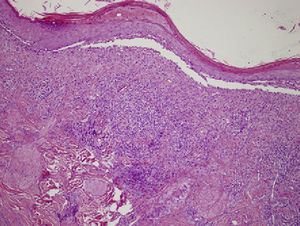
HistopathologyAn incisional biopsy was performed on the edge of a blistering lesion. Histopathology showed dermal-epidermal separation and subepidermal blisters containing fibrinoid material, lymphocytes, and eosinophils. In the dermis, there was an area with a scar-like appearance, together with an interstitial inflammatory infiltrate consisting of lymphocytes and a marked presence of eosinophils (Fig. 2).
Additional TestsDirect immunofluorescence of a perilesional biopsy specimen showed strong linear deposition of immunoglobulin (Ig) G, IgA, and C3 and weaker deposition of IgM (Fig. 3). Bacterial and viral cultures of exudate were negative.
What Is Your Diagnosis?
DiagnosisLocalized cicatricial pemphigoid (Brunsting–Perry variety)
Clinical Course and TreatmentA complete blood count with erythrocyte sedimentation rate, a full biochemical workup, thyroid stimulating hormone levels, and a protein profile was requested, with normal results in all cases. Antinuclear antibodies, anti-basement membrane autoantibodies, and intercellular substance antibodies were negative.
Topical treatment was initiated with once-daily clobetasol propionate 0.05% and resulted in a clear improvement in the lesions within 2 weeks; satisfactory control was subsequently achieved with the application of clobetasol propionate 0.05% once or twice a week. In a year of follow-up, the patient has not developed any mucosal lesions or skin lesions at other sites.
CommentCicatricial pemphigoid, which has also recently been named mucous membrane pemphigoid, constitutes a diverse group of blistering diseases that mainly affect the mucous membranes, although, they can occasionally affect the skin.1 The condition is mediated by autoantibodies directed against proteins at the dermal-epidermal junction, resulting in the formation of subepidermal blisters. Localized cicatricial pemphigoid tends to be confined to the head and neck, and skin lesions can precede mucosal lesions by months or even years.2 Brunsting–Perry pemphigoid, a variant of this condition described by Brunsting and Perry3 in 1957, tends to affect men between 40 and 70 years of age and is characterized by blistering lesions and recurrent erosions on the head and neck that leave scars when they clear. Unlike other variants of localized cicatricial pemphigoid, Brunsting–Perry pemphigoid does not tend to affect the mucous membranes. It has been reported to occur following trauma to the affected area.4 In our patient, the continued trauma to the scalp caused by the use of a safety helmet for 5 years might have triggered the lesions. Histologically, Brunsting–Perry pemphigoid is characterized by subepidermal blistering and a chronic inflammatory infiltrate rich in eosinophils. In most cases, direct immunofluorescence shows linear IgG and complement deposition, occasionally in association with IgA or IgM deposits. Indirect immunofluorescence tests, on the other hand, tend to be negative, as was the case with our patient.
The differential diagnosis should include erosive pustular dermatosis of the scalp, giant cell arteritis, epidermolysis bullosa acquisita, dermatitis artefacta, and infections.5
The treatments of choice for Brunsting-Perry cicatricial pemphigus are intralesional or topical corticosteroids, although dapsone, sulfapyridine, and minocycline have also proven effective. Finally, refractory or extensive disease can be treated with oral corticosteroids or other immunosuppressants.
B. García-García, S. Mallo-García, B. Vivanco-Allende. Lesiones vesiculosas y erosivas en el cuero cabelludo. Actas Dermosifiliogr. 2012;103:541-2.