The appearance of multiple satellite lesions is a rare complication of the treatment of a primary pyogenic granuloma lesion. We report 5 cases of recurrent pyogenic granuloma in patients aged between 4 and 31 years. The lesions resolved spontaneously after 1 to 9 months. Although the diagnosis and treatment of recurrent pyogenic granuloma can be problematic, this condition is benign and frequently self-limiting.
El desarrollo de múltiples lesiones satélite de granuloma piogénico tras el tratamiento de la lesión primaria es un trastorno poco frecuente. Comunicamos 5 casos de granuloma piogénico recidivante en pacientes con edades comprendidas entre los 4 y los 31 años, con lesiones que se resolvieron espontáneamente al cabo de 1-9 meses. Aunque puede plantear problemas diagnósticos y terapéuticos, es una entidad benigna y con frecuencia autolimitada.
Pyogenic granuloma is a very common vascular proliferation that usually presents as a solitary, sessile, or pedunculated lesion with a fragile surface prone to bleeding, ulceration, and crusting. Local recurrence after treatment is very common. However, the appearance of multiple satellite lesions after excision of the initial lesion is a rare complication of pyogenic granuloma and can present problems of diagnosis and management. Such lesions, known as recurrent pyogenic granuloma (RPG), were described by Warner and Wilson Jones in 1968.1 We present 5 cases of RPG, most of which are in pediatric patients.
Case DescriptionWe performed a retrospective study that identified 5 patients who had been diagnosed with pyogenic granuloma in the Dermatology Department of Hospital General de Valencia, Spain, and had subsequently developed satellite angiomatous lesions. Photographs of the recurrent lesions, histopathology, and a detailed history of the development of the lesions were assessed. The patients were 3 females and 2 males (Table 1) aged 4 to 31 years (mean, 13 y). The lesions were located on the trunk or thighs and appeared after the initial treatment for pyogenic granuloma by surgical excision or electrodessication (Figs. 1 and 2). The time from initial treatment to the appearance of RPG ranged from 1 to 9 months (mean, 3 mo). In all cases the RPG lesions disappeared spontaneously, beginning to regress after 45 to 120 days (mean, 81 d).
Demographic Characteristics of Patients With the Site and Clinical Course of Recurrent Pyogenic Granulomas.
| Age, y | Sex | Site | Treatment of Primary PG | Latency Period, mo | Clinical Course |
| 9 | Male | Scapula | Surgical excision | 1 | Regression at 45 d |
| 15 | Female | Thigh | Electrodessication | 9 | Regression at 2 mo |
| 6 | Female | Abdomen | Surgical excision | 3 | Regression at 2 mo |
| 31 | Male | Thigh | Surgical excision | 1 | Regression at 4 mo |
| 4 | Female | Clavicle | Surgical excision | 1 | Regression at 4 mo |
PG, pyogenic granuloma.
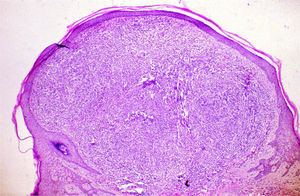
Biopsies of the recurrent lesions revealed typical findings of pyogenic granuloma. The dermis was occupied by lobes of prominent endothelial cells with formation of small vascular spaces. The endothelial cells showed no atypia and no inflammation. The lesion was surrounded by an epidermal collarette (Fig. 3).
DiscussionRPG is a rare and therefore little-known disease. It is mainly found in males under the age of 25 years. Interestingly, RPG lesions do not appear in the places where pyogenic granuloma lesions often appear, such as the hands, face, nasal mucosa, gums, and lips.2 The main site of multiple recurrent lesions is the trunk, particularly the interscapular region.1,3,4 Most satellite lesions appear between 1 week and 4 months after treatment of the primary tumor but they can occur up to 2 years after treatment.5,6 In rare cases there can be a second recurrence after treatment of the RPG lesions.7 The satellite lesions tend to be asymptomatic, bright red, sessile papules of 1 to 10mm diameter with the surface intact.
Possible predisposing factors for the appearance of pyogenic granulomas are trauma, chronic irritation, infections, viral oncogenes, and microscopic arteriovenous anastomosis.2 The pathogenesis of satellite metastasis is not well known. It has been suggested that after treatment of the primary lesion angiogenic factors may promote the appearance of new lesions. However, the risk of recurrent lesions does not appear to be related to the treatment method used for the initial tumor because this condition has been described after surgical excision, cautery, carbon dioxide laser excision, ligation, and curettage.8 It has also been observed following irritation of the primary lesion.3,9 In 1 case Bartonella henselae was identified in lesions of an immunocompetent man, leading the authors of that case report to suggest that RPG might be a localized variant of bacillary angiomatosis,10 although this hypothesis has not been confirmed in subsequent case reports.
Histological findings in RPG are identical to those of any other variant of pyogenic granuloma, with the exception that smaller recurrent lesions are very similar to capillary hemangiomas.1 Initially they are identical to granulation tissue, with numerous capillaries and venules distributed radially to the skin surface in edematous stroma with mixed inflammatory infiltrate. In more advanced stages, fibrous septa partition the lesion into lobules composed of aggregates of capillaries and venules with prominent endothelial cells but no stromal edema and little inflammatory infiltration. Finally, fibroplasia replaces the lobules of capillaries until the lesion transforms into a fibroma.11 In a few cases of recurrent lesions, anastomosing vascular channels dissect collagen bundles, especially in the deep areas, with an appearance similar to angiosarcoma.1,12 The ultrastructural study also fails to distinguish the endothelial cells of the recurrent lesions from simple pyogenic granuloma.13
A conservative approach is an appropriate option, because most untreated recurrent lesions disappear spontaneously in 6 to 12 months.13 When treatment is prescribed, the same methods as those of simple pyogenic granuloma are used. The treatments include Nd:YAG laser,14 topical imiquimod,15 and intralesional bleomycin,16 in addition to systemic corticosteroids for giant lesions in the proliferative phase.17
We have reported 5 cases of RPG, the largest series after the initial description by Warner and Jones.1 Our observations are in agreement with the finding that the lesions appear in young people, even in children, and are mainly located on the trunk and limbs around the scar from treatment of the primary lesion. Histopathology is necessary to confirm the diagnosis. In all cases the lesions disappeared completely without treatment, so we recommend a conservative approach. It is important to identify RPG because the appearance of satellite lesions after treatment of a tumor disease can be a concern for physicians who are not familiar with this condition.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pitarch G, Pérez-Ferriols A, Millán F. Granuloma piogénico recidivante. Actas Dermosifiliogr.2012;103: 536-539.