Although the gold standard for the study of skull anomalies is X-rays on two planes, limited availability in outpatient settings and the radiation inherent to X-ray image acquisition have prompted the use of alternative non-radiation imaging techniques with pediatric patients, such as ultrasonography.1
Furthermore, some subcutaneous pseudotumors, especially in the head and neck region, are not actually skin tumors but alterations of bony surface. Such is the case of external occipital protuberance (EOP), which may present painful exostosis in adolescence.
Two males aged 14 and 15 years old, respectively, were referred to the Dermatology Clinic with suspected tumors at the occipital level, which had presented slow but steady growth in recent years and were causing slight discomfort in the supine position. In both cases, a hard protuberance was felt in the referred zone. One of the cases had previously been diagnosed as pilomatricoma.
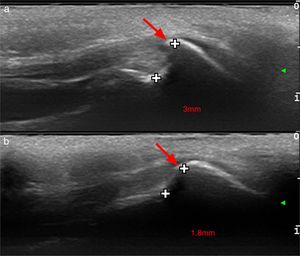
An ultrasound examination was performed using a high frequency linear probe, in which no dermal or subcutaneous cellular tissue alterations were evident. However, a spine or hook shaped bony protuberance was observed on the surface of the occipital bone, contiguous with the insertion of the cervical musculature, separated from the bone table by 3mm in the first case (Fig. 1a) and 1.8mm in the second (Fig. 1b).
High frequency ultrasound of patients showing longitudinal scan of the occipital area. Type 3 or spine type external occipital protuberance is marked with an arrow and distance between the occipital bone and the exostosis is measured in millimeters. We can also observe the upward displacement of the adjacent musculoaponeurotic layers, constituted by the nuchal ligament, insertion fibers of the trapezius muscle and the epicranial aponeurosis.
Diagnosis of type 3 or spine type EOP was made, and as the lesion was almost asymptomatic, conservative follow-up was indicated.
External occipital protuberance has been widely reported in the anthropological literature, but there is a paucity of information on it in medical publications. Broca classified EOP into six anatomical subtypes which Gülekon and Turgut subsequently simplified into three subtypes2: smooth form (type 1), crest type (type 2) and spine type (type 3).
Type 3 EOP is an anatomical skull variant reported in 63.4% of males and 4.2% of females, and is a sex marker in forensic and anthropological studies (Fig. 2). However, EOP can become symptomatic in predisposed individuals in late adolescence due to a focal bony exostosis, possibly related to growth of the neck muscles that are inserted in it, mainly the trapezius muscle. This increases in size, causing subperiosteal stretching and tenderness in the area, especially on pressure palpation.
Apart from a sonographic report by Nevo and Brohnstein3 on transient protuberances of the occipital bone in fetuses as a differential diagnosis of encephalocele, most studies of this anatomical variation have been based on ionizing radiation diagnostic tests such as X-rays or CTscans.
As demonstrated by these clinical cases, ultrasonography enables quick, direct diagnosis of this condition and rules out other dermal or subcutaneous skin tumors, such as calcified cephalohematoma (mainly in newborns and young children) or pilomatricoma (both in children and adults) among others.4,5 Consequently, dermatologists are making increasing use of this technique, avoiding unnecessary biopsies or ionizing explorations.6
The incidence of symptomatic EOP is unknown, and its management is based on analgesia. However, limited surgical resection and bony smoothing can provide a long term solution in resistant cases, as reported by Marshall et al.7 Ultrasonography is a valid diagnostic method for EOP which is easily available to dermatologists and has the potential to avoid unnecessary ionizing explorations and surgery.
Please cite this article as: Gómez Zubiaur A, Alfageme F, López-Negrete E, Roustan G. Type 3 External Occipital Protuberance (Spine Type): Ultrasonographic Diagnosis of an Uncommon Cause of Subcutaneous Scalp Pseudotumor in Adolescents Eczema y urticaria en Portugal. 2019;110:774–775.