Thymoma is the most common primary tumor of the anterior mediastinum. Symptoms are due to compression by the tumor or to various paraneoplastic syndromes. However, 50% of patients are asymptomatic at the time of diagnosis.1 We describe the case of a patient who developed pruritus and telangiectasias on the trunk as the initial signs of a malignant thymoma.
The patient was a 78-year-old man who was seen in outpatients for the progressive appearance of telangiectasias on the skin of the anterior chest wall over the previous 3 months. He reported that he had previously had a skin rash in the area but that it had resolved by the time of consultation. The patient complained of intense pruritus and malaise that even affected nighttime rest.
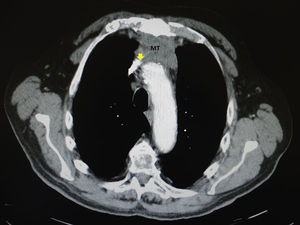
He did not report chest pain or respiratory difficulty. His past history included a bladder tumor that was in remission. A chest x-ray and abdominal ultrasound performed 2 years earlier had shown no alterations. Physical examination revealed telangiectasias in a vertical distribution, most prominent on the left hemithorax, with no other changes and no other dilated, larger caliber vessels (Figs. 1 and 2). There were no relevant findings on examination of the face and neck and no palpable masses or lymph nodes. In view of the intensity of the symptoms reported by the patient, cervical and thoracic computed tomography (CT) was requested to rule out an underlying lesion. The CT revealed a retrosternal mass of 5×2.5cm with enlarged perilesional and pericardial lymph nodes and compression of the superior vena cava (Fig. 3). The differential diagnosis included teratoma, lymphoma, and thymoma. The patient did not report weight loss or night sweats, and his general state of health was normal. Cytology from a fine-needle aspiration biopsy was compatible with thymoma. The patient was evaluated by the thoracic surgeons and the tumor was considered inoperable. The final diagnosis was malignant sclerosing thymoma. Studies of tumor spread excluded metastatic disease and there were no symptoms of paraneoplastic syndromes, such as myasthenia gravis. The patient started combined treatment with adriamycin and radiation therapy with a partial regression of the mass. The telangiectases did not vary, but the pruritus reported by the patient resolved with the treatment.
Thymoma is the most common tumor of the anterosuperior mediastinum. It typically starts in the midline and spreads unilaterally. Symptoms described by patients with thymoma can be due to the mass effect, such as chest pain, respiratory difficulty, cough, or superior vena cava syndrome.1–3 This syndrome occurs when venous return from the upper part of the body is obstructed. One of the earliest and most prominent signs of this syndrome is the appearance of numerous vertically orientated, dilated and tortuous capillaries and venules.4 Other typical signs of superior vena cava syndrome are edema of the face and of the upper limbs, cyanosis, and visual changes due to papilledema. Bruno et al.5 published a case caused by lymphoma in which the patient also presented a transient skin rash and telangiectases. Other causes of telangiectases on the chest wall are chronic actinic damage and poikiloderma, essential telangiectasia, connective tissue diseases such as lupus, dermatomyositis or scleroderma, hyperestrogenic states such as cirrhosis and pregnancy, and malignant causes such as intravascular B-cell lymphoma or skin metastases.
Other manifestations in patients with thymoma include a high prevalence of infections and immunological disturbances.6 Myasthenia gravis develops in at least 30% of patients.7 There have also been cases of red cell aplasia, hypogammaglobulinemia, endocrine disturbances, chronic mucocutaneous candidiasis, connective tissue diseases such as lupus or dermatomyositis, and paraneoplastic pemphigus.8
Surgery is the treatment of choice. Patients with advanced invasive thymoma require treatment with radiation therapy and chemotherapy.3 Cases have been seen of invasive thymoma affecting the pleura and lung, thoracic vertebrae, thyroid gland, central nervous system, liver, extrathoracic lymph nodes, and overlying dermis.9
At no time did our patient present extracutaneous symptoms, and it was the skin manifestations that led to the diagnosis of his serious underlying disease. Thus, in a patient with intense pruritus on the chest with no causative skin lesions and/or vertically oriented telangiectasias of rapid onset, we must exclude an intrathoracic space-occupying lesion.
Please cite this article as: Laguna C. Telangiectasias verticalizadas y prurito en el tórax en un paciente con síndrome de cava superior inicial secundario a un timoma maligno. Actas Dermosifiliogr. 2015;106:331–332.