A 34-year-old, homosexual male patient with a history of infection with human immunodeficiency virus (HIV), disseminated tuberculosis, Salmonella infectious diarrhea, herpes zoster and neurosyphilis presented to our dermatology clinic with a 3-week history of painful perianal nodules. At first, he had been taking 250mg of oral cephalexin four times a day and using topical chloramphenicol ointment for several weeks without improvement. He had been under treatment with antiretroviral therapy regularly: 600mg of efavirenz daily and one tablet of lamivudine/zidovudine twice daily for HIV for seven years.
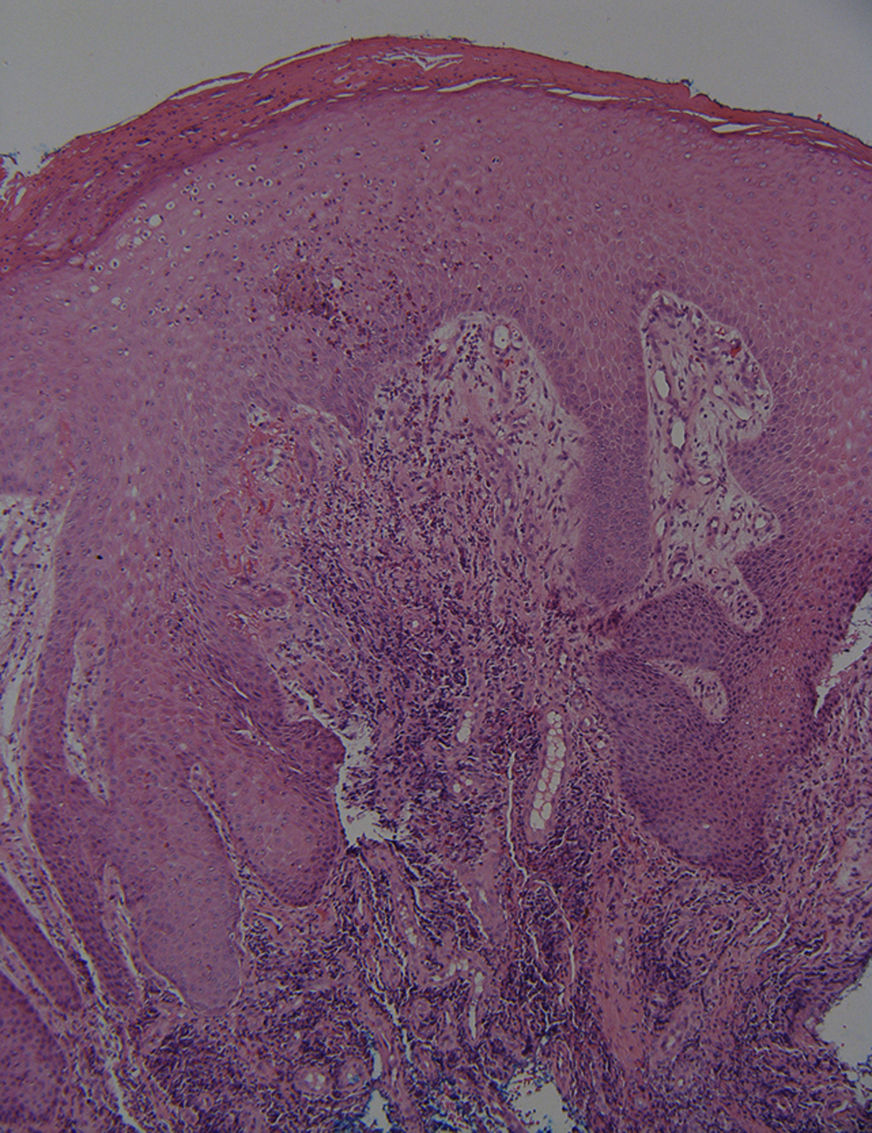
Physical examinationPhysical examination showed two painful, 1-cm wide, erythematous nodules in the perianal area (Fig. 1). The nodules were hard with superficial ulceration and much discharge.
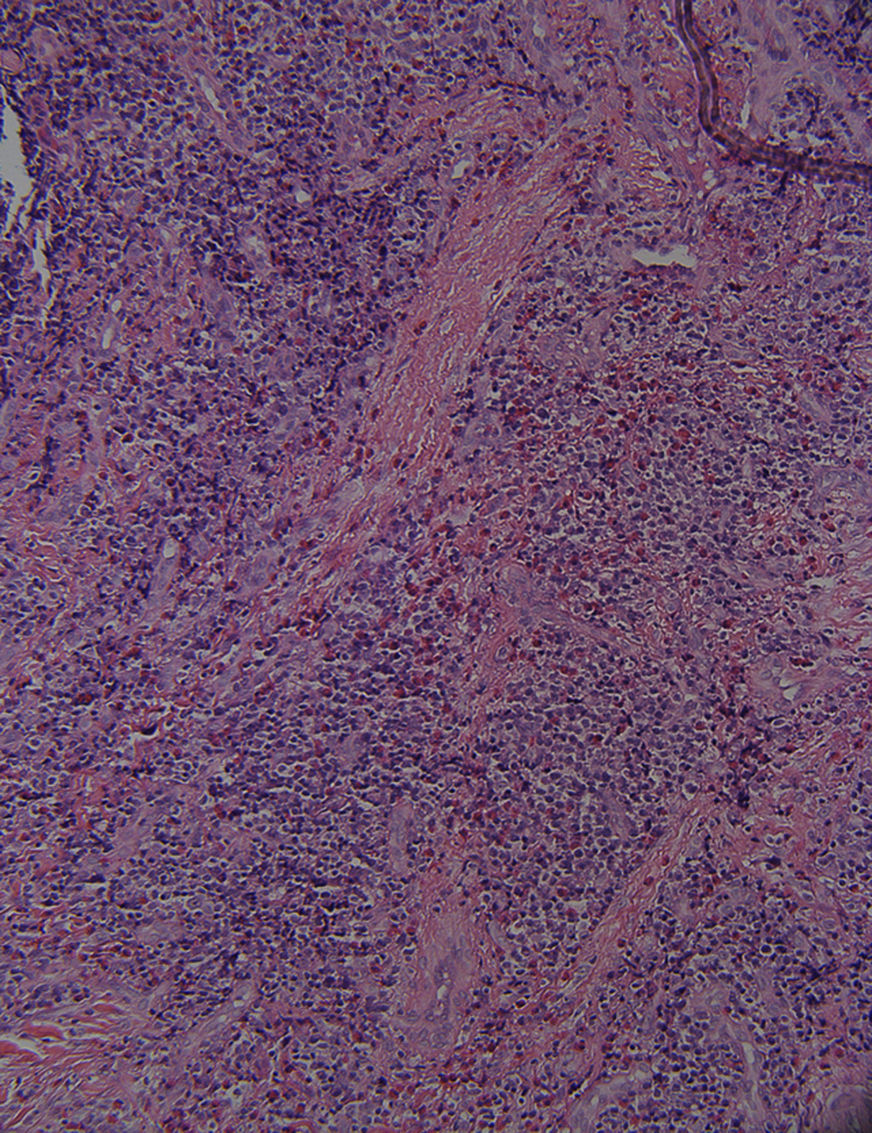
HistopathologyA punch biopsy of a nodule in the perianal area was performed. Hematoxylin–eosin staining showed pseudoepitheliomatous hyperplasia with exocytosis and parakeratosis (Fig. 2). In the dermis, acute and chronic inflammation with mixed lymphohistiocytes, eosinophils, neutrophils and plasma cells were noticed (Fig. 3).
Additional testsHis latest CD4 count, measured one month prior to the development of ulcerative nodules, was 427/μL (normal range: 500–1500/μL). The spirochete immunostain and periodic acid-Schiff stain were both negative. Moreover, the venereal disease research laboratory test showed 1:1 (weakly reactive), and viral isolation by culture from the tissue specimen was positive for herpes simplex type 2 (HSV-2).
What is your diagnosis?
DiagnosisNodular perianal herpes simplex.
Clinical course and treatmentAfter diagnosis with herpes simplex, he was treated with 1g of valcyclovir twice daily for two subsequent months with the nearly complete resolution of the cutaneous lesions.
CommentHIV-positive patients have high rates of HSV-2 infection, ranging from 50% to 90% in different studies.1 The relationship between genital HSV-2 and HIV has been termed a syndemic. Genital HSV-2 infection is the leading cause of genital ulcers worldwide, particularly in immunocompromised patients. However, the clinical presentations of genital HSV-2 infection in HIV are variable.2
Clinical manifestations of HSV-2 in HIV include nodular, hypertrophic, tumor-like, vegetative or ulcerative growths simulating neoplasms. It has been suggested that an overstimulated inflammatory response that follows immune restoration after highly active antiretroviral therapy (HAART) initiation could be responsible for nodular and vegetative presentations of genital herpes infection.3 However, our patient developed nodular HSV lesions seven years after HAART initiation, in marked contrast to what most studies have reported.
The nodular HSV lesions were of atypical morphology and mimicked other opportunistic infections such as syphilis, molluscum contagiosum, Kaposi sarcoma, and other lymphoproliferative tumors. Thus, biopsy was often necessary for correct diagnosis. Because HIV-positive individuals are also at higher risk of developing anogenital malignancies and lymphomas, when an HIV-infected individual presents with a nodular mass that lacks the characteristic clinical and histopathological features of herpes, HSV is often overlooked and the concern for lymphoma or anogenital malignancies rises.
Histopathologically, features of herpes generally show a dense chronic inflammatory infiltrate composed mainly of plasma cells mixed with eosinophils and lymphocytes. Typically, there are also multinucleated giant cells with steel-gray molded nuclei, ground-glass chromatin, and acantholytic keratinocytes.4 Nonetheless, the histology may fail to show typical viral inclusion bodies or multinucleated giant cells, and HSV cultures are often negative. Polymerase chain reaction and immunohistochemistry may be necessary to detect the virus.5 Our case showed a large number of plasma cells mixed with eosinophils and lymphocytes in the dermis, and viral isolation by culture from the tissue specimen was positive for HSV-2.
In previous studies, most cases of HSV in HIV-positive patients have presented with a prolonged clinical course of disease and only a few were rapidly growing masses. The present case showed a relatively rapid growth of only three weeks duration. Two 1-cm painful nodules exhibited superficial ulceration.
Treatment of atypical HSV infection in HIV-positive individuals requires a high-dose and long-term therapy with acyclovir.6 Antiviral therapies are effective and safe for suppressive and episodic treatment of HSV in HIV-positive patients.
Conflict of interestThe authors declare that they have no conflicts of interest.